Admittedly there's a research gap concerning face shields since they are mainly intended for hospital settings, hence scenarios limited to hospital settings. The general consensus is that face shields are intended for ballistic droplets, not for aerosols.
Below are the studies:
Below are the studies:
Lindsley et al. (2014). Efficacy of Face Shields Against Cough Aerosol Droplets from a Cough Simulator
Face shields are evaluated to stop the initial impact of the cough which brought heavy droplets, however, airborne droplets still make way around.
ncbi.nlm.nih.gov/pmc/articles/P…
Face shields are evaluated to stop the initial impact of the cough which brought heavy droplets, however, airborne droplets still make way around.
ncbi.nlm.nih.gov/pmc/articles/P…

Akagi et al. (2020). Effect of sneezing on the flow around a face shield. Phys. Fluids 32. doi:10.1063/5.0031150
A numerical simulation of a sneeze on a face shield, showing that transient effects actually directs aerosols inside even during impact.
aip.scitation.org/doi/10.1063/5.…
A numerical simulation of a sneeze on a face shield, showing that transient effects actually directs aerosols inside even during impact.
aip.scitation.org/doi/10.1063/5.…

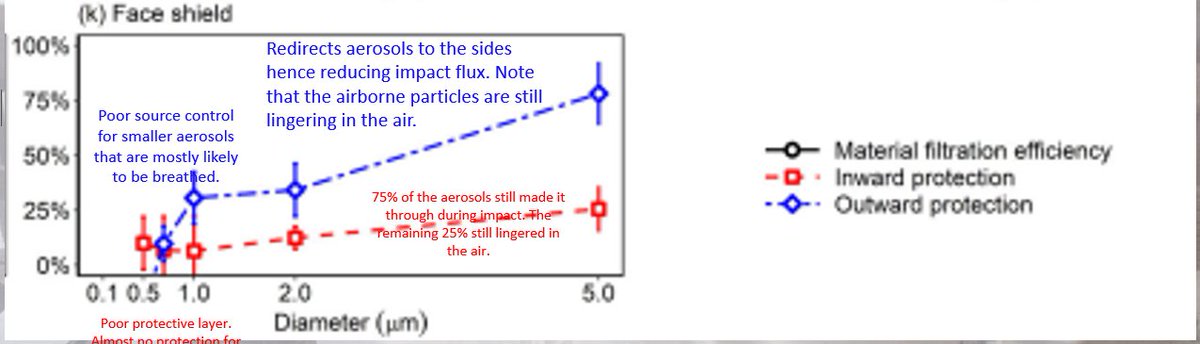
Pan et al. (2021) Inward and outward effectiveness of cloth masks, a surgical mask, and a face shield, Aerosol Science and Technology, 55:6, 718-733, DOI: 10.1080/02786826.2021.1890687
Face shields are rated as the poorest protective layers.
medrxiv.org/content/10.110…

Face shields are rated as the poorest protective layers.
medrxiv.org/content/10.110…

Salimnia et al. (2021). A laboratory model demonstrating the protective effects of surgical masks, face shields, and a combination of both in a speaking simulation
An experimental study evaluating little to no contribution of face shield.
pubmed.ncbi.nlm.nih.gov/33485923/
An experimental study evaluating little to no contribution of face shield.
pubmed.ncbi.nlm.nih.gov/33485923/

Bagtasa (2021). Efficacy of face shields to ambient aerosols in local indoor and outdoor setting. 2021: Proceedings of the 39th Samahang Pisika ng Pilipinas Physics Conference
Evaluating that face masks are the ones doing the work, not face shields.
proceedings.spp-online.org/article/view/S…
Evaluating that face masks are the ones doing the work, not face shields.
proceedings.spp-online.org/article/view/S…

Wendling et al. (2021) Experimental Efficacy of Face Shield and the Mask against Emitted and Potentially Received Particles, J. Environmental Research and Public Health
One of the flawed studies conducted by medical professionals. Fails on equipoise.
pubmed.ncbi.nlm.nih.gov/33671300/
One of the flawed studies conducted by medical professionals. Fails on equipoise.
pubmed.ncbi.nlm.nih.gov/33671300/

A visualization of TU Delft shows what happens to the emissions in the first place when the face masks are interfering:


If the face mask are already directing the emissions to the sides and the back instead to the front, what's the use of Wendling's setup? 

Verma et al. (2020). Visualizing droplet dispersal for face shields and masks with exhalation valves
A visualization experiment by the Florida Atlantic University showing that face shields are poor source control... They don't stop aerosols at all.
aip.scitation.org/doi/10.1063/5.…
A visualization experiment by the Florida Atlantic University showing that face shields are poor source control... They don't stop aerosols at all.
aip.scitation.org/doi/10.1063/5.…

Most of these studies were derived from hospital settings, therefore they perceived sporadic (i.e. cough, sneezes, speaking) emissions as the high risk scenarios, and focused only for that scenario.
Here is what happens at different angles of approach:
Here is what happens at different angles of approach:
https://twitter.com/JoshuaCAgar/status/1438734560737431552?s=20
If the cough is coming from behind, the wearer of the face shield is practically screwed:
https://twitter.com/JoshuaCAgar/status/1478636752789118980?s=20
Here is what happens when you walk in an indoor space (close spaces, crowded places) saturated with airborne particles while donning a face shield:
https://twitter.com/JoshuaCAgar/status/1478034845146447874?s=20
Faster accumulation of airborne particles if you're looking side-to-side while walking:
https://twitter.com/JoshuaCAgar/status/1479209331337822209?s=20
A face shield provide a place for retention of airborne particles:
https://twitter.com/JoshuaCAgar/status/1479430742488719368?s=20
If there's wind potentially carrying SARS-CoV-2 coming from behind:
https://twitter.com/JoshuaCAgar/status/1479651469637079042?s=20
Similar scenario, only at an oblique angle:
https://twitter.com/JoshuaCAgar/status/1479669884367761408?s=20
As Dr. Jimenez has said, face shields are useless against Covid-19, now that the understanding that it is airborne. When face shields are coupled with face masks, face masks are the ones doing the work while face shields do nothing.
https://twitter.com/ANCALERTS/status/1479265266936778752?s=20
There are in-fact, other atmospheric consequences of face shields that lead to the increase in infectivity of SARS-CoV-2.
This is the extended abstract of the conference paper that I'll be presenting two weeks from now.
This is the extended abstract of the conference paper that I'll be presenting two weeks from now.

If one insist on doing RCTs on face shields in public settings, despite these studies and despite the fact that face shields are physical items, not medicine, maybe for truthfulness sake, include the Pontresina Case
thelocal.ch/20200715/only-…
thelocal.ch/20200715/only-…

• • •
Missing some Tweet in this thread? You can try to
force a refresh


















