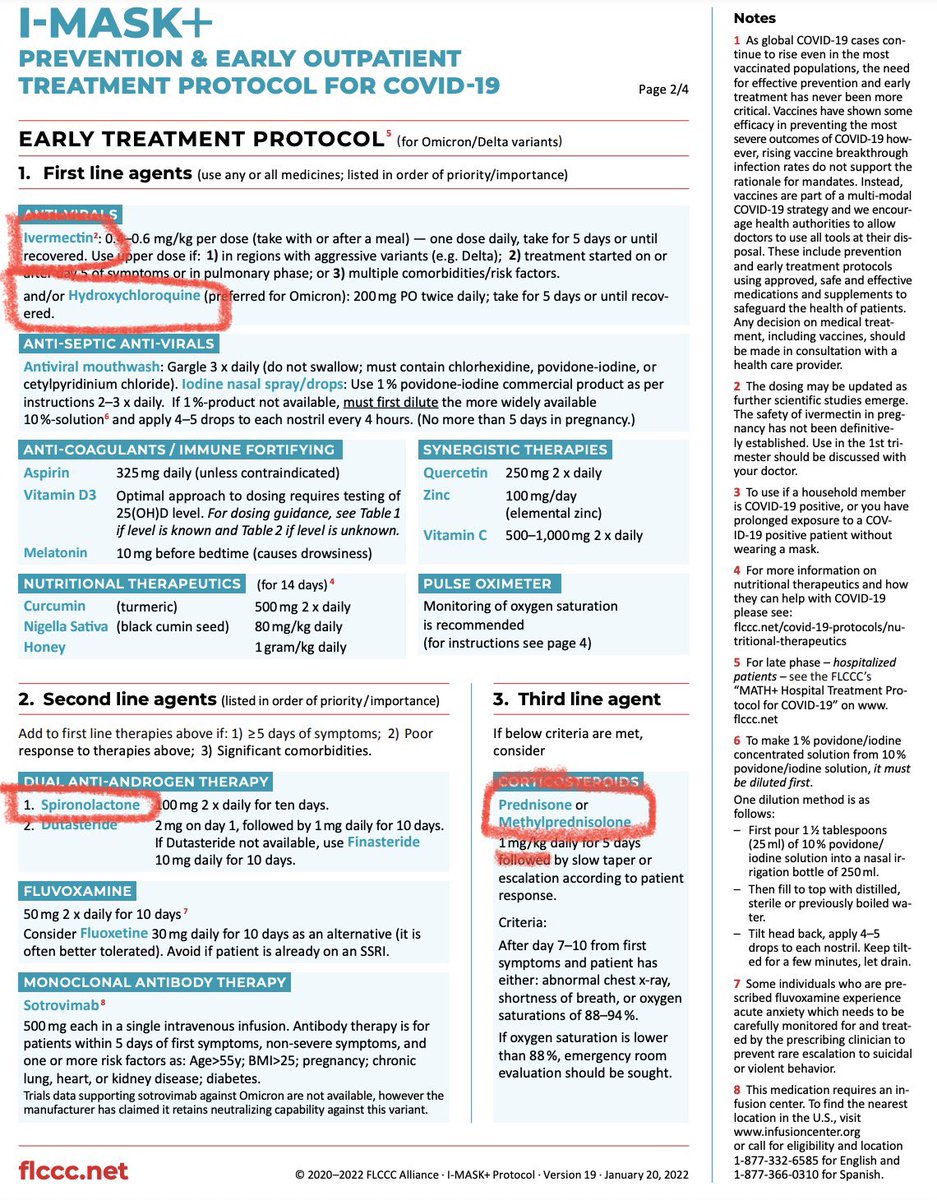
The ivermectin crazies are now recommending hydroxychloroquine too.
Their “protocol” includes a dangerously high dose of diuretics & recommends high dose steroids in people not on supplemental O2.
This has crossed the line from (mostly) harmless nonsense to actual harm.
Their “protocol” includes a dangerously high dose of diuretics & recommends high dose steroids in people not on supplemental O2.
This has crossed the line from (mostly) harmless nonsense to actual harm.
Supporting Evidence:
A 2021 Cochrane meta-analysis (the 🥇standard) concluded that HCQ “has little or no effect on the risk of death and probably no effect on progression to mechanical ventilation. Adverse events are tripled compared to placebo…”
cochranelibrary.com/content?templa…
A 2021 Cochrane meta-analysis (the 🥇standard) concluded that HCQ “has little or no effect on the risk of death and probably no effect on progression to mechanical ventilation. Adverse events are tripled compared to placebo…”
cochranelibrary.com/content?templa…

A more recent meta-analysis in @NatureComms that included unpublished studies went further, concluding “that treatment with hydroxychloroquine is associated with increased mortality in COVID-19 patients”
nature.com/articles/s4146…
nature.com/articles/s4146…

Regarding steroids:
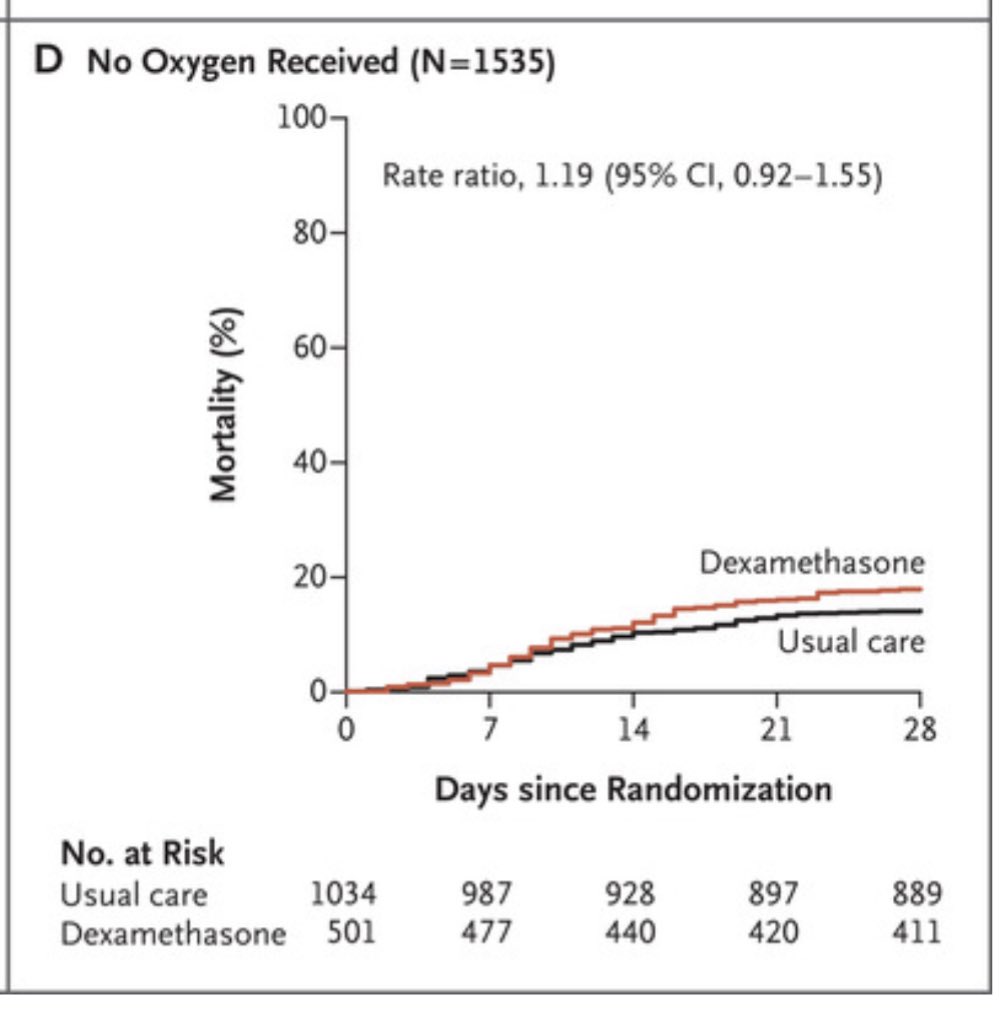
The UK RECOVERY trial found that among hospitalized inpatients w/ COVID, dexamethasone 6 mg PO/IV reduced mortality
They also found a HARM signal among people NOT on supplemental Oxygen. That’s why we ONLY use Dex in inpatients on O2!
nejm.org/doi/full/10.10…



The UK RECOVERY trial found that among hospitalized inpatients w/ COVID, dexamethasone 6 mg PO/IV reduced mortality
They also found a HARM signal among people NOT on supplemental Oxygen. That’s why we ONLY use Dex in inpatients on O2!
nejm.org/doi/full/10.10…



A Cochrane MA concluded “there is no evidence for [steroids in] asymptomatic or mild disease (non-hospitalised participants)”
pubmed.ncbi.nlm.nih.gov/34396514/
pubmed.ncbi.nlm.nih.gov/34396514/
Another MA examined steroids in people not on O2 & found INCREASED duration of fever, DELAYED time to viral clearance, & LONGER hospital length of stay, concluding “steroids in non-O2 requiring COVID-19 patients can be more detrimental than beneficial.”
pubmed.ncbi.nlm.nih.gov/34347106/
pubmed.ncbi.nlm.nih.gov/34347106/
The spironolactone label shows a big potential harm: hyperkalemia
The recommended starting dose is lower & checking serum K+ levels is advised.
Caution is advised in people taking ACEi, NSAIDS, & other meds.
The “protocol” doesn’t mention any of this!
accessdata.fda.gov/drugsatfda_doc…

The recommended starting dose is lower & checking serum K+ levels is advised.
Caution is advised in people taking ACEi, NSAIDS, & other meds.
The “protocol” doesn’t mention any of this!
accessdata.fda.gov/drugsatfda_doc…


Bottom line: several aspects of FLCCC’s new I-MASK+ protocol are potentially very dangerous.
This is way worse than just presenting ivermectin as a “vaccine alternative.”
Based on the evidence & clinical practice guidelines, these recommendations are likely to cause real harm.
This is way worse than just presenting ivermectin as a “vaccine alternative.”
Based on the evidence & clinical practice guidelines, these recommendations are likely to cause real harm.

To put it another way:
If a person died while being treated with these meds (especially if they died from an arrhythmia), I would list the “I-MASK” protocol as a contributing factor.
It is truly malpractice to encourage this. Medical boards take notice. @ABIMFoundation @TheFSMB
If a person died while being treated with these meds (especially if they died from an arrhythmia), I would list the “I-MASK” protocol as a contributing factor.
It is truly malpractice to encourage this. Medical boards take notice. @ABIMFoundation @TheFSMB
• • •
Missing some Tweet in this thread? You can try to
force a refresh
































