In confronting COVID misinformation I’ve mostly focused on inpatient treatment (this is my area of experience).
Recently I saw the FLCCC Long COVID “protocol” & oh boy is this some crazy non-evidence based prescriptions: HIV meds, steroids, diuretics, & of course ivermectin…
1/
Recently I saw the FLCCC Long COVID “protocol” & oh boy is this some crazy non-evidence based prescriptions: HIV meds, steroids, diuretics, & of course ivermectin…
1/

First off, Long COVID is definitely “real” & can be severe.
Many studies have found persistent changes in immune cell phenotype & function, months after COVID infection.
Many great docs (@WesElyMD & others) are actively researching long COVID to improve our understanding.
2/
Many studies have found persistent changes in immune cell phenotype & function, months after COVID infection.
Many great docs (@WesElyMD & others) are actively researching long COVID to improve our understanding.
2/
What concerns me is FLCC presenting “protocols” as proven treatments for long COVID.
Throwing 20 medications (9 are prescription 🟥) at a problem with minimal (or no) evidence is irresponsible.
nature.com/articles/s4159…
As we will see, this is both unethical & likely harmful.
3/
Throwing 20 medications (9 are prescription 🟥) at a problem with minimal (or no) evidence is irresponsible.
nature.com/articles/s4159…
As we will see, this is both unethical & likely harmful.
3/

What's the evidence for ivermectin in Long COVID? Basically nothing!
Despite ~200 studies on Long COVID, there are ZERO registered studies of IVM in long COVID.
Even among 86 IVM studies, the only thing even close is a small study looking at anosmia.
Not much evidence...
4/


Despite ~200 studies on Long COVID, there are ZERO registered studies of IVM in long COVID.
Even among 86 IVM studies, the only thing even close is a small study looking at anosmia.
Not much evidence...
4/



What evidence do ivermectin proponents cite?
Kory references ONE uncontrolled study (really just an abstract;👀 below), where they gave n=33 people ivermectin at increasing doses & eventually they got better. Preprint posted in July 2020. Still unpublished.
Not compelling...
5/

Kory references ONE uncontrolled study (really just an abstract;👀 below), where they gave n=33 people ivermectin at increasing doses & eventually they got better. Preprint posted in July 2020. Still unpublished.
Not compelling...
5/


Not only are there *ZERO* published RCTs of ivermectin in long COVID (or any in progress), there isn't even *ONE* controlled study.
The 'evidence base' for ivermectin in long COVID consists of one sketchy unpublished uncontrolled pre-print abstract of n=33 pts.
Thats it.
6/
The 'evidence base' for ivermectin in long COVID consists of one sketchy unpublished uncontrolled pre-print abstract of n=33 pts.
Thats it.
6/
On to the other aspects of the “protocol”:
Chronic steroids in COVID is a complex question. For outpatients who were never hypoxic there’s NO evidence for benefit (and quite possibly harm) with steroids.
7/
Chronic steroids in COVID is a complex question. For outpatients who were never hypoxic there’s NO evidence for benefit (and quite possibly harm) with steroids.
7/
https://twitter.com/nickmmark/status/1484577850833268736

What’s the evidence for chronic steroids in post COVID outpatients?
Again basically nothing.
One RCT was done. It’s still unpublished so we don’t know if it helped or made things worse.
A few observational studies with contradictory results.
No good evidence for steroids
8/


Again basically nothing.
One RCT was done. It’s still unpublished so we don’t know if it helped or made things worse.
A few observational studies with contradictory results.
No good evidence for steroids
8/



This is not to say they is no role for steroids post-COVID. There *may* be a role for a longer steroid course in select patients (e.g. organizing pneumonia or fibrosis on chest CT) but no such subtlety is present in the FLCCC protocol.
Just 3 weeks of steroids for everyone!
9/
Just 3 weeks of steroids for everyone!
9/
On to the next Rx: low dose naltrexone
There is a *theoretical* argument that naltrexone inhibits ERK1/2 signaling, which downregulates inflammation... again there is no clinical data that this is actually beneficial.
No studies on naltrexone whatsoever in long COVID.
10/
There is a *theoretical* argument that naltrexone inhibits ERK1/2 signaling, which downregulates inflammation... again there is no clinical data that this is actually beneficial.
No studies on naltrexone whatsoever in long COVID.
10/
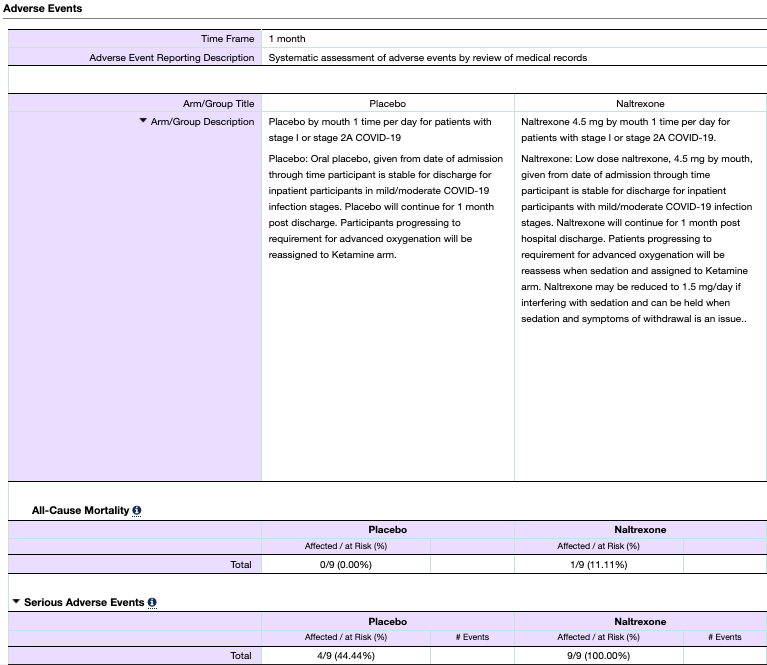
There is ONE study that actually looked at naltrexone in acute COVID19: SINK-COVID19 (NCT0436598)
clinicaltrials.gov/ct2/show/resul…
It randomized n=9 people to naltrexone vs n=9 to placebo.
It found no difference in ANY outcome.
It's the *ONLY* public data about naltrexone in COVID.
11/


clinicaltrials.gov/ct2/show/resul…
It randomized n=9 people to naltrexone vs n=9 to placebo.
It found no difference in ANY outcome.
It's the *ONLY* public data about naltrexone in COVID.
11/


On to the "second line therapies"
Fluvoxamine *IS* indeed a promising therapy for COVID. It's been shown to reduce hospitalizations/ED visits among outpatients who are newly diagnosed with COVID.
But does that mean it works for long COVID too?
12/
Fluvoxamine *IS* indeed a promising therapy for COVID. It's been shown to reduce hospitalizations/ED visits among outpatients who are newly diagnosed with COVID.
https://twitter.com/nickmmark/status/1453500711266766849?s=20&t=RaASSZ1GaW-phXgyvgewyw
But does that mean it works for long COVID too?
12/
There are ZERO RCTs of fluvoxamine in post-COVID. There are also ZERO interventional or observational studies of fluvoxamine in long-COVID.
There is literally no evidence that fluvoxamine reduces symptom severity or duration (or *anything*) in long covid.
13/
There is literally no evidence that fluvoxamine reduces symptom severity or duration (or *anything*) in long covid.
13/

So far this "long COVID protocol" is 0/4 for actual evidence among prescription meds.
What about #5: atorvastatin?
Statins probably DO reduce inflammation & reduce (long term) mortality in most people but the evidence in COVID is surprisingly weak.
hopkinsmedicine.org/news/newsroom/…
14/
What about #5: atorvastatin?
Statins probably DO reduce inflammation & reduce (long term) mortality in most people but the evidence in COVID is surprisingly weak.
hopkinsmedicine.org/news/newsroom/…
14/
There actually ARE well designed studies trying to figure out *IF* statins help in long COVID.
STRONGER an open label n=400 RCT of atorva vs SOC
clinicaltrials.gov/ct2/show/NCT04…
and
HEAL-COVID an n=2631 RCT of atorva vs SOC
clinicaltrials.gov/ct2/show/NCT04…
(Aside: both are great acronyms)
15/

STRONGER an open label n=400 RCT of atorva vs SOC
clinicaltrials.gov/ct2/show/NCT04…
and
HEAL-COVID an n=2631 RCT of atorva vs SOC
clinicaltrials.gov/ct2/show/NCT04…
(Aside: both are great acronyms)
15/


The fact that there are studies ongoing means that there is equipoise about whether these statins work or not.
I'm excited to see the results of STRONGER & HEAL-COVID but I'm not holding my breath. Until results are published there is NO evidence for statins in long COVID.
16/
I'm excited to see the results of STRONGER & HEAL-COVID but I'm not holding my breath. Until results are published there is NO evidence for statins in long COVID.
16/
On to the next & oddest med in this protocol: Maraviroc.
Maravaric is a CCR5 chemokine receptor antagonist, used to treat HIV infection by blocking its entry into CCR5 expressing cells.
Maraviroc isn't generic & it's expensive: typically over $2000 for the 300mg BID dose.
17/
Maravaric is a CCR5 chemokine receptor antagonist, used to treat HIV infection by blocking its entry into CCR5 expressing cells.
Maraviroc isn't generic & it's expensive: typically over $2000 for the 300mg BID dose.
17/

As with everything else in the this protocol, there are exactly ZERO studies of Maravaric in long COVID.
No RCTs. No interventional studies. No observational studies. Nothing. Nada.
Pay $2k/month for 2 months (which insurance definitely won't cover) based on no evidence.
18/
No RCTs. No interventional studies. No observational studies. Nothing. Nada.
Pay $2k/month for 2 months (which insurance definitely won't cover) based on no evidence.
18/
Interestingly, there were 2 early stage trials of maraviroc in severe COVID, w/ the hypothesis that blocking CCR5 would reduce neutrophil infiltrates in 🫁 preventing/mitigating ARDS
This is a nice *idea* for an inpatient clinical trial. NOT an outpatient treatment protocol
19/
This is a nice *idea* for an inpatient clinical trial. NOT an outpatient treatment protocol
19/

But here's where it gets even sketchier...
The protocol says consider "getting an InCellDx test to assess long hauler index"
Huh?
Looks like another COVID grifter has entered the scene.
motherjones.com/politics/2022/…
20/

The protocol says consider "getting an InCellDx test to assess long hauler index"
Huh?
Looks like another COVID grifter has entered the scene.
motherjones.com/politics/2022/…
20/


Basically, InCellDx used a 14 cytokine panel to do a tiny study in 121 post-COVID pts vs 29 health controls
They found tiny cytokine changes but via the magic of ML created an overfit unvalidated random forest model to spit out "long haul covid index"
frontiersin.org/articles/10.33…
21/
They found tiny cytokine changes but via the magic of ML created an overfit unvalidated random forest model to spit out "long haul covid index"
frontiersin.org/articles/10.33…
21/

InCellDx's science is 'meh' but their marketing is top notch!
InCellDx turned their cytokine test & "long haul COVID index" into quite the product.
They created a COVID support group "COVID long haulers" to push the test.
They also appear to have partnered w/ FLCCC & others.
22/


InCellDx turned their cytokine test & "long haul COVID index" into quite the product.
They created a COVID support group "COVID long haulers" to push the test.
They also appear to have partnered w/ FLCCC & others.
22/



Never mind the inconvenient question: "WHY do this expensive cytokine test for long COVID?"
What clinical implications does that test have? There's absolutely no evidence to start or stop *any* therapy based on the result.
At best this is a research tool. At worst a scam.
23/
What clinical implications does that test have? There's absolutely no evidence to start or stop *any* therapy based on the result.
At best this is a research tool. At worst a scam.
23/
Another point about bad data science:
The group used a technique called SMOTE (synthetic minority over sampling technique). I’ve used this before. It’s great for rare events but it’s super weird to use it to oversample healthy controls. Why not get more volunteers?
A big 🚩
The group used a technique called SMOTE (synthetic minority over sampling technique). I’ve used this before. It’s great for rare events but it’s super weird to use it to oversample healthy controls. Why not get more volunteers?
A big 🚩
Talking to people who have been through it:
After the $360 test, InCellDx charges $200 for a video consultation, then $300 for more tests.
Then a referral to a FLCCC approved doc ($200+) followed by $2k/month for maraviroc.
Seems like InCellDx is cashing in on long COVID.
24/
After the $360 test, InCellDx charges $200 for a video consultation, then $300 for more tests.
Then a referral to a FLCCC approved doc ($200+) followed by $2k/month for maraviroc.
Seems like InCellDx is cashing in on long COVID.
24/
As for another prescription included in this protocol: high dose diuretics (spironolactone).
Starting spironolactone at higher than recommended dose *without checking electrolytes* is dangerous & potentially malpractice.
I’ve written about this previously👇
25/
Starting spironolactone at higher than recommended dose *without checking electrolytes* is dangerous & potentially malpractice.
I’ve written about this previously👇
25/
https://twitter.com/nickmmark/status/1484587021045694468
Last but not least: Montelukast.
As a pulmonologist, I know this med very well & there are reasons to think it *could* help alleviate dyspnea after COVID pneumonia.
But what’s the actual evidence for montelukast in long COVID?
Once again not very much…
26/
As a pulmonologist, I know this med very well & there are reasons to think it *could* help alleviate dyspnea after COVID pneumonia.
But what’s the actual evidence for montelukast in long COVID?
Once again not very much…
26/
There actually are ongoing clinical trials of montelukast in long COVID, such as the well named E-SPERANZA study in 🇪🇸
clinicaltrials.gov/ct2/show/NCT04…
This trial is predicated upon a 13 person uncontrolled pilot study. That n=13 study is the sum total of evidence for Montelukast btw
27/
clinicaltrials.gov/ct2/show/NCT04…
This trial is predicated upon a 13 person uncontrolled pilot study. That n=13 study is the sum total of evidence for Montelukast btw
27/

One article proposes using montelukast because of “the lack of effective therapy, chemo prevention, & vaccination.”
Oh wait we have all of those things now. Maybe we don’t need montelukast…?
This raises an important point. The best way to prevent long COVID is vaccination!
28/
Oh wait we have all of those things now. Maybe we don’t need montelukast…?
This raises an important point. The best way to prevent long COVID is vaccination!
28/

Speaking of effective: there is evidence that vaccination can improve long COVID symptoms!
In an observational study of n=163 people with severe long COVID 8 months after infection, 95% reported improved/stable symptoms 1 month following vaccination
pubmed.ncbi.nlm.nih.gov/34029484/
29/
In an observational study of n=163 people with severe long COVID 8 months after infection, 95% reported improved/stable symptoms 1 month following vaccination
pubmed.ncbi.nlm.nih.gov/34029484/
29/
If the FLCCC protocol is what NOT to do, how *should* we treat long COVID?
UpToDate has a pretty good open access article:
uptodate.com/contents/covid…
27/
UpToDate has a pretty good open access article:
uptodate.com/contents/covid…
27/
Instead of a one size fits all kitchen sink approach involving 20+ meds (each with potential side effects), it recommends a stepwise approach based on symptoms, timing, & severity.
There are actual proven therapies for post ICU syndrome & sequelae of critical illness.
27/
There are actual proven therapies for post ICU syndrome & sequelae of critical illness.
27/
If you are suffering from long COVID, there are reputable doctors who can help. There are centers of excellence (such as the @CIBScenter) & clinical trials you can enroll in (see the 🧵 above).
Don’t get taken advantage of by discredited scam artists pushing “protocols”.
28/
Don’t get taken advantage of by discredited scam artists pushing “protocols”.
28/
Summary:
-the “I-RECOVER protocol” of 20 meds is dangerous nonsense. None of these interventions is based on robust clinical trials.
-taking an unproven combination of meds could make you feel worse not better.
-don’t get conned into paying these quacks for this “protocol”
fin/
-the “I-RECOVER protocol” of 20 meds is dangerous nonsense. None of these interventions is based on robust clinical trials.
-taking an unproven combination of meds could make you feel worse not better.
-don’t get conned into paying these quacks for this “protocol”
fin/

• • •
Missing some Tweet in this thread? You can try to
force a refresh
































