
✳️ #TenTweetNephJC ✳️
👉 where we catch you up on the week's #NephJC chat in 10 tweets
The topic at hand was Plasma Exchange and Vasculitis: the infamous debate of to PLEX or not to PLEX in AAV
Check out this thread to see if you change your mind on this comPLEX topic 👇
👉 where we catch you up on the week's #NephJC chat in 10 tweets
The topic at hand was Plasma Exchange and Vasculitis: the infamous debate of to PLEX or not to PLEX in AAV
Check out this thread to see if you change your mind on this comPLEX topic 👇
What did I miss?
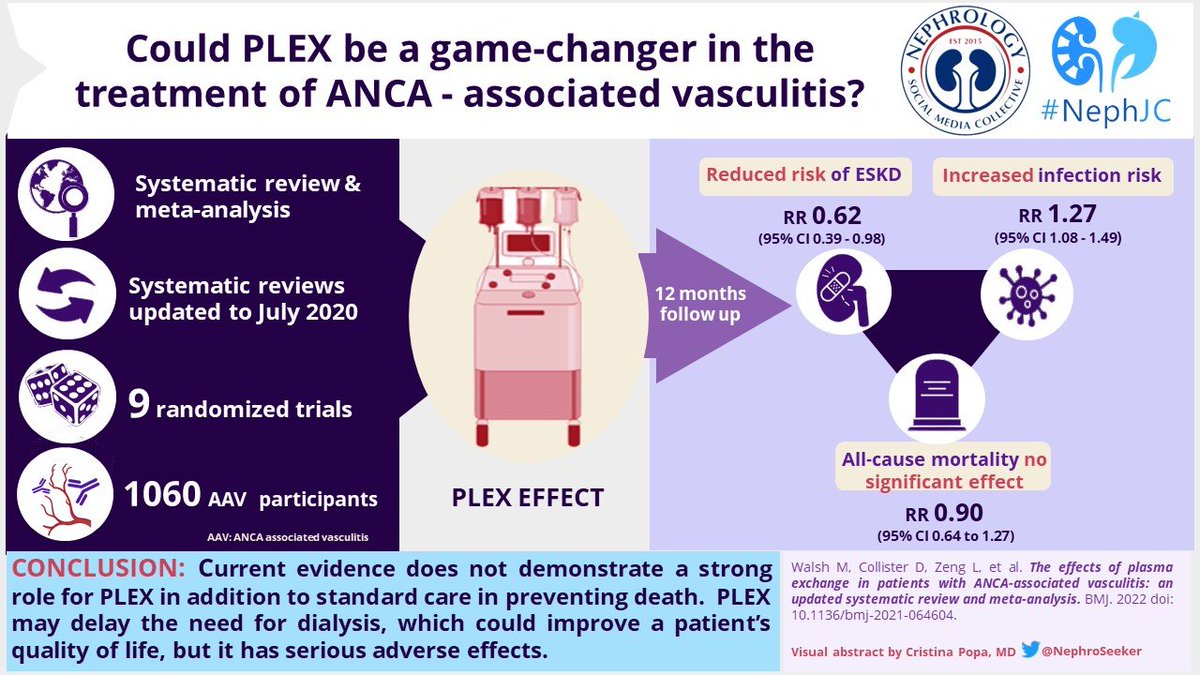
PLEX, with its plausible biological rationale, has been in the center of debate for management of AAV since the 1980s, with several RCTs in favor of PLEX or against it
🔸️An updated meta-analysis which included the PEXIVAS results was discussed
PLEX, with its plausible biological rationale, has been in the center of debate for management of AAV since the 1980s, with several RCTs in favor of PLEX or against it
🔸️An updated meta-analysis which included the PEXIVAS results was discussed
1 tweet methods
✅ updated systematic review & meta-analysis
✅ RCTs of patients with AAV or pauci-immune RPGN receiving PLEX and ≥12mo. follow-up
✅ Outcome measures were at least one of: mortality, ESKD, serious infection, relapse, AE or health-related QoL
✅ updated systematic review & meta-analysis
✅ RCTs of patients with AAV or pauci-immune RPGN receiving PLEX and ≥12mo. follow-up
✅ Outcome measures were at least one of: mortality, ESKD, serious infection, relapse, AE or health-related QoL
1 tweet results
🔹9 RCTs (n, 1060)
❌No effect on all-cause mortality
RR risk 0.90 (95% CI 0.64 - 1.27)
🔹7 RCTs (n, 999)
⬇️ risk of ESKD at 12 mo.
RR 0.62 (0.39 - 0.98)
❌No effect long-term
🔹4 RCTs (n, 908)
⬆️ risk of serious infections over 12 mo.
RR 1.27 (1.08 - 1.49)
🔹9 RCTs (n, 1060)
❌No effect on all-cause mortality
RR risk 0.90 (95% CI 0.64 - 1.27)
🔹7 RCTs (n, 999)
⬇️ risk of ESKD at 12 mo.
RR 0.62 (0.39 - 0.98)
❌No effect long-term
🔹4 RCTs (n, 908)
⬆️ risk of serious infections over 12 mo.
RR 1.27 (1.08 - 1.49)
Give me something clever to say
“This meta-analysis demonstrates the unexpected, differential effects of PLEX on ESKD compared with all-cause mortality, which dramatically reduced the power of PEXIVAS to reliably estimate the benefits of PLEX using a composite outcome.”
“This meta-analysis demonstrates the unexpected, differential effects of PLEX on ESKD compared with all-cause mortality, which dramatically reduced the power of PEXIVAS to reliably estimate the benefits of PLEX using a composite outcome.”
Chat consensus?
1️⃣ Most would continue to use PLEX in patients with PAH
2️⃣ Most wouldn't consider PLEX with a creatinine level <500 µmol/L
3️⃣ Involving patients in decision making and choose patients with ⬆️ risk of ESKD and ⬇️ risk of infections
1️⃣ Most would continue to use PLEX in patients with PAH
2️⃣ Most wouldn't consider PLEX with a creatinine level <500 µmol/L
3️⃣ Involving patients in decision making and choose patients with ⬆️ risk of ESKD and ⬇️ risk of infections
Quote of the fortnight!
"@NephJC My favorite quote when researching for this summary #NephJC "
"
@brian_rifkin
"@NephJC My favorite quote when researching for this summary #NephJC
 "
" @brian_rifkin
I want more info
✅ Summary from @nephrologik and @drpriyajohn
nephjc.com/news/anca-plex
✅Follow @lastwalsh and read his slides summarizing his paper:
✅ VA by @NephroSeeker
✅ Summary from @nephrologik and @drpriyajohn
nephjc.com/news/anca-plex
✅Follow @lastwalsh and read his slides summarizing his paper:
https://twitter.com/vasculitis2022/status/1511642259443363840?s=21
✅ VA by @NephroSeeker
Final thoughts
✳️After the pessimism post-PEXIVAS, this meta-analysis gives believers some justification by showing less ESKD at one year (but at a cost)
➡️Up next - shifting gears to discuss the new ISPD peritonitis guidelines
See you on 19-20th April!
Tweetorial by @Husamjz
✳️After the pessimism post-PEXIVAS, this meta-analysis gives believers some justification by showing less ESKD at one year (but at a cost)
➡️Up next - shifting gears to discuss the new ISPD peritonitis guidelines
See you on 19-20th April!
Tweetorial by @Husamjz
• • •
Missing some Tweet in this thread? You can try to
force a refresh










