1/11
A 55 y/o man presents for evaluation of chronic diarrhea. We walk into the room to meet him.
We have an opportunity to make an “augenblick” diagnosis – one that can be made in the blink of an eye.
A 55 y/o man presents for evaluation of chronic diarrhea. We walk into the room to meet him.
We have an opportunity to make an “augenblick” diagnosis – one that can be made in the blink of an eye.
2/11
We listen to his heart to help confirm our hypothesis (best with headphones). There is a holosystolic murmur over the LLSB. Notice that the intensity of the murmur seems to vary in a regular cycle? It gets louder/quieter/louder/quieter. What is the significance of this?
We listen to his heart to help confirm our hypothesis (best with headphones). There is a holosystolic murmur over the LLSB. Notice that the intensity of the murmur seems to vary in a regular cycle? It gets louder/quieter/louder/quieter. What is the significance of this?
3/11
The augmentation of the murmur during inspiration is known as Carvallo’s sign, and indicates that the abnormal heart sound is coming from the R-side of the heart. Here is a more dramatic example in a different patient with tricuspid stenosis:
The augmentation of the murmur during inspiration is known as Carvallo’s sign, and indicates that the abnormal heart sound is coming from the R-side of the heart. Here is a more dramatic example in a different patient with tricuspid stenosis:
4/11
Our patient has tricuspid regurgitation. We’ve made a diagnosis, but does it end there? No. We must now determine the cause of the TR.
Similar to the “diagnosis” of anemia. . .we don’t stop there, we must determine the underlying cause.
So what is the cause of TR here?
Our patient has tricuspid regurgitation. We’ve made a diagnosis, but does it end there? No. We must now determine the cause of the TR.
Similar to the “diagnosis” of anemia. . .we don’t stop there, we must determine the underlying cause.
So what is the cause of TR here?
5/11
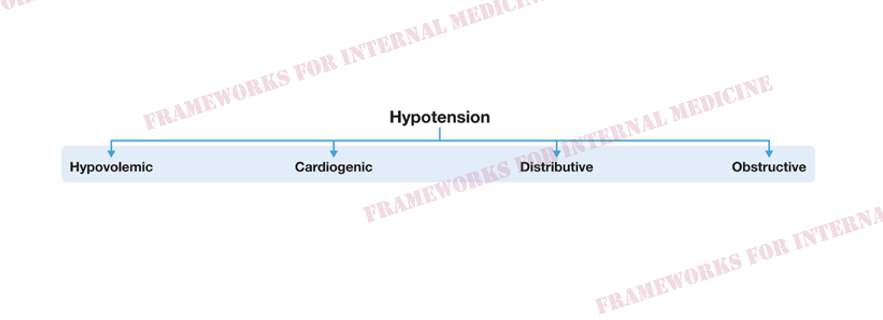
Let’s get back to the chief complaint of diarrhea. Is there a tie-in with tricuspid regurgitation? We consult our framework for diarrhea:
Let’s get back to the chief complaint of diarrhea. Is there a tie-in with tricuspid regurgitation? We consult our framework for diarrhea:

6/11
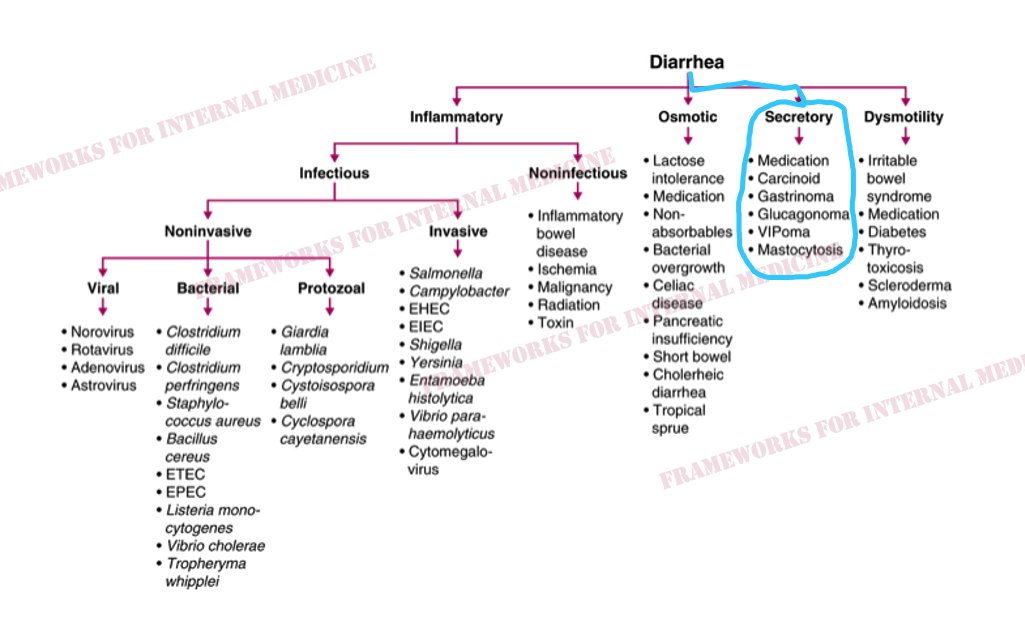
The diarrhea is chronic and non-bloody, making infectious (and other inflammatory) causes less likely.
The diarrhea is chronic and non-bloody, making infectious (and other inflammatory) causes less likely.

7/11
Additional history reveals that the diarrhea occurs up to 15 times per day, and persists even during periods when he does not eat. These features suggest a secretory cause.
Additional history reveals that the diarrhea occurs up to 15 times per day, and persists even during periods when he does not eat. These features suggest a secretory cause.
8/11
Is there a cause of secretory diarrhea in the framework that can be associated with tricuspid valve regurgitation? Yes there is.
Is there a cause of secretory diarrhea in the framework that can be associated with tricuspid valve regurgitation? Yes there is.

9/11
Vasoactive substances released by carcinoid tumors can damage the heart valves, leading to stenosis and/or regurgitation. Left-sided valves are spared in most cases because the lungs inactivate the vasoactive substances before they reach the left side of the heart.
Vasoactive substances released by carcinoid tumors can damage the heart valves, leading to stenosis and/or regurgitation. Left-sided valves are spared in most cases because the lungs inactivate the vasoactive substances before they reach the left side of the heart.
10/11
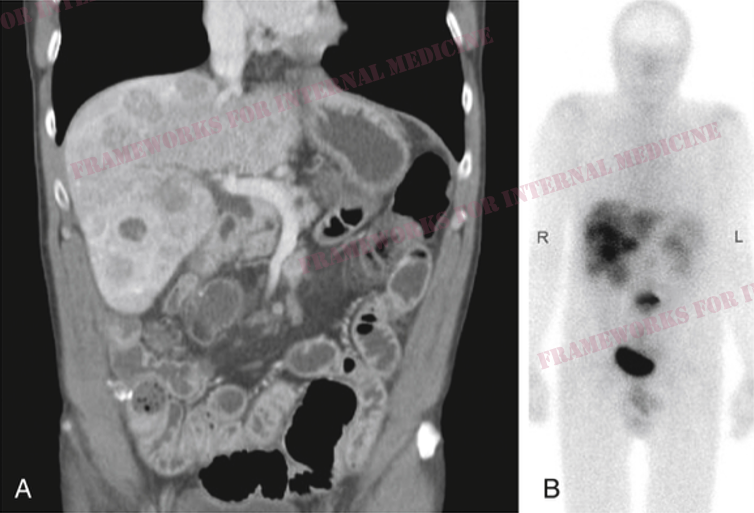
Octreotide scan shows areas of normal radiotracer uptake (bladder, kidneys, spleen), but there is a focus of increased uptake in the region of the small intestine (the primary tumor site), and multiple globular foci of increased uptake in the liver (mets).
Octreotide scan shows areas of normal radiotracer uptake (bladder, kidneys, spleen), but there is a focus of increased uptake in the region of the small intestine (the primary tumor site), and multiple globular foci of increased uptake in the liver (mets).
11/11
First, we diagnosed TR with our eyes only. An augenblick diagnosis.
Next, we used the diarrhea framework to identify a connection to TR, leading to hypothesis-driven confirmation.
For more cases: physicaldiagnosispdx.com/case-presentat…
For more frameworks: amazon.com/Frameworks-Int…
First, we diagnosed TR with our eyes only. An augenblick diagnosis.
Next, we used the diarrhea framework to identify a connection to TR, leading to hypothesis-driven confirmation.
For more cases: physicaldiagnosispdx.com/case-presentat…
For more frameworks: amazon.com/Frameworks-Int…
• • •
Missing some Tweet in this thread? You can try to
force a refresh