1/ As the team starts discussing patient #16 on the list during rounds, you look around & notice:
Learner 1: *👀 at their phone*
Learner 2: *🥱, almost 🛌*
Learner 3: *🥺 pleading for rounds to end*
How can you keep everyone engaged?!
If this feels familiar, check out this 🧵!
Learner 1: *👀 at their phone*
Learner 2: *🥱, almost 🛌*
Learner 3: *🥺 pleading for rounds to end*
How can you keep everyone engaged?!
If this feels familiar, check out this 🧵!

2/ This week, we are continuing our discussion about opportunities for inpatient teaching during rounds with a focus on how to keep learners engaged.
Although these tips are primarily for rounds that do NOT occur at the bedside, many of the same principles apply.
Although these tips are primarily for rounds that do NOT occur at the bedside, many of the same principles apply.

3/ For tips on how to engage all learners at the bedside, check out this recent thread from @YihanYangMD on engaging all learners at the bedside with physical exam teaching:
https://twitter.com/YihanYangMD/status/1503772148774572032
4/ As I mentioned previously, I often start with teaching BEFORE rounds.
Then, once rounds begin, everyone is already turned away from their computers, involved in the discussion, and primed to learn.
https://twitter.com/JenniferSpicer4/status/1455572216268132353
Then, once rounds begin, everyone is already turned away from their computers, involved in the discussion, and primed to learn.
5/ Now that I have the team's attention, it's important for me to maintain it during rounds by involving EVERYONE in the discussion of ALL patients, not just their own.
At the beginning of the month, I set this expectation. Because sometimes other team members have great ideas!
At the beginning of the month, I set this expectation. Because sometimes other team members have great ideas!
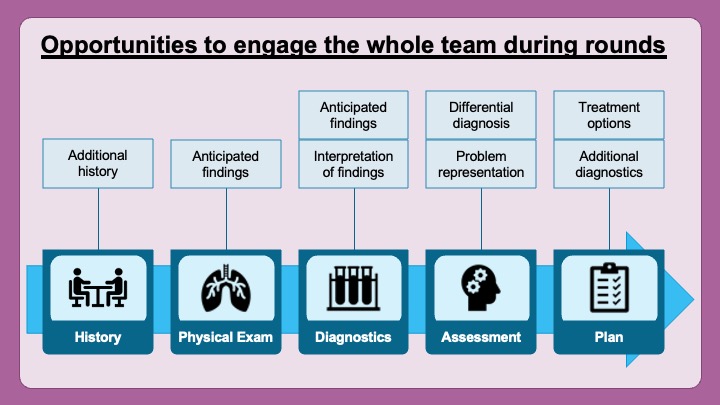
6/ So let's talk about opportunities to involve other team members during patient presentations.
None of this is ground-breaking. You probably ask these questions already!
BUT...I want us to think about how we can use these questions to engage other members of the team.
None of this is ground-breaking. You probably ask these questions already!
BUT...I want us to think about how we can use these questions to engage other members of the team.

7/ So after a team member finishes presenting portions of the history, I ask other team members to weigh in:
What else do they want to know?
What do they think is going on?
This promotes other team members' active listening!
What else do they want to know?
What do they think is going on?
This promotes other team members' active listening!

8/ I may ask other team members to REQUEST portions of the exam or PREDICT what they would see based on their current hypotheses.
This teaches the team to use the exam as a diagnostic tool (and could be done at the bedside too!).
This teaches the team to use the exam as a diagnostic tool (and could be done at the bedside too!).

9/ Instead of the presenter list all of the labs, I ask other team members what tests they want & why. THEN the presenter shares in any other unexpected labs.
Or sometimes I have other team members read the patient's EKG/imaging/PFTs, then the presenter share the official read.
Or sometimes I have other team members read the patient's EKG/imaging/PFTs, then the presenter share the official read.

10/ @gradydoctor once told me her trick of having a different team member summarize the relevant data into the problem representation. (sgim.org/web-only/clini…)
Again, brilliant! This requires everyone to listen and helps teach clinical reasoning skills during the case.
Again, brilliant! This requires everyone to listen and helps teach clinical reasoning skills during the case.

11/ I always allow the presenter to provide their ddx; however, when we have a true diagnostic mystery, I ask everyone to add additional thoughts.
This works great on our HIV service when I'm trying to teach residents a structured approach to HIV syndromes.
This works great on our HIV service when I'm trying to teach residents a structured approach to HIV syndromes.

12/ Then I do the same thing for the plan.
The presenter gets the first run at the plan, but other team members have the opportunity to add their thoughts on the diagnostic plan.
The presenter gets the first run at the plan, but other team members have the opportunity to add their thoughts on the diagnostic plan.

13/ And finally, when discussing treatment, I love to have team members debate treatment options, ESPECIALLY when selecting antibiotics.
Often, there's not ONE correct answer, so everyone has different thoughts!
Even better: have them write it on a notecard, then share & debate
Often, there's not ONE correct answer, so everyone has different thoughts!
Even better: have them write it on a notecard, then share & debate

14/ The key to making this effective is to ensure that the presenter knows that THEY ARE IN CHARGE of the decision-making.
You don't want team members one-upping each other; rather, create a spirit of team discussion while allowing the presenter to make the final decision.
You don't want team members one-upping each other; rather, create a spirit of team discussion while allowing the presenter to make the final decision.
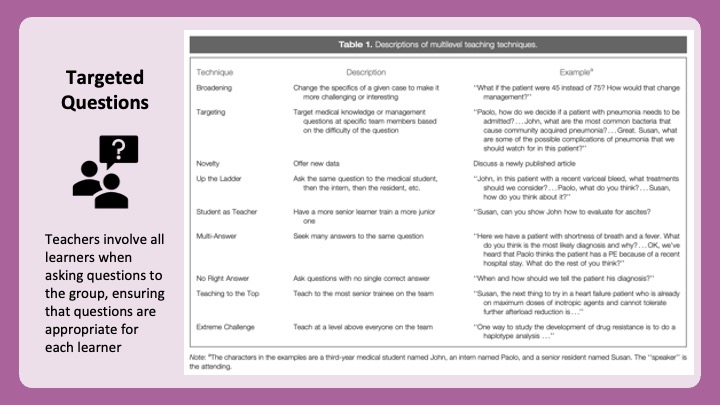
15/ And if you're looking for tips on engaging multi-level learners, then review this tweetorial.
When asking the group questions, use either:
1⃣ open-ended questions with potential multiple answers
2⃣questions targeted to a specific learner level
https://twitter.com/JenniferSpicer4/status/1447981442135384064
When asking the group questions, use either:
1⃣ open-ended questions with potential multiple answers
2⃣questions targeted to a specific learner level
16/ So, in summary, consider how you can ask the TEAM to engage during each presentation.
Don't just ask these questions to the presenter.
Asking other members of the team engages them as active listeners and makes patient care a true team experience.
Don't just ask these questions to the presenter.
Asking other members of the team engages them as active listeners and makes patient care a true team experience.
17/ Join us next week for #TweetorialTuesday when @GStetsonMD will discuss how to drop teaching pearls on rounds.
And don't forget to follow @YihanYangMD, @ChrisDJacksonMD, & the @MedEdTwagTeam so that you don't miss a thread.
And don't forget to follow @YihanYangMD, @ChrisDJacksonMD, & the @MedEdTwagTeam so that you don't miss a thread.

• • •
Missing some Tweet in this thread? You can try to
force a refresh