Part 6️⃣ in my extremes of animal physiology #tweetorial series:
Case 1: How low can PaO2 go?
You are called by the lab about an abnormal ABG result.
pH 7.5 / PaCO2 20 / PaO2 22 / HCO3 15
“That’s gotta be venous” they say.
“No” you reply, “Its from a ___"
1/
Case 1: How low can PaO2 go?
You are called by the lab about an abnormal ABG result.
pH 7.5 / PaCO2 20 / PaO2 22 / HCO3 15
“That’s gotta be venous” they say.
“No” you reply, “Its from a ___"
1/
Answer: bar-headed goose!
The Himalayan summits are almost lifeless.
In the midst of this barren landscape, breathless climbers have heard the thrum of wings & the honking of geese above their heads.
How can these geese breathe so easily while flying at over 8000m?
2/

The Himalayan summits are almost lifeless.
In the midst of this barren landscape, breathless climbers have heard the thrum of wings & the honking of geese above their heads.
How can these geese breathe so easily while flying at over 8000m?
2/


Bar headed geese have many amazing adaptions to altitude: large hearts, specialized hemoglobins, highly capillarized muscles with dense mitochondria, and cerebral insensitivity to hypocapnia.
But most of all they have amazing lung physiology!
ncbi.nlm.nih.gov/pmc/articles/P…
3/
But most of all they have amazing lung physiology!
ncbi.nlm.nih.gov/pmc/articles/P…
3/

Unlike mammalian lungs with reciprocating airflow in & out, birds have continuous airflow from cranial to caudal air sacs.
This reduces dead space & enables a denser network of airways & blood vessels, with a highly efficient countercurrent exchange.
erj.ersjournals.com/content/29/1/11
4/



This reduces dead space & enables a denser network of airways & blood vessels, with a highly efficient countercurrent exchange.
erj.ersjournals.com/content/29/1/11
4/




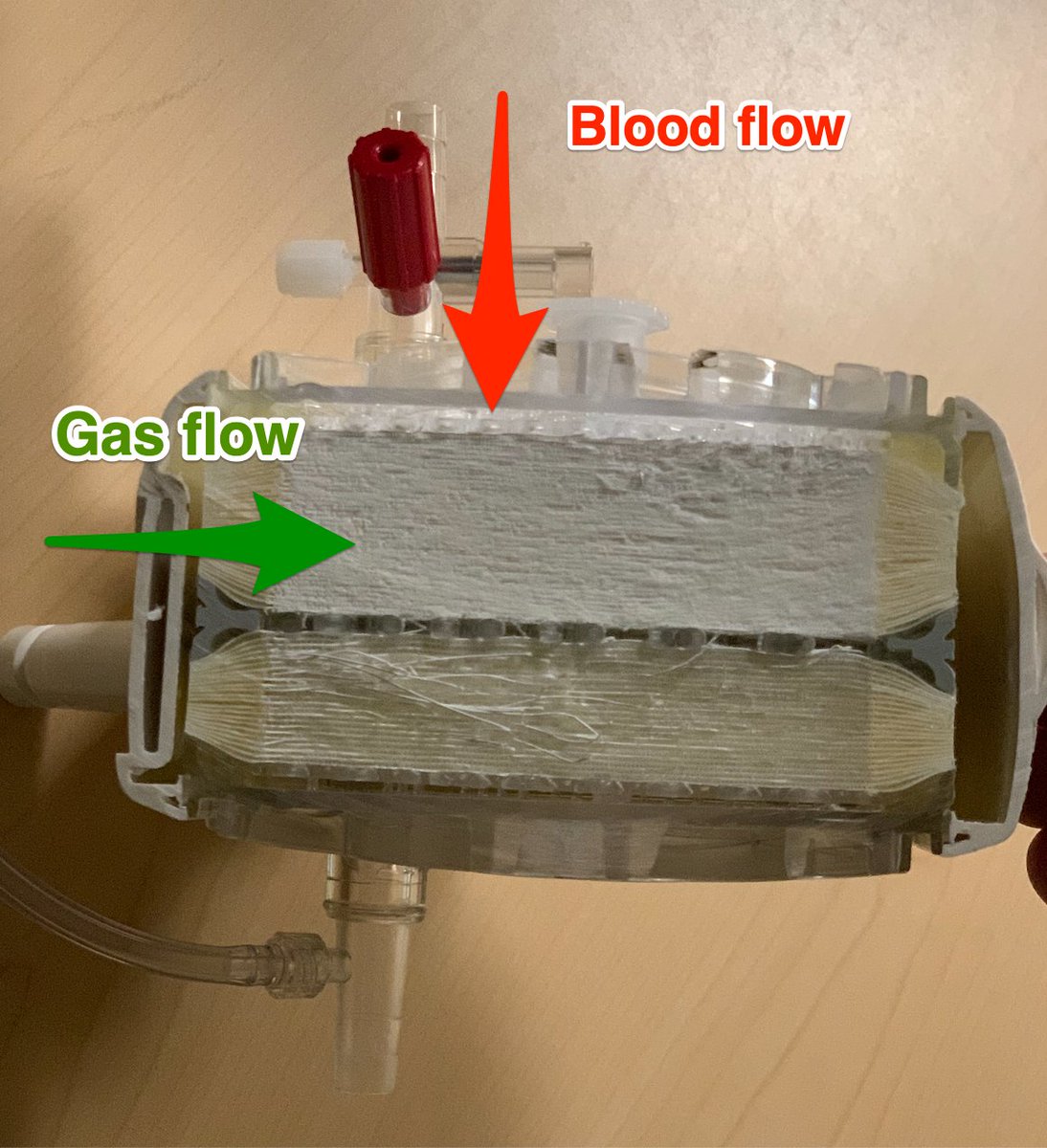
Clinical aside: countercurrent flow across thin tubules also explains why an ECMO membrane lung is so efficient.
Look at this oxygenator I cut open: Just like the bird lung, gas flow is opposite to the direction of blood flow.
Countercurrents rock!
5/


Look at this oxygenator I cut open: Just like the bird lung, gas flow is opposite to the direction of blood flow.
Countercurrents rock!
5/


How about climbers?
Their ABG has a greater respiratory alkalosis than a goose
We know because 4 climbers drew femoral ABGs at 8400m (at rest w/o supplemental O2)
PaO2 of 24 & SpO2 of 54%1 These are truly the limits of human physiology!
pubmed.ncbi.nlm.nih.gov/19129527/
6/
Their ABG has a greater respiratory alkalosis than a goose
We know because 4 climbers drew femoral ABGs at 8400m (at rest w/o supplemental O2)
PaO2 of 24 & SpO2 of 54%1 These are truly the limits of human physiology!
pubmed.ncbi.nlm.nih.gov/19129527/
6/

This bring up an important question: how do we measure ABGs in flying birds?
Answer: we don’t!
To measure ABGs, they *simulated* high altitude flight by running geese on treadmills under hypoxic conditions!
Yes that Goose has a Swan!
pubmed.ncbi.nlm.nih.gov/2506620/
7/


Answer: we don’t!
To measure ABGs, they *simulated* high altitude flight by running geese on treadmills under hypoxic conditions!
Yes that Goose has a Swan!
pubmed.ncbi.nlm.nih.gov/2506620/
7/



How good are bird lungs? Or put another way, how high can birds fly?
We don’t know!
We know that Rüppell's Griffon Vulture can fly to *at least* 37,000 feet because one got struck by an airliner at that altitude.
37,000 feet (11,300m) has an O2 tension of just 36 mmHg!
8/

We don’t know!
We know that Rüppell's Griffon Vulture can fly to *at least* 37,000 feet because one got struck by an airliner at that altitude.
37,000 feet (11,300m) has an O2 tension of just 36 mmHg!
8/


Case 2: extreme bronchoscopy
Some docs feel like it's too hard to perform a bronchoscopy outside the controlled environment of the bronch suite.
In which of the following situations has bronchoscopy been successfully performed?
9/
Some docs feel like it's too hard to perform a bronchoscopy outside the controlled environment of the bronch suite.
In which of the following situations has bronchoscopy been successfully performed?
9/
Answer: all of the above!
🐘 Elephants *frequently* contract TB. Bronchoscopy has been performed in elephants (it doesn’t look easy) & apparently a trunk nerve block helps!
bit.ly/3EH7zoi
10/

🐘 Elephants *frequently* contract TB. Bronchoscopy has been performed in elephants (it doesn’t look easy) & apparently a trunk nerve block helps!
bit.ly/3EH7zoi
10/


Clinical 🥡:
TB is common in elephants (2% of Africa Elephants & 12% of Asian Elephants have TB).
People who work around elephants can get TB from them. Remember this the next time you evaluate a zookeeper with fevers & night sweats!
11/
TB is common in elephants (2% of Africa Elephants & 12% of Asian Elephants have TB).
People who work around elephants can get TB from them. Remember this the next time you evaluate a zookeeper with fevers & night sweats!
https://twitter.com/nickmmark/status/1469794321385680899?s=20&t=3YRgUHgvGZqjvpZGibAnng
11/
🐬 bronchoscopy is possible but has some challenges.
First the laryngeal spout - an amazing water/pressure tight organ - must be anesthetized & passed, but it only opens for a fraction of a second.
This makes navigating human vocal cords seem easy!
12/


First the laryngeal spout - an amazing water/pressure tight organ - must be anesthetized & passed, but it only opens for a fraction of a second.
This makes navigating human vocal cords seem easy!
12/



Once past the laryngeal spout and within in the trachea, don’t be fooled by a tracheal bronchus!
Many animals including 🐘, 🐐, 🐫, 🐋,🐖, and 1% of humans have a tracheal bronchus.
See my prior 🧵 for more on pig bronchi:
13/
Many animals including 🐘, 🐐, 🐫, 🐋,🐖, and 1% of humans have a tracheal bronchus.
See my prior 🧵 for more on pig bronchi:
https://twitter.com/nickmmark/status/1434137941245267977?s=20&t=rCvHWZ6VZsYzo7041faSkA
13/
Clinical 🥡:
Tracheal bronchi can cause unexplained lobar collapse in intubated people if the ETT occludes the opening. This can cause unexplained hypoxemia + RUL collapse.
Always consider a pig bronchus on your differential for upper lobe collapse in the ICU!
14/
Tracheal bronchi can cause unexplained lobar collapse in intubated people if the ETT occludes the opening. This can cause unexplained hypoxemia + RUL collapse.
Always consider a pig bronchus on your differential for upper lobe collapse in the ICU!
14/
Finally, there are some unique challenges to interventional pulmonary procedures in dolphins.
For example, you can’t use electrocautery in an animal that has to stay wet!
I highly recommend this article for:
atsjournals.org/doi/full/10.15…
15/

For example, you can’t use electrocautery in an animal that has to stay wet!
I highly recommend this article for:
atsjournals.org/doi/full/10.15…
15/


Galloping horses do sometimes develop stridor.
Even a small tracheal stenosis can cause big problems when your minute ventilation at peak exercise is >1600 L/min!
How can you evaluate exercise induced wheezing in a thoroughbred horse?
17/
Even a small tracheal stenosis can cause big problems when your minute ventilation at peak exercise is >1600 L/min!
How can you evaluate exercise induced wheezing in a thoroughbred horse?
17/

Bronchoscopy, of course: turns out it is possible to perform bronchoscopies in galloping horses (on a treadmill) to evaluate for dynamic airway collapse! Crazy!
pubmed.ncbi.nlm.nih.gov/19562896/
18/
pubmed.ncbi.nlm.nih.gov/19562896/
18/
Case 3: extreme uremia
You are called about “a very abnormal chemistry panel”
“This has gotta be incompatible with life!” the caller exclaims “They need dialysis ASAP!"
“Not so” you reply, “that’s normal for a ___”
19/
You are called about “a very abnormal chemistry panel”
“This has gotta be incompatible with life!” the caller exclaims “They need dialysis ASAP!"
“Not so” you reply, “that’s normal for a ___”
19/

Sodium 282 mmol/L
Potassium 7.3
Chloride 290
Bicarb 3
BUN 1004 mg/dL
Creatinine < 0.1
Osmolarity 1094 mOsm/Kg
This is a normal BMP for a ___
20/
Potassium 7.3
Chloride 290
Bicarb 3
BUN 1004 mg/dL
Creatinine < 0.1
Osmolarity 1094 mOsm/Kg
This is a normal BMP for a ___
20/
Answer: 🦈 Shark
Sharks are osmoconformers, meaning they adjust their internal osm to match the environment, mostly by retaining urea.
The average osmolality of the ocean is 1000 mOsm/L so that’s what shark’s blood is too!
21/

Sharks are osmoconformers, meaning they adjust their internal osm to match the environment, mostly by retaining urea.
The average osmolality of the ocean is 1000 mOsm/L so that’s what shark’s blood is too!
21/


Interestingly, some 🦈 like the Bull shark are diadromous meaning they can transition between fresh water and salt water.
This requires them to radically alter their blood chemistry - particularly BUN - gradually over a week.
Why gradually?
22/


This requires them to radically alter their blood chemistry - particularly BUN - gradually over a week.
Why gradually?
22/



As the 🦈 transitions from salt to fresh water, its kidneys excrete urea.
Urea shifts out of the cells into the blood, *gradually* decreasing the intracellular Osms.
If the 🦈 dropped its BUN too fast its cells would swell, which would look something like this:
23/
Urea shifts out of the cells into the blood, *gradually* decreasing the intracellular Osms.
If the 🦈 dropped its BUN too fast its cells would swell, which would look something like this:
23/
Clinical 🥡:
People with renal failure can have very high BUN too (like over 200!)
Removing BUN too quickly with dialysis can cause cells to swell.
What’s the solution?
Add urea to the dialysate to limit how fast urea can drop!
academic.oup.com/ndt/article/16…
24/

People with renal failure can have very high BUN too (like over 200!)
Removing BUN too quickly with dialysis can cause cells to swell.
What’s the solution?
Add urea to the dialysate to limit how fast urea can drop!
academic.oup.com/ndt/article/16…
24/


Wrong answers:
In contrast to sharks, which are osmoconformers, Camels, dolphins, and chinchilla are osmoregulators.
They try to maintain a blood chemistry that's dissimilar from their environment. And how they do it is pretty cool!
25/
In contrast to sharks, which are osmoconformers, Camels, dolphins, and chinchilla are osmoregulators.
They try to maintain a blood chemistry that's dissimilar from their environment. And how they do it is pretty cool!
25/
Camels crank up their renin-angiotensin-aldosterone system (RAAS) to retain salt/fluid when dehydrated.
Camels can tolerate >20 days without water & their Na rises to 175!
But if they take losartan (blocking RAAS) they become even more hypernatremic!
ncbi.nlm.nih.gov/pmc/articles/P…
26/
Camels can tolerate >20 days without water & their Na rises to 175!
But if they take losartan (blocking RAAS) they become even more hypernatremic!
ncbi.nlm.nih.gov/pmc/articles/P…
26/

Clinical 🥡:
For people, like camels, taking ACE inhibitors is a major risk factor for dehydration under hot conditions.
Remember that people on ACEi are at risk for AKI & dehydration. Be suspicious for dehydration in elderly people taking ACEIs!
journals.plos.org/plosone/articl…
27/
For people, like camels, taking ACE inhibitors is a major risk factor for dehydration under hot conditions.
Remember that people on ACEi are at risk for AKI & dehydration. Be suspicious for dehydration in elderly people taking ACEIs!
journals.plos.org/plosone/articl…
27/

🐪🐫 Side-bar: My son wanted to shared a great mnemonic for remembering the types of camels.
Bactrian - B shaped - two humps
Dromendary - D shaped - one hump
(we even made an infographic about it!)
28/
Bactrian - B shaped - two humps
Dromendary - D shaped - one hump
(we even made an infographic about it!)
28/

Check out my prior thread for more how desert animals can retain water - including how amazing the Chinchilla is: it can concentrate it's urine to > 7500 mOsm/L (thats a SG > 10.60!)
29/
https://twitter.com/nickmmark/status/1352348918617501697?s=20&t=rCvHWZ6VZsYzo7041faSkA
29/
I hope you’ve enjoyed part 6 in my series on what the extremes of animal physiology can teach us about critical care medicine.
30/30
30/30
• • •
Missing some Tweet in this thread? You can try to
force a refresh

































