1/🚨Addiction & Substance Use Science of 2021🚨
Our #SGIM22 team checked >1000 titles to come up with key insights for general med/addiction clinicians and affected communities on:
Opioids
Alcohol
“Potpourri” (nicotine, stimulants+)
Policy
Let's go!
@SocietyGIM
Our #SGIM22 team checked >1000 titles to come up with key insights for general med/addiction clinicians and affected communities on:
Opioids
Alcohol
“Potpourri” (nicotine, stimulants+)
Policy
Let's go!
@SocietyGIM

2/By the way, here's "our team" for #SGIM22 includes:
Kenny Morford from @YaleADM
@_kmullins_ from @MonteAddMed
@XimenaLevander of @OHSUSOM
And @StefanKertesz from @cappi_uab
Lets go!
Kenny Morford from @YaleADM
@_kmullins_ from @MonteAddMed
@XimenaLevander of @OHSUSOM
And @StefanKertesz from @cappi_uab
Lets go!

3/*Tired of docs who don’t know anything about addiction?
Internal Medicine resident training in addiction WILL be required starting 7/1/22, –
But this paper finds some training but only 12% include addiction med clinic time
pubmed.ncbi.nlm.nih.gov/34729698/
Internal Medicine resident training in addiction WILL be required starting 7/1/22, –
But this paper finds some training but only 12% include addiction med clinic time
pubmed.ncbi.nlm.nih.gov/34729698/

4/Poll question:
When we taper opioid doses on stable patients with pain, the current retrospective, observational reports suggest that makes our patient
When we taper opioid doses on stable patients with pain, the current retrospective, observational reports suggest that makes our patient
5/We highlighted a @JAMA_current paper by @alicia_agnoli. The authors compared outcomes (overdose, withdrawal, mental crises) among persons subject to 15% dose reduction or not
jamanetwork.com/journals/jama/…
jamanetwork.com/journals/jama/…

6/Among 113,618 patients, the 18.2% who tapered had a 1.3x increased risk of overdose and 1.7x increased risk of mental health crises, compared to those who did not. Strength of "causal inference" is limited by observational design.
Still: it’s important to be aware of this
Still: it’s important to be aware of this

7/*OUD medications at time of surgery*
Did you know that when a patient on bupe for OUD goes for a surgery, they should *NOT* have that med stopped?
This VA paper that found 66% have doses held around the time of surgery. This should be corrected
pubmed.ncbi.nlm.nih.gov/34545469/
Did you know that when a patient on bupe for OUD goes for a surgery, they should *NOT* have that med stopped?
This VA paper that found 66% have doses held around the time of surgery. This should be corrected
pubmed.ncbi.nlm.nih.gov/34545469/

8/Which do patients being treated for opioid use disorder (in a randomized trial) tend to prefer?
9/This RCT randomly assigned patients with OUD to treatment with sublingual versus subcutaneous depot BUPE. @JAMANetworkOpen
Treatment satisfaction was high in both groups (>70% on a 100-point scale) but actually higher in the depot injection group!
jamanetwork.com/journals/jaman…
Treatment satisfaction was high in both groups (>70% on a 100-point scale) but actually higher in the depot injection group!
jamanetwork.com/journals/jaman…

10/*Alcoholism Recovery*
Should it count as “recovery” if a person
still drinks after treatment, and does so heavily on occasion?
This study by @KatieWitkiewitz says “yes," but THAT triggered "lively" editorial debate in @JAM_ASAM
journals.lww.com/journaladdicti…
Should it count as “recovery” if a person
still drinks after treatment, and does so heavily on occasion?
This study by @KatieWitkiewitz says “yes," but THAT triggered "lively" editorial debate in @JAM_ASAM
journals.lww.com/journaladdicti…

11/Among n=149 who got treatment for alcohol problems 10 years before, 4 groups sorted out at 3 years, based on drinking 🍷 & function (fxn)
low fxn, frequent heavy 🍷
low fxn, infrequent heavy
high fxn, occasional heavy 🍷
high fxn, infrequent non-heavy 🍷
low fxn, frequent heavy 🍷
low fxn, infrequent heavy
high fxn, occasional heavy 🍷
high fxn, infrequent non-heavy 🍷
12/The high-functioning groups, included one that drank on *51% of their days*
The 2 higher functioning had higher purpose in life and lower depression
The authors suggest this calls for new thinking on recovery
The 2 higher functioning had higher purpose in life and lower depression
The authors suggest this calls for new thinking on recovery

13/Editorialists John Kelly and Brandon Bergman called this “a Bridge too far” (see image)
The authors, however, say that criticism delivers a “Bridge to Nowhere”
journals.lww.com/journaladdicti…
The authors, however, say that criticism delivers a “Bridge to Nowhere”
journals.lww.com/journaladdicti…

14/Hey doc, have you thought of Rx'ing *STATINS for alcoholic liver disease?
In a study of Taiwanese patients with alcohol use disorder, those on statins were at ⬇️ risk of decompensated liver cirrhosis & of hepatocellular carcinoma! @drugalcoholdep sciencedirect.com/science/articl…
In a study of Taiwanese patients with alcohol use disorder, those on statins were at ⬇️ risk of decompensated liver cirrhosis & of hepatocellular carcinoma! @drugalcoholdep sciencedirect.com/science/articl…

15/How you known someone (patient, friend or family) whose liver failed, and where they couldn't get a liver transplant partly because they hadn't stopped drinking?
16/*Liver Transplant without 6 months abstinence?*
At Johns Hopkins U:
Comparing 88 “early” transplants to 75 “standard” ones, with “early” ones were picked after _careful multidisciplinary review_
Outcomes were similar for both groups @JAMASurgery
jamanetwork.com/journals/jamas…
At Johns Hopkins U:
Comparing 88 “early” transplants to 75 “standard” ones, with “early” ones were picked after _careful multidisciplinary review_
Outcomes were similar for both groups @JAMASurgery
jamanetwork.com/journals/jamas…
17/Maybe a med for methamphetamine use disorder?
This @nejm RCT of im naltrexone 380 mg q3weeks & buproprion 450 mg/day found it worked in a minority (13.6% response rate, vs 2.6% placebo)
So- these meds *help*, but remission occurred in a minority nejm.org/doi/full/10.10…
This @nejm RCT of im naltrexone 380 mg q3weeks & buproprion 450 mg/day found it worked in a minority (13.6% response rate, vs 2.6% placebo)
So- these meds *help*, but remission occurred in a minority nejm.org/doi/full/10.10…

18/🚬🚬🚬
"I can't stop, doc" 😔
👨🏽⚕️"Have you considered vaping?"
This trial in @AddictionJrnl randomly assigned 68 smokers to Nicotine Replacement Treatment (NRT) vs 67 to e-cigarettes
Smoking reduction achieved by 26.5% (e-cigs)
versus 6.0% (NRT)
onlinelibrary.wiley.com/doi/full/10.11…
🚬
"I can't stop, doc" 😔
👨🏽⚕️"Have you considered vaping?"
This trial in @AddictionJrnl randomly assigned 68 smokers to Nicotine Replacement Treatment (NRT) vs 67 to e-cigarettes
Smoking reduction achieved by 26.5% (e-cigs)
versus 6.0% (NRT)
onlinelibrary.wiley.com/doi/full/10.11…
🚬

19/ *We can treat Hep C even when our patient uses iv drugs, actually*
N=61 with opioid use disorder + Hep C
59% used drugs *during* HCV treatment
3 different administration routes.
98% achieved sustained remission! @NIDAnews
@ijdrugpolicy
pubmed.ncbi.nlm.nih.gov/33667826/
N=61 with opioid use disorder + Hep C
59% used drugs *during* HCV treatment
3 different administration routes.
98% achieved sustained remission! @NIDAnews
@ijdrugpolicy
pubmed.ncbi.nlm.nih.gov/33667826/

20/*One way to PREVENT local hepatitis C in a community is to TREAT hepatitis C*
In🏴 they compared Tayside (which ramped up community offer of direct acting antiviral therapy) to the rest, with a BIG ⬇️ in HCV in Tayside users. @AddictionJrnl
onlinelibrary.wiley.com/doi/10.1111/ad…
In🏴 they compared Tayside (which ramped up community offer of direct acting antiviral therapy) to the rest, with a BIG ⬇️ in HCV in Tayside users. @AddictionJrnl
onlinelibrary.wiley.com/doi/10.1111/ad…

21/In the US drug poisoning/overdose crisis, which group has recently emerged to have the highest per capita overdose/poisoning death rate?
22/Per capita, AmericanIndians, Alaska Natives & Blacks now suffer opioid-involved OD deaths at higher rates than Whites
This is a complex story we approached through several 2021 papers
@JAMAPsych
jamanetwork.com/journals/jamap…
This is a complex story we approached through several 2021 papers
@JAMAPsych
jamanetwork.com/journals/jamap…
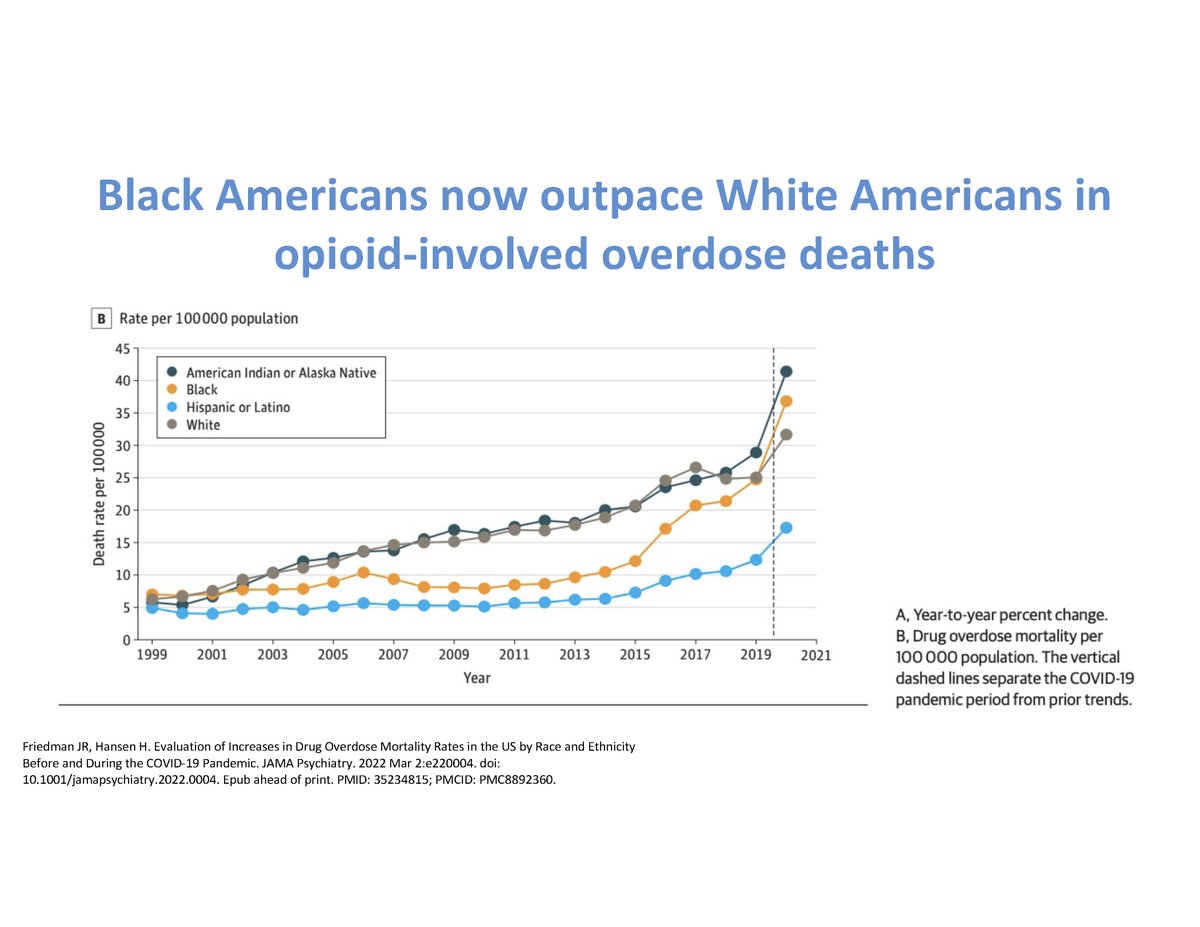
23/Treatment of OUD with meds, Bupe in particular, is lower for Blacks vs Whites, despite rising ODs for Blacks.
This PA study suggests jail and ER experience are associated with ⬇️ chances of getting meds, which may hint at key touchpoint
doi.org/10.1016/j.drug…
This PA study suggests jail and ER experience are associated with ⬇️ chances of getting meds, which may hint at key touchpoint
doi.org/10.1016/j.drug…

24/Getting MD's a "bupe waiver" is *not* sufficient
Most US bupe prescribers treat no more than 1-2 patients a month. Many stop entirely.
There are terrible gaps in training, our support for clinics & reimbursement @papergirlmacy @BradleyDStein
rand.org/pubs/external_…
Most US bupe prescribers treat no more than 1-2 patients a month. Many stop entirely.
There are terrible gaps in training, our support for clinics & reimbursement @papergirlmacy @BradleyDStein
rand.org/pubs/external_…

25/Offering hospital-based inpatient addiction consultation services are associated with which of the following outcomes?
26/Inpatient hospital consultation for addiction is associated with 2.35% decreased all-cause mortality in a case control analysis of patients from @PittGIM @liebschutz 
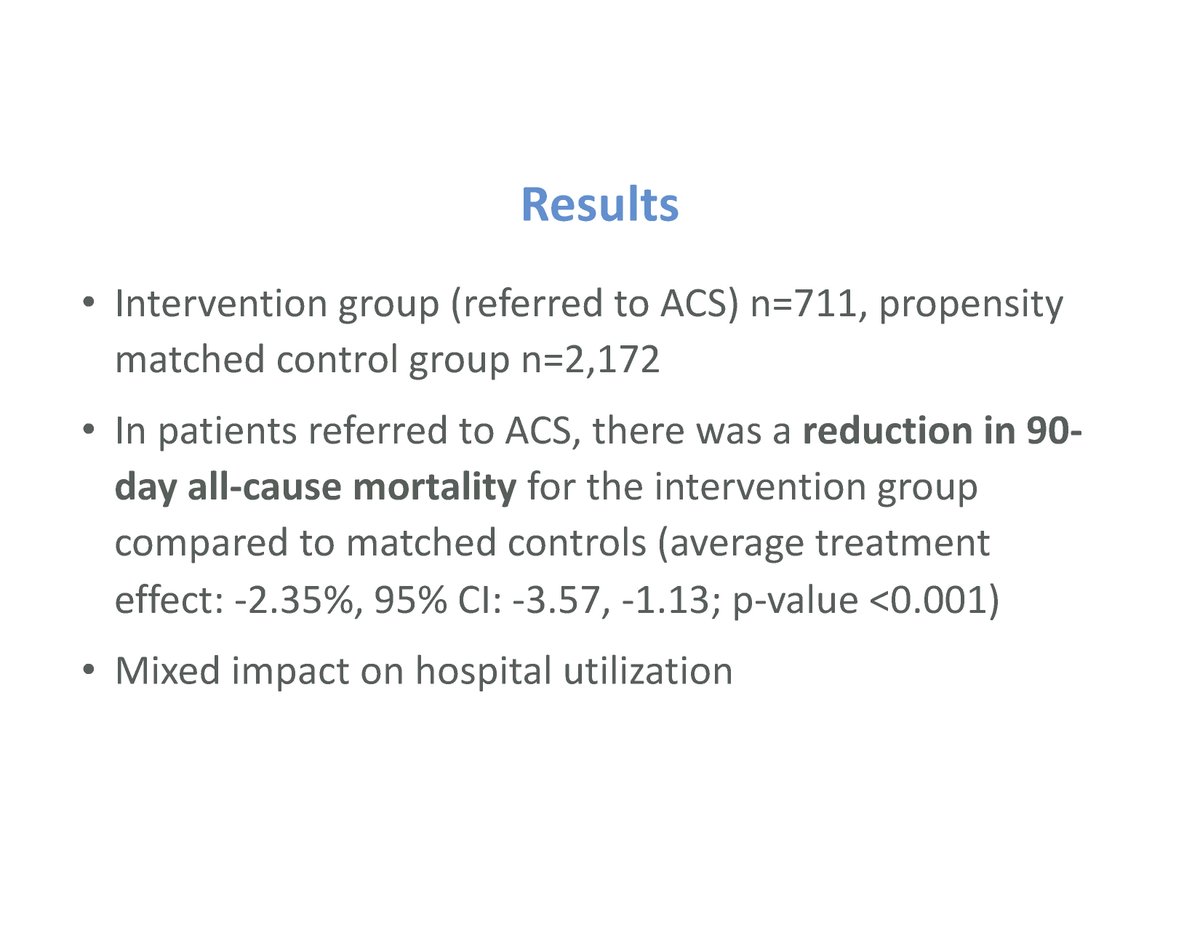
27/"What a difference a day makes"
For hospitalized patients with medical issues and opioid use disorder, does your hospital refer to outpatient addiction clinic?
Extending wait time by 1 day reduces chance of a patient showing up from 63%
to 42%.
pubmed.ncbi.nlm.nih.gov/33964730/
For hospitalized patients with medical issues and opioid use disorder, does your hospital refer to outpatient addiction clinic?
Extending wait time by 1 day reduces chance of a patient showing up from 63%
to 42%.
pubmed.ncbi.nlm.nih.gov/33964730/

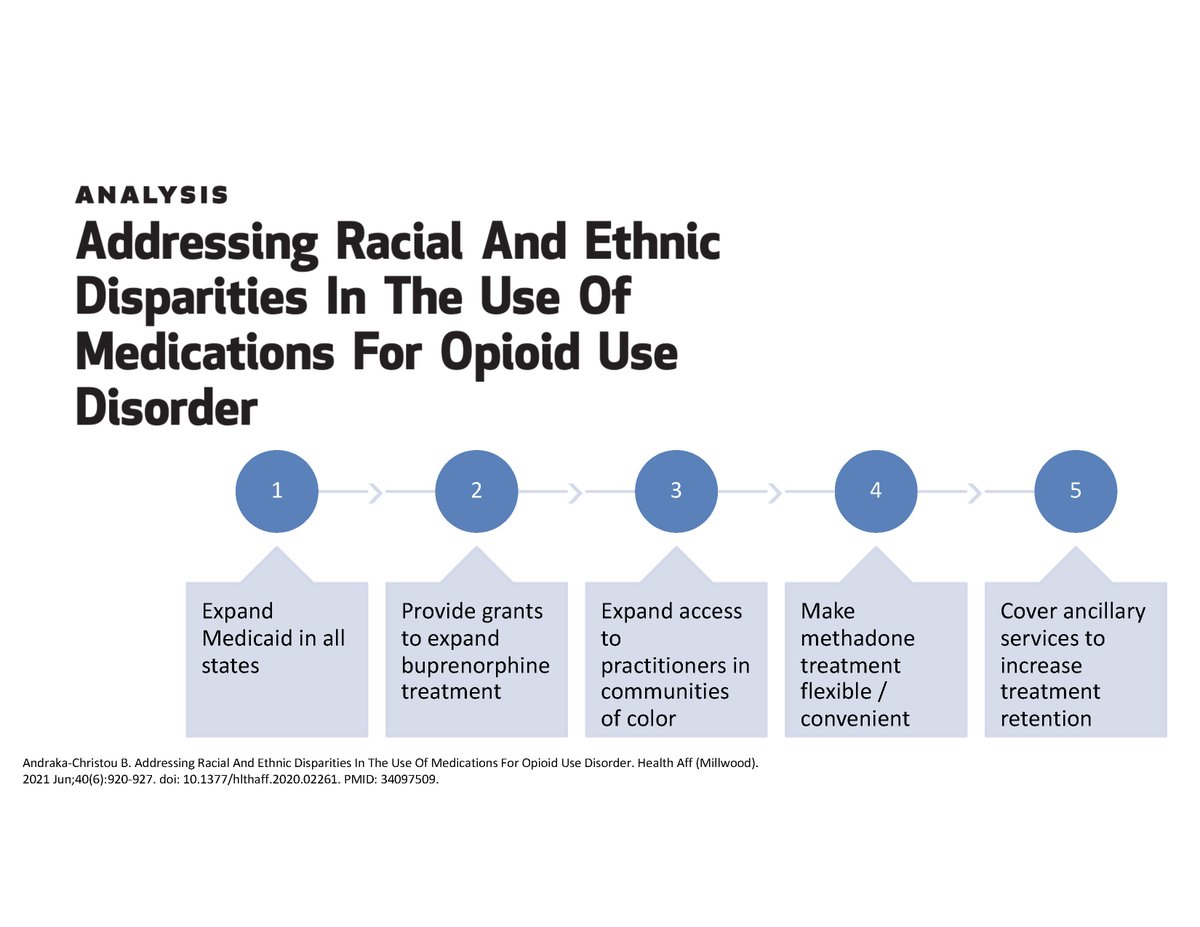
28/Just 1/5 of patients with OUD get medication for it.
That lifesaving care is currently accessed more by Whites than people of color, despite higher overdose rates in the latter group.
What could we do?
Dr. @AndrakaBasia wrote in @Health_Affairs :
healthaffairs.org/doi/10.1377/hl…
That lifesaving care is currently accessed more by Whites than people of color, despite higher overdose rates in the latter group.
What could we do?
Dr. @AndrakaBasia wrote in @Health_Affairs :
healthaffairs.org/doi/10.1377/hl…

29/Issues that make OUD treatment less available to Blacks than White are numerous, writes @AndrakaBasia. Treatment facilities in Black communities are less likely to offer any medication. And Bupe prescribers are less likely to accept Medicaid.
30/This new piece on disparities also drew my own attention, by @MaxJordan_N
He notes that because methadone programs are seen as “a problem” for neighborhoods, they have been disproportionately put in Black/Brown neighborhoods with ⬇️ political pushback
journalofsubstanceabusetreatment.com/article/S0740-…
He notes that because methadone programs are seen as “a problem” for neighborhoods, they have been disproportionately put in Black/Brown neighborhoods with ⬇️ political pushback
journalofsubstanceabusetreatment.com/article/S0740-…
31/Methadone is quite effective but 🇺🇸clinics are set up a lot more like a criminal justice supervision programs (compared to, for example, 🇨🇦), reinforcing distrust of the recipients. Both @MaxJordan_N and @AndrakaBasia urge making this treatment less burdensome
32/A summary of paths to address racial and ethnic disparities are graphically depicted below.
I should emphasize: NO ONE thinks that we have anything close to adequate addiction treatment access for Whites, Blacks or anyone else at this time
healthaffairs.org/doi/10.1377/hl…
I should emphasize: NO ONE thinks that we have anything close to adequate addiction treatment access for Whites, Blacks or anyone else at this time
healthaffairs.org/doi/10.1377/hl…
33/A clarification here- we reviewed as a team for a mere 60 minute session at the @SocietyGIM #SGIM22 meeting.
If you see there are MAJOR articles from 2021 we could not include, we agree.
It was tough, but we emphasized what general internists tend to need.
If you see there are MAJOR articles from 2021 we could not include, we agree.
It was tough, but we emphasized what general internists tend to need.
34/For folks who are interested in learning more about this session, please note we did a @thecurbsiders podcast right after the session. It should come out in a month or two. There are a few "preview comments' in this recent episode @DoctorWatto pod.link/1198732014/epi…
35/Finally, I have to thank the amazing co-presenters. My first "Update in Addiction Medicine" was led by @AJ_Gordon in 2006 or so. This was probably my second? Well, guess what: a lot changed and the amazing Kenny Morford , @XimenaLevander and @_kmullins_ taught me a lot 

36/Post-final finally- thank you to @DrPoorman for showing me how to use polling tweets get people into a review of a medical topic
• • •
Missing some Tweet in this thread? You can try to
force a refresh