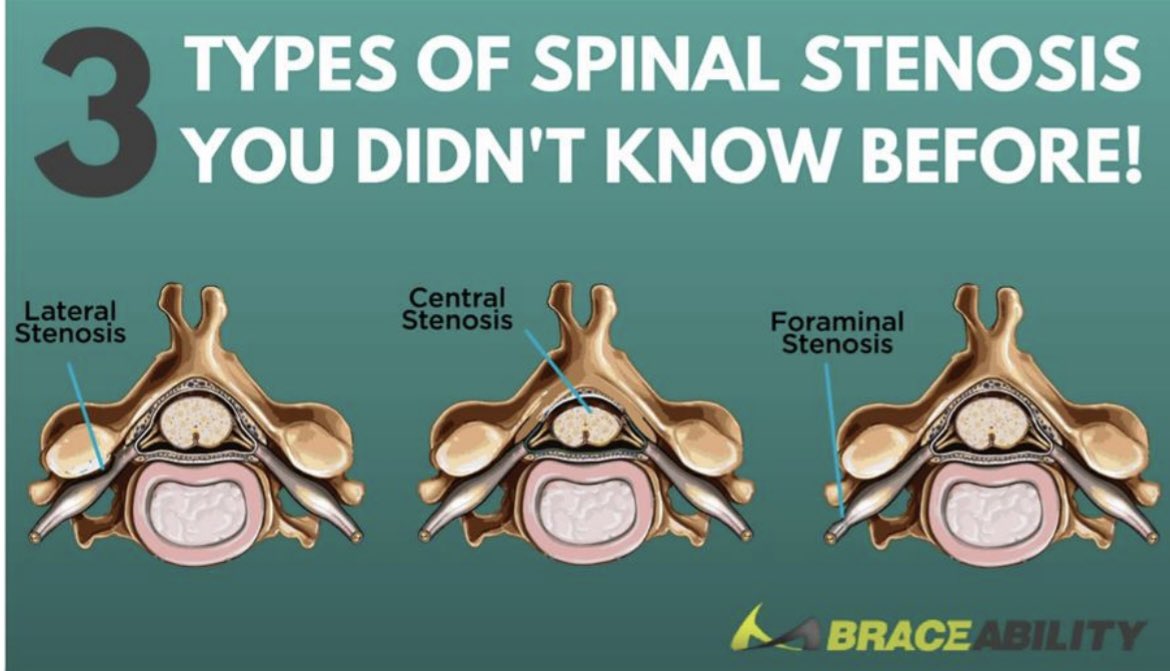
2) LSS is defined as narrowing of the spinal canal +/- neural foramina which causes crowding around the exiting caudal nerve roots with compression & ischaemia due to progressive, age related changes to the anatomical structures of the spine. 

3) Epidemiology: approx 103 million people suffer with symptomatic LSS with 20% of > 60yrs suffering with it, yet 80% are thought to be asymptomatic (Katz et al., 2022). Other research found a higher prevalence and ? 45-60% of adults >65yrs (Comer et al., 2020). 

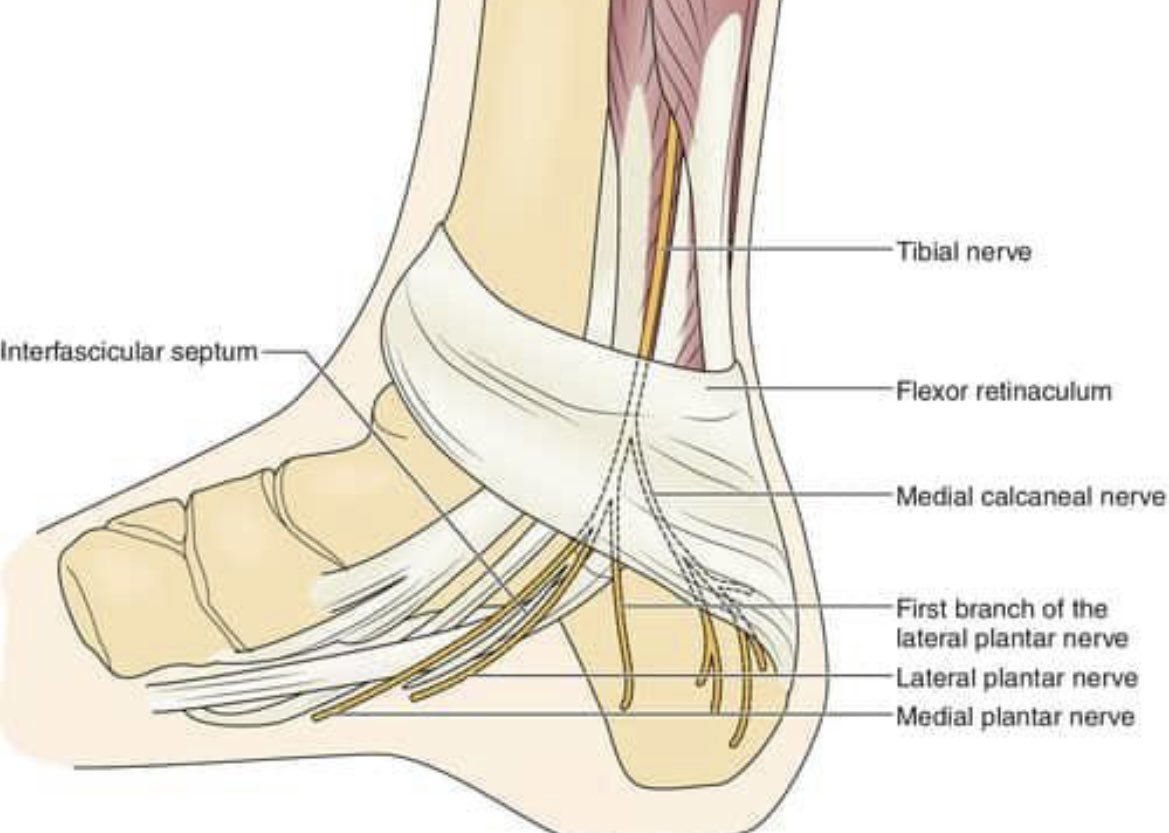
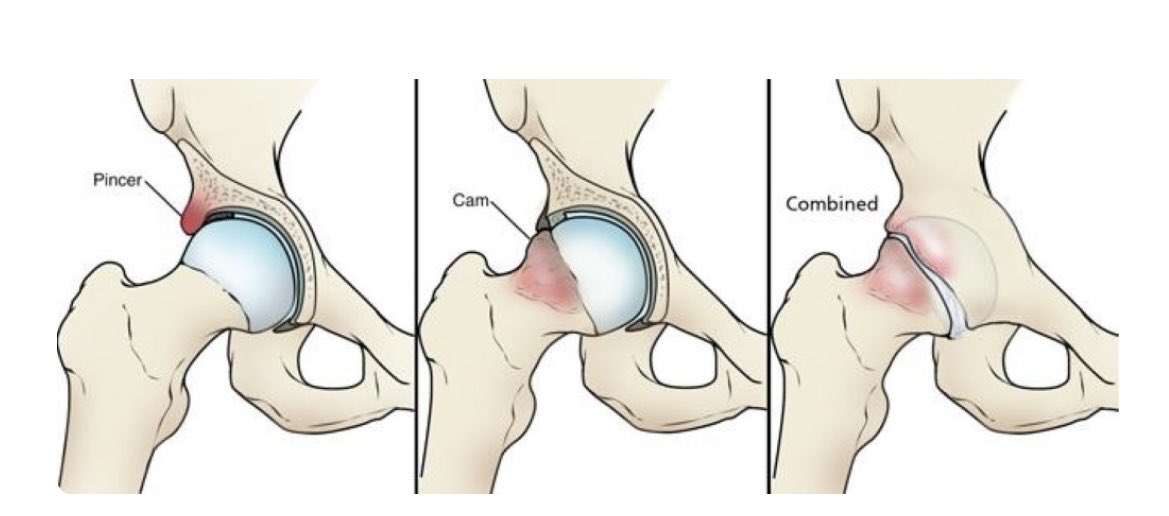
4) Pathophysiology; DDD puts greater load on posterior facet joints which alongside the ligaments hypertrophy and this encroaches on surrounding nerves. Pain is thought to be from ischaemia to small arterioles of the nerve +/- venous congestion. Most common is L4/5 (Lee et al 20)
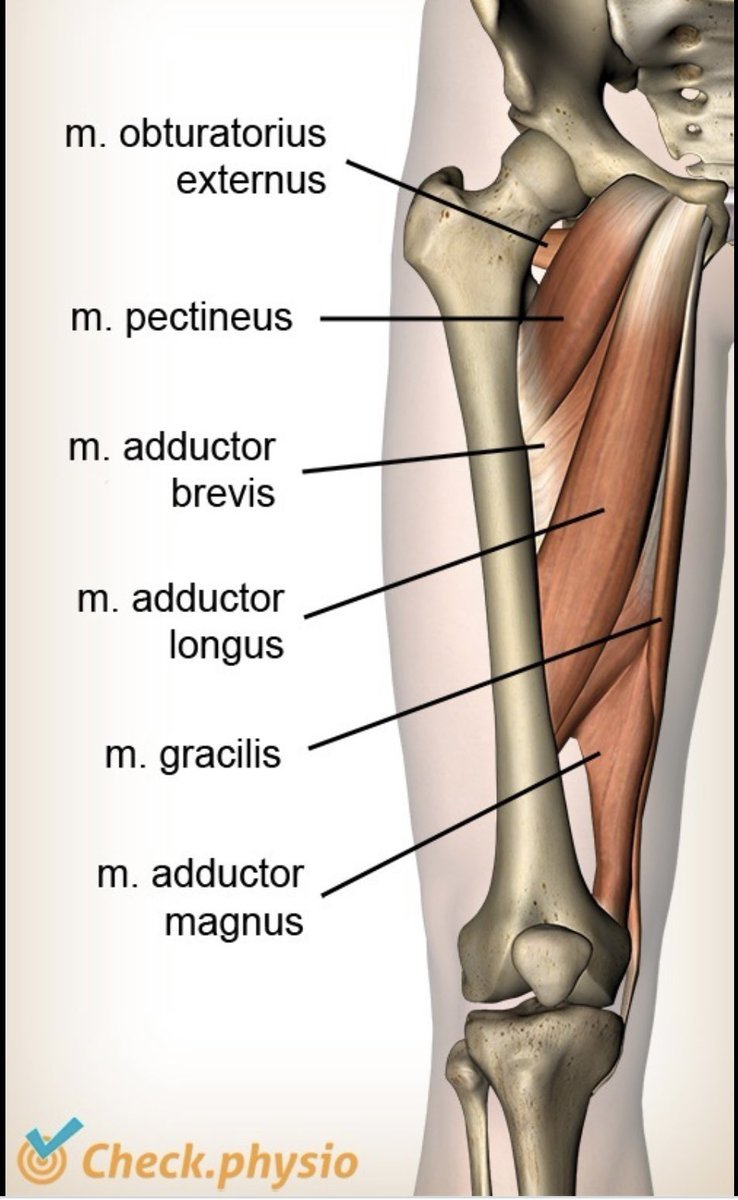
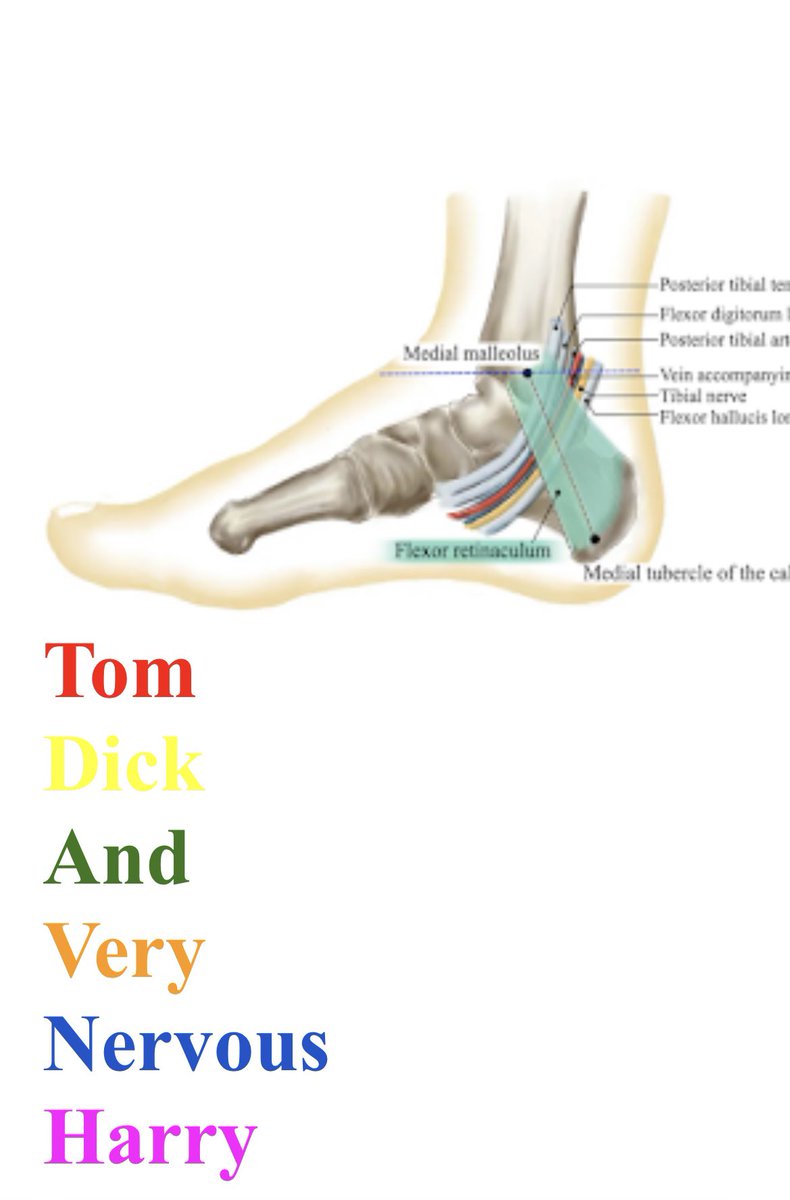
5) Features; UL/BL pain in the LL (rarely the feet). Sx relief w flexion or walking flexed. LBP, neuro Sx when walking or standing for long period & normal symmetrical dorsalis pedis pulses (Genevay et al., 2018). Chronic Sx can impede balance & mobility.
6) Diagnosis: Can be made through clinical assessment. Previously Cluster of Cook was found to have a high LR if pt’s had 4/5 (Cook et al 2011). More recently N-Class Criteria (see pictures) has been proposed but there is little research on its psychometric properties. 

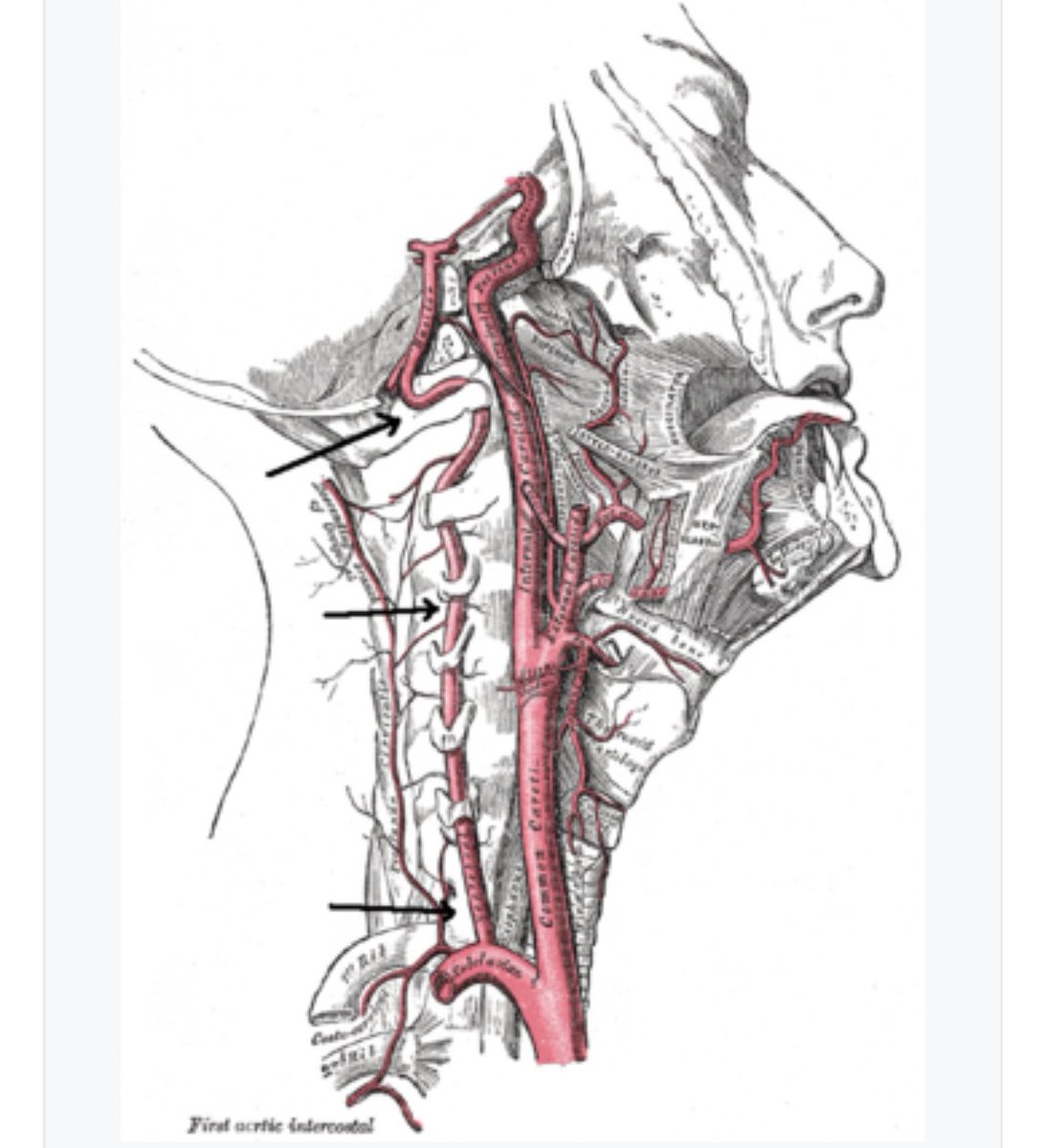
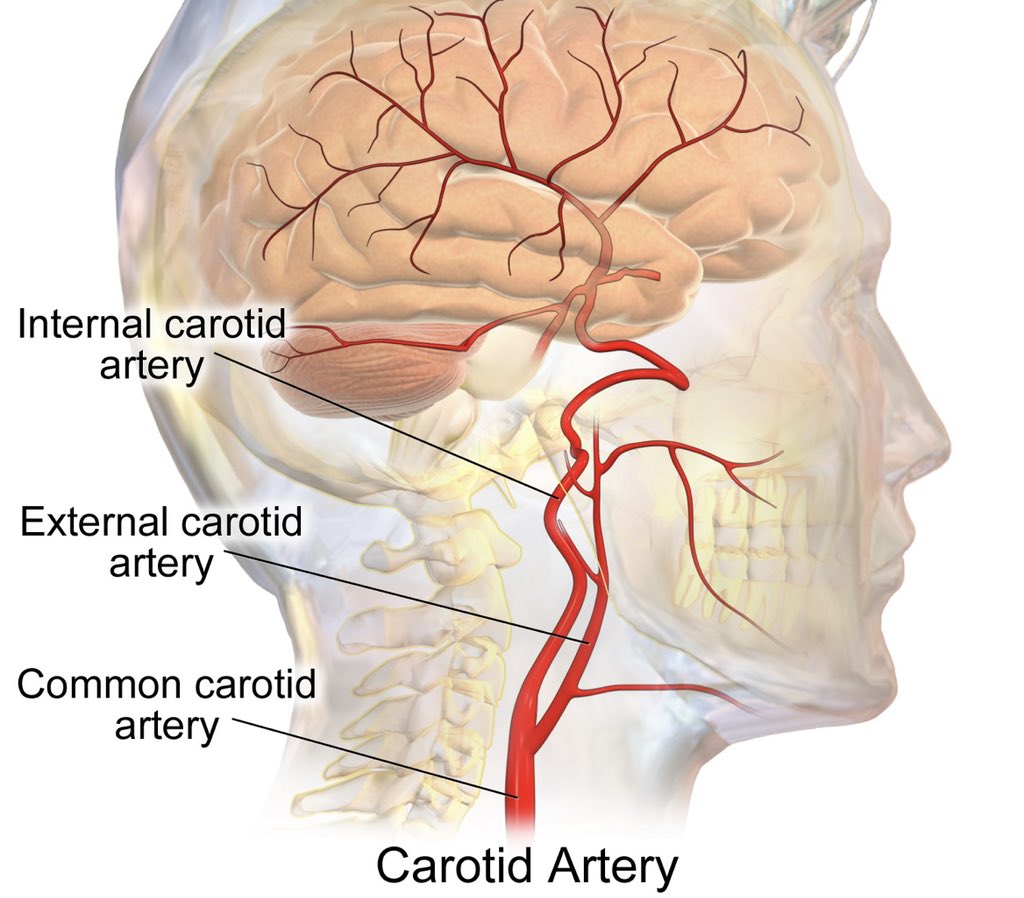
7) PAD - a differential Dx which can elicit similar Sx. Clinicians should be aware of vascular comorbidities, smoking Hx & physically assess for LL oedema / skin integrity, pulses & Buerglers. Sx will be provoked irrespective of spinal position w PAD’s during exertion (Bike Test) 

8) Imaging - low correlation between Sx & findings. Utilise for pt’s with persistent Sx that are impeding function. MRI can be used to assess the diameter of the spinal canal. CT w myelogram can provide more accurate info w dynamic positions (flex vs ext) - Lee et al., 2020. 

9) Prognosis: A study of 146 pt’s found a 1/3 improved, 50% remained ISQ & 10-20% became worse with symptoms at 3yr f/u (Wessberg et al., 2017).
researchgate.net/publication/31…
researchgate.net/publication/31…
10) Treatment; Host of different techniques. There has been some low evidence supporting the use of cycling, aquatic & supported treadmill walking. This is thought to increase the CSA of the canal and reduces axial loading on the spine. For further info this paper is great. 

11) Surgery; Should only be considered when significant disability and no improvement with Rx. 10-24% can suffer complications post-decompression (Temporiti et al 2022). Those with concomitant scoliosis / spondylolithesis may require fusion to prevent spinal instability.
• • •
Missing some Tweet in this thread? You can try to
force a refresh