
63. For Part 4 of our #Tweetorial on the basics of mechanical circulatory support (MCS) we will look at some case examples and clinical indications. 🏥
Follow along below ⬇
Follow along below ⬇
64. This 71 yo man had chest pain, shortness of breath, and inferior STEMI & based on BP has what looks like an RV infarct. Treatment began with IV fluids, and vasopressors but BP remains low & HR is actually low for the condition. What do you do? 🤒 

65. I know some have used left-sided Impella for this type of shock patient with RV infarct, but I would not choose this path as unloading the LV would not help without RV function. 

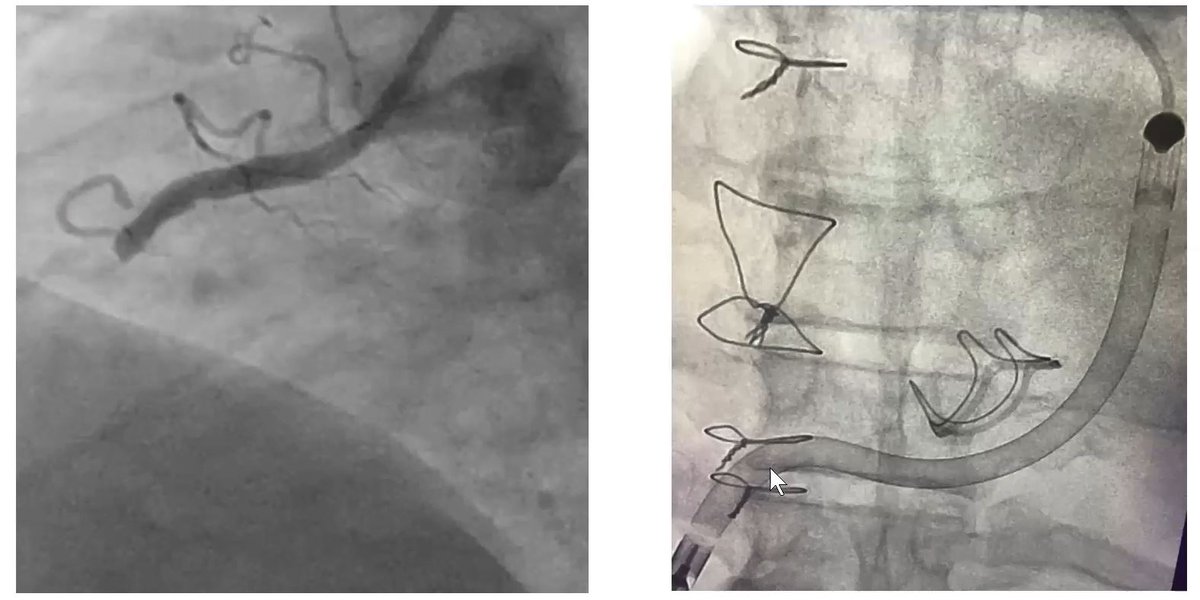
66. This patient continued to be in shock. Here we see the occluded RCA of the STEMI. RV infarct shock needed RV support. In this case, Impella RP. You can see it go up the RA, through the RV & into the PA. The device provided very good RV support. 
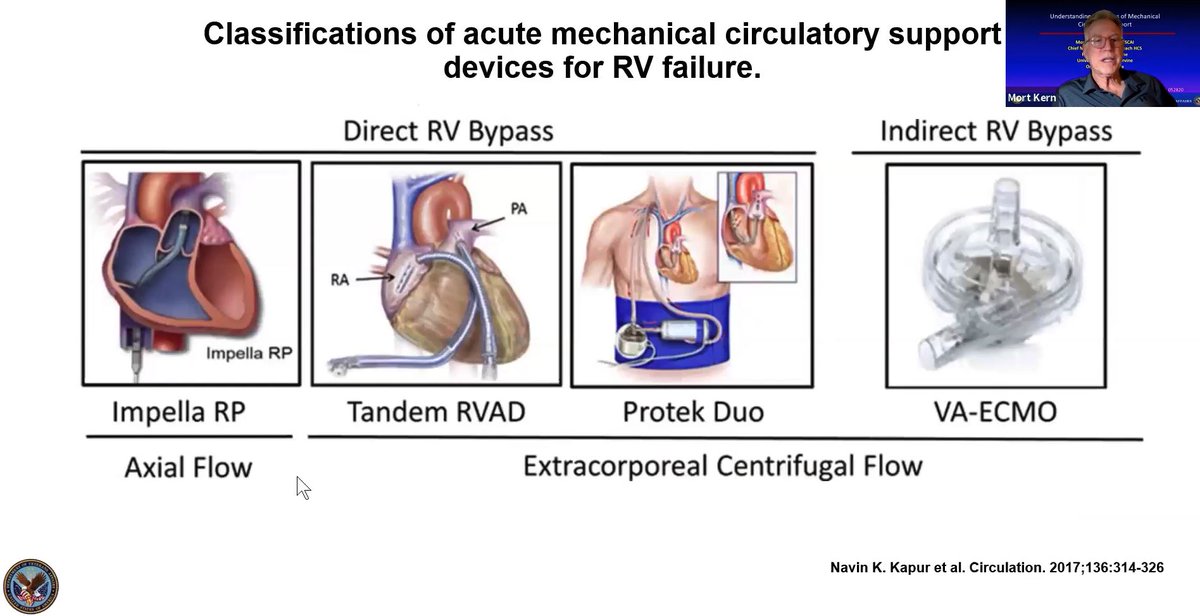
67. There are other devices that can provide RV support and “direct RV bypass” as well They are a little more complicated, but they are all effective. ⚙ 
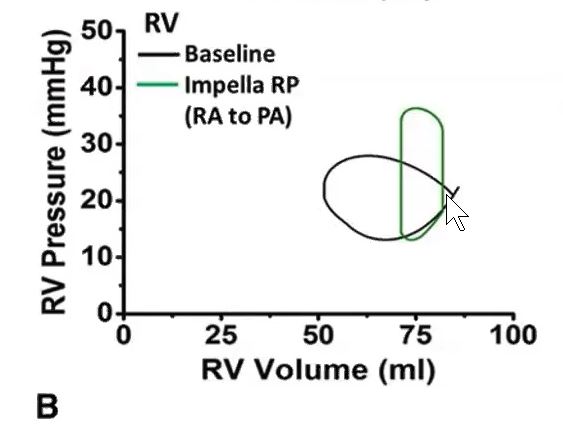
68. The heart in shock behaves differently when the RV is involved. Here we will look at biventricular hemodynamics when a right-sided Impella is placed. The RV pressure-volume loop is different and unique from the left side. 👉🔁 
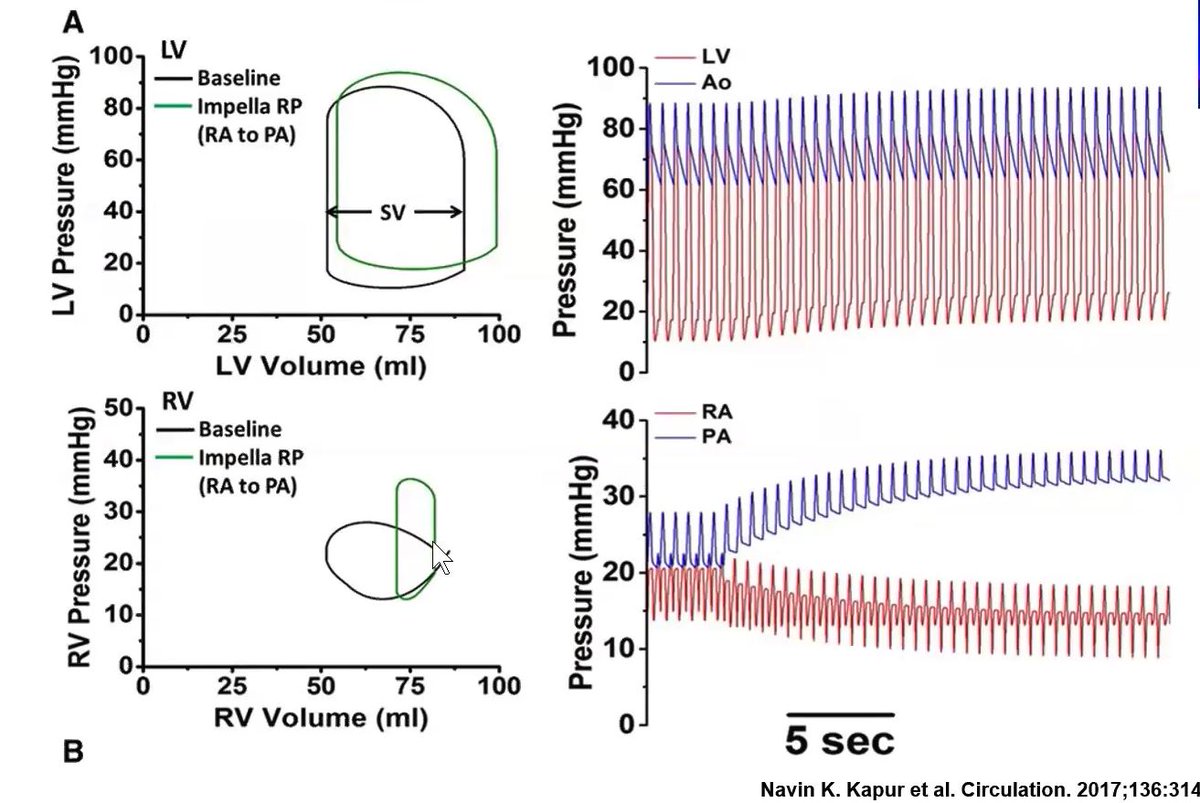
69. For the RV, normally the PV loop is ovoid in shape. When the Impella is implanted a rectangular PV curve returns. Remember, ejection goes up, the end-systolic point moves to the left, and isometric relaxation improves, but the same diastolic filling pattern remains. 
70. When the Impella RP is working, the hemodynamics show a decrease in RA pressure from 20 to 15 while PA pressure goes up. The pulse pressure remains low, despite the fact that the pulmonary pressure is going up. 📈 
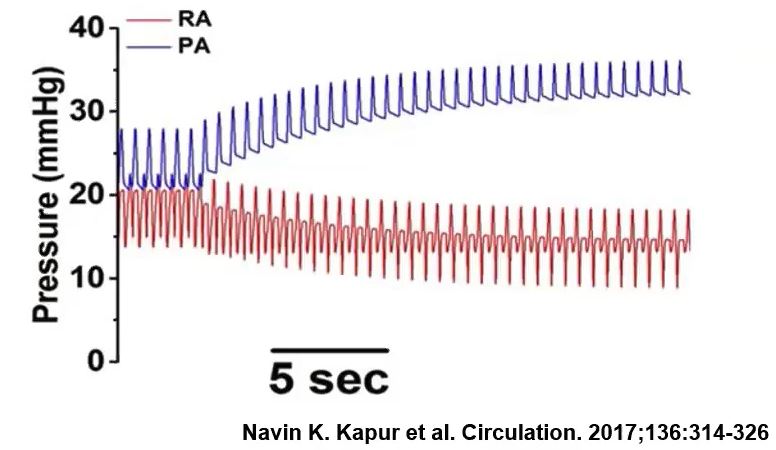
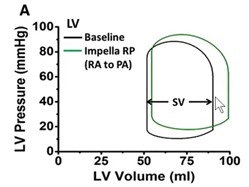
71. The effect of the Impella RP also improves left-sided hemodynamics. Stroke volume for the LV gets bigger & pressure goes up because you are improving the delivery of blood to the left side of the heart which was impaired by the RV dysfunction. 💓 
72. We will conclude by focusing on clinical indications. I am a proponent of early support for cardiogenic shock because of the negative effects that the hemo-metabolic derangements produce early. Support the patient early with unloading then proceed to reperfusion, etc. ⏳ 
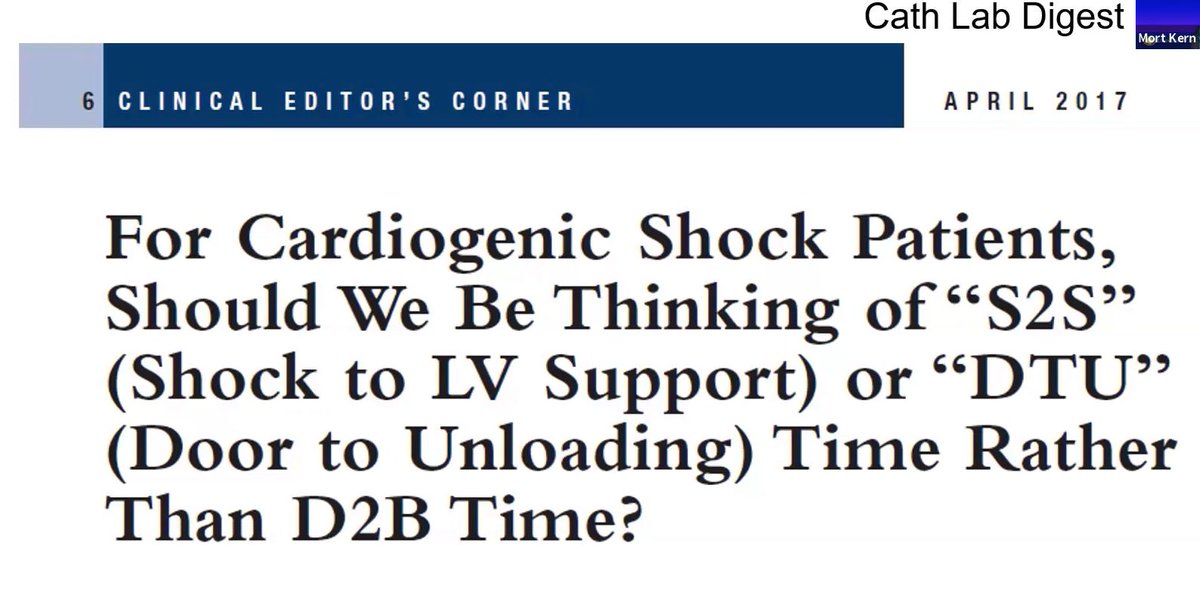
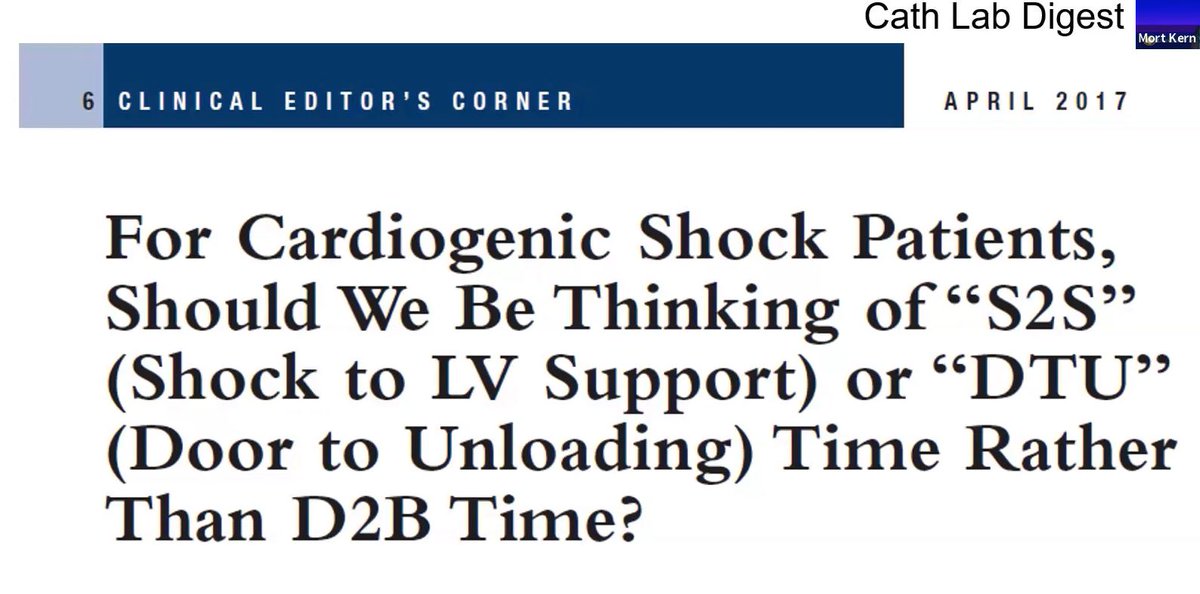
73. Along with @DougDrachmanMD & @BillONeillMD I think they make a strong case for door-to-unloading time 🚪👉⛽ as a benefit over door-to-balloon time 🎈 – in shock patients ⚡. 
74. Early data supports this approach. 3 studies show early Impella has better outcomes & improved survival in these very sick patients. The Detroit shock initiative (NCSI) also supports this approach. 📊 

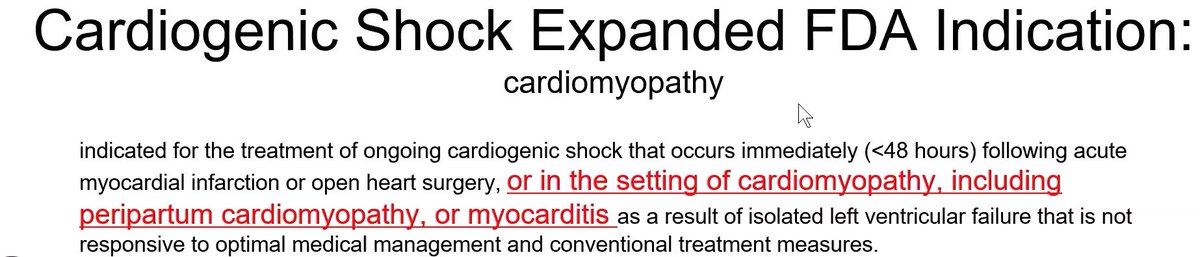
75. The FDA expanded indication for use in patients with cardiogenic shock for Impella, including cardiomyopathy, peripartum cardiomyopathy, or myocarditis. ⚙⛽ 
76. Keep in mind the limitations of implantation time (about 7 minutes) & vascular access. Nonetheless, this device will support the heart for recovery or bridge to transplant. 💞
77. To date shock studies have been stymied because we have not been able to look at shock patients in a unified way or as an entity that behaves in the same way. The nonsurvivable or futile patient is mixed with survivable patients. 🔀 
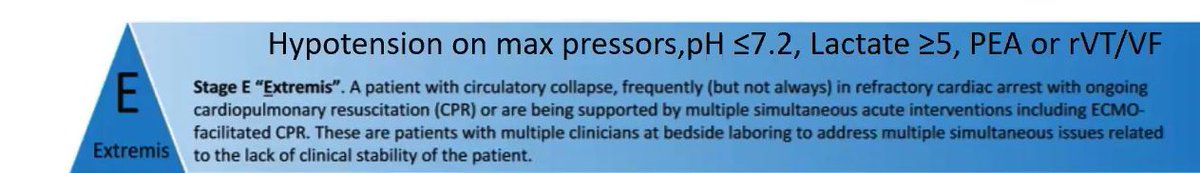
78. The results of comparative MCS studies show no difference when trying to see which device or method will help. Baran & et al at SCAI produced a classification of CGS going from pre-shock to extremis with survival statistics improving with each classification (A to E). 
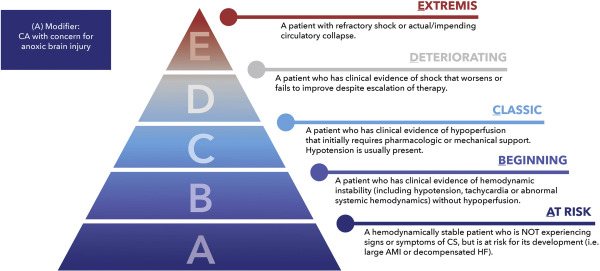
79. Some patients should probably not be randomized into trials because survival with any method will likely be 0. Likewise, others should be excluded from randomization because they will survive with any intervention. 
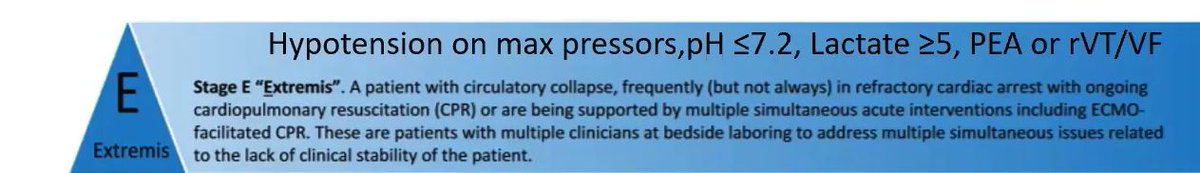
80. We should appreciate the association of shock classes and outcomes. For comparative therapies, we should include similar shock class patients to be included and thus understand the differences in outcomes from their initial clinical presentation and device used. 💭 
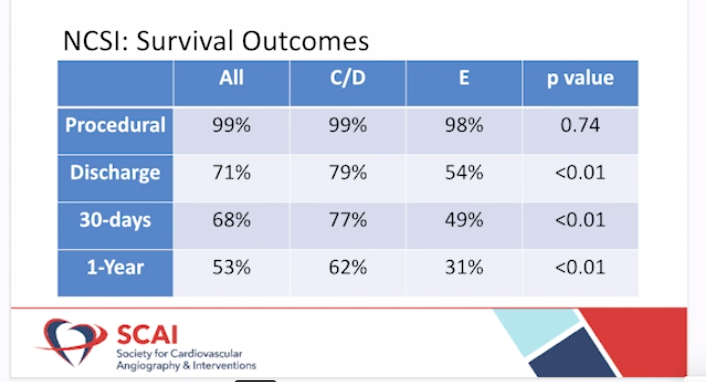
Thank you again for following along with this #Tweetorial.
You can view more of my Hemodynamic Rounds Live series here: wondrmedical.net/ch/HemoDynamic…
@WondrMedical @cardionerd #CardioTwitter @SCAI
You can view more of my Hemodynamic Rounds Live series here: wondrmedical.net/ch/HemoDynamic…
@WondrMedical @cardionerd #CardioTwitter @SCAI
• • •
Missing some Tweet in this thread? You can try to
force a refresh











