Writing an #ECG talk for @ICEM2022 and couldn't find an algorithm for approaching the "fixed" regular narrow complex tachycardia. Thought I would create my own.
#FOAMed @acemonline
#FOAMed @acemonline

@ICEM2022 @acemonline All this talk about VT versus SVT and it seems no one talks about an approach to regular narrow complex tachycardia.
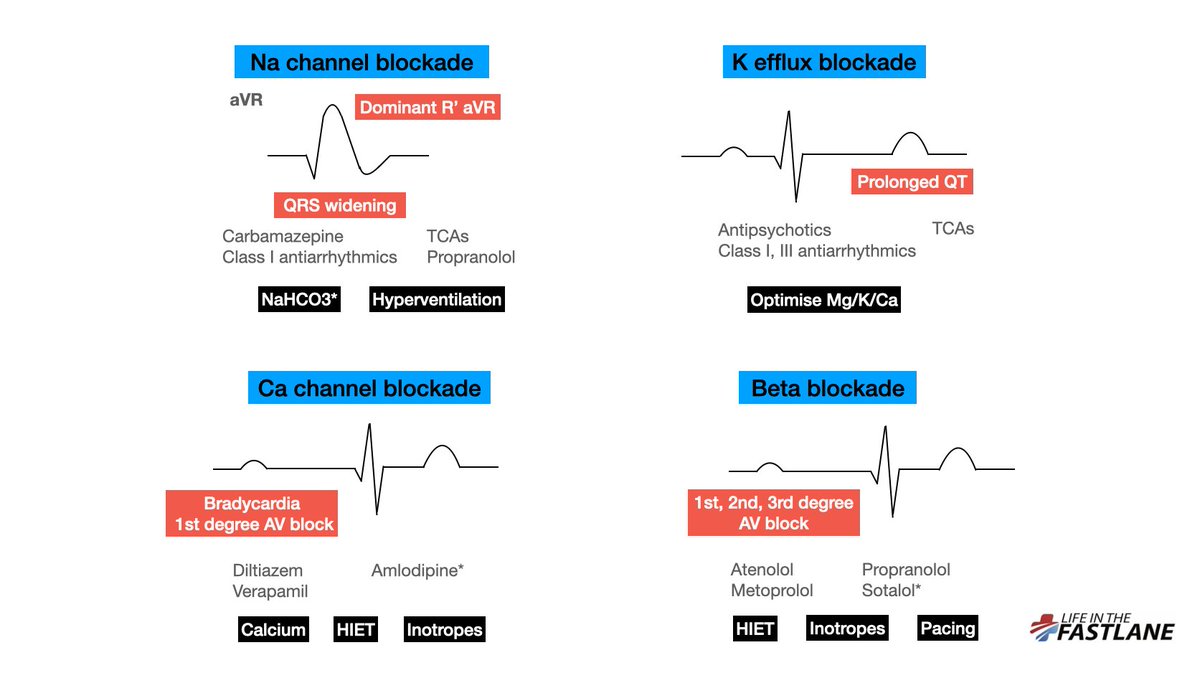
Well, basic principles. Regular narrow complex tachycardias are either re-entrant, automatic, or due to triggered automaticity. (1)
Well, basic principles. Regular narrow complex tachycardias are either re-entrant, automatic, or due to triggered automaticity. (1)
Those due to re-entrant circuits include atrial flutter, AVNRT, orthodromic AVRT, and some focal atrial tachycardias. These are paroxysmal, have a fixed rate, and all respond to electricity (2)
Those due to enhanced automaticity include most focal atrial tachycardias, junctional tachycardia (AJR), and of course sinus tachycardia. These have a gradual onset and exhibit beat-to-beat variability. (3)
The 3 questions I ask myself in any regular narrow complex tachycardia:
1) Sudden versus gradual onset?
2) Beat-to-beat variability?
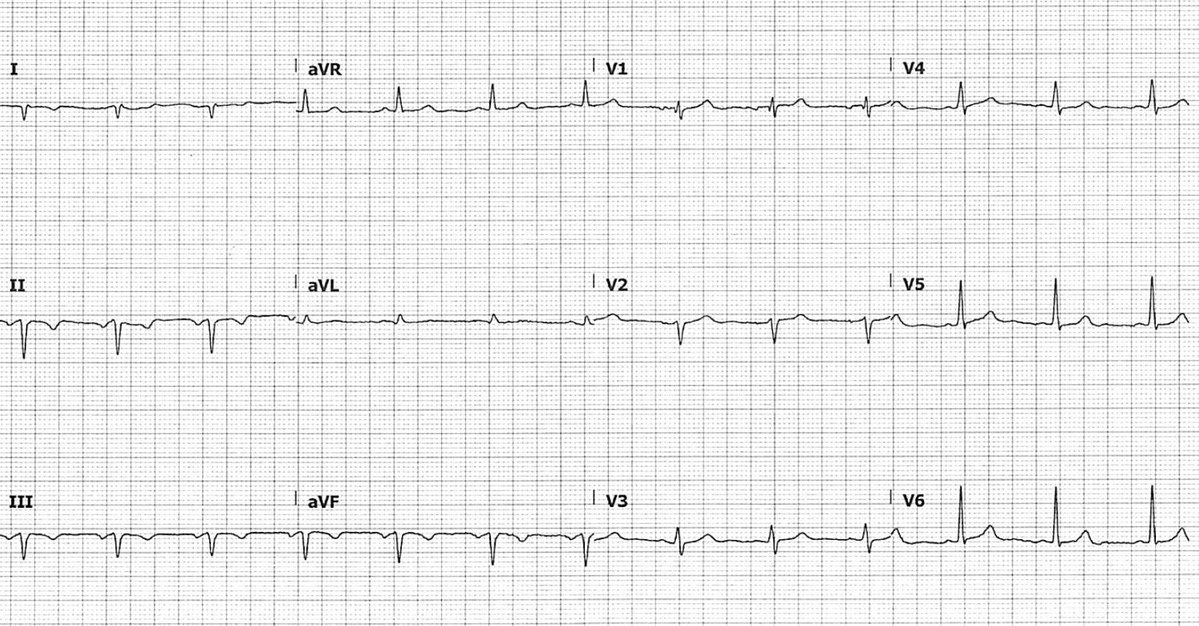
3) Presence, location (R-P interval), and morphology of P waves?
Oh, and don't forget to look for STE suggestive of underlying infarction (4)
1) Sudden versus gradual onset?
2) Beat-to-beat variability?
3) Presence, location (R-P interval), and morphology of P waves?
Oh, and don't forget to look for STE suggestive of underlying infarction (4)
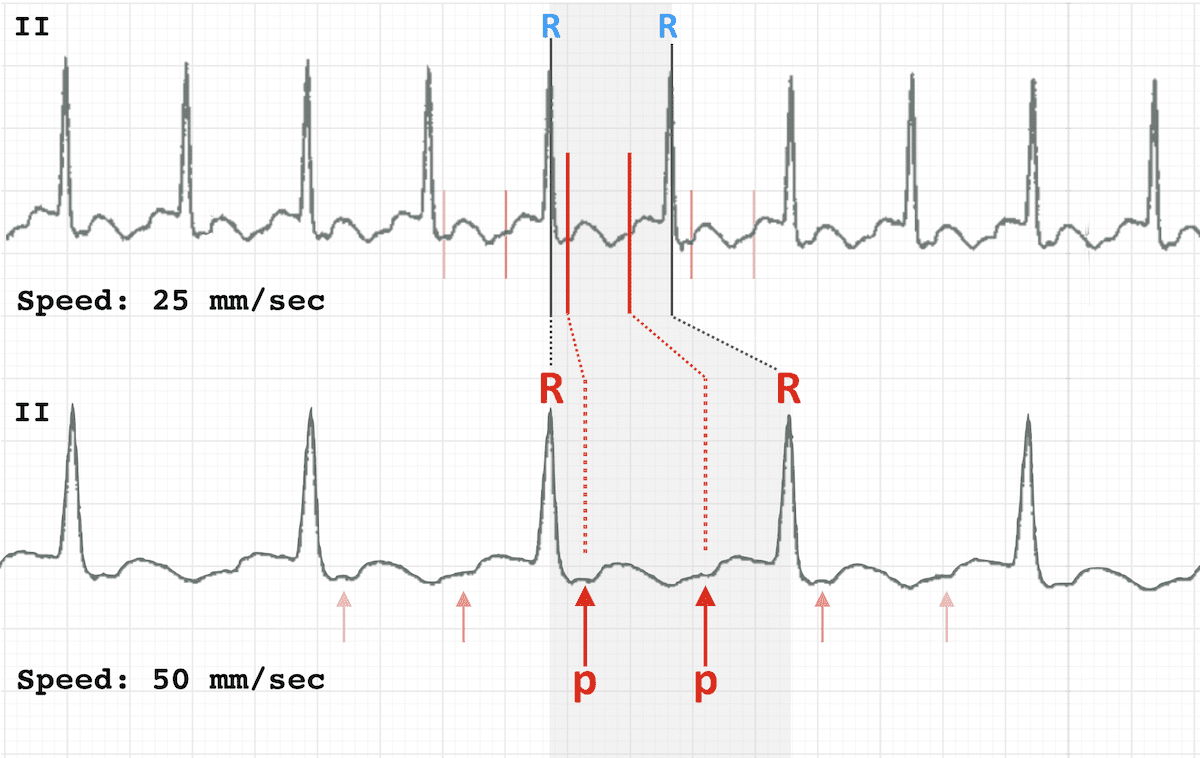
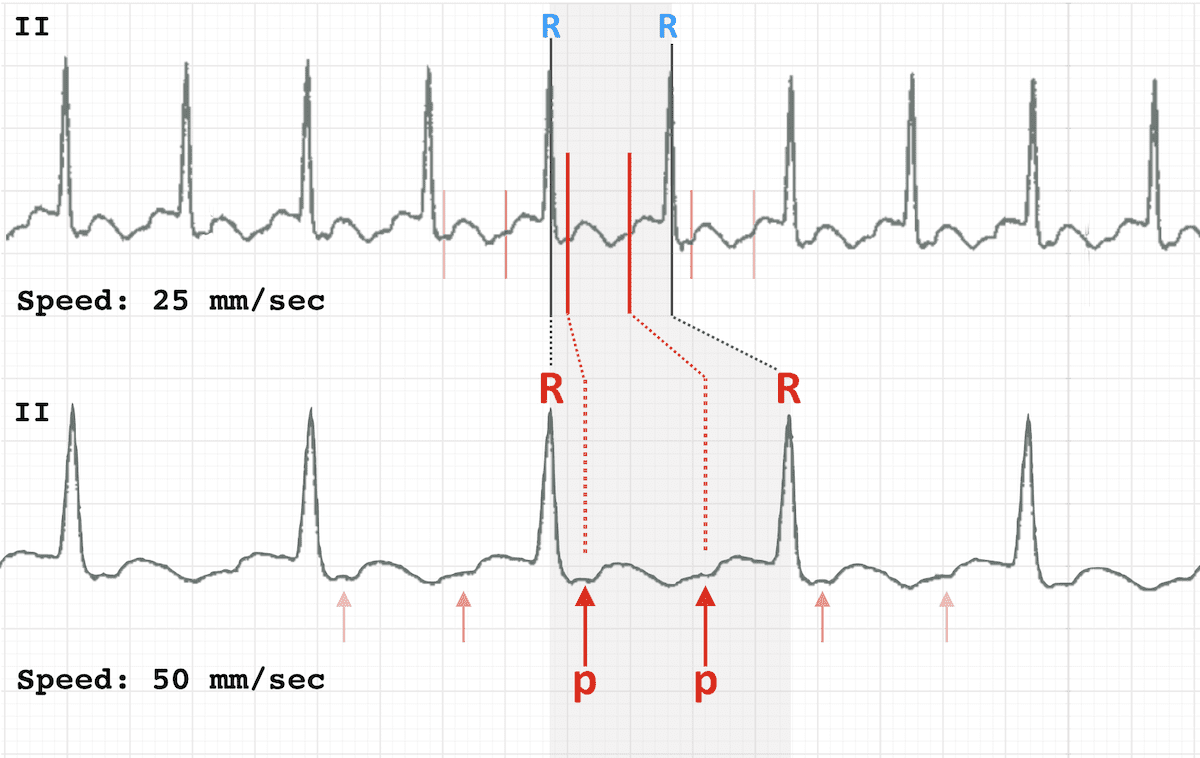
Having trouble seeing P waves in the midst of the flashing fluorescent lighting, loud beeping, and interruptions of ED?
There are a couple of other tricks still (5)
There are a couple of other tricks still (5)
Double the paper speed -- this is the rate at which the ECG machine produces a trace. Standard output is 25mm/sec.
Doubling the rate to 50mm/sec causes the ECG trace to appear "drawn out". Particularly useful for revealing flutter waves in 2:1 block (6)
Doubling the rate to 50mm/sec causes the ECG trace to appear "drawn out". Particularly useful for revealing flutter waves in 2:1 block (6)
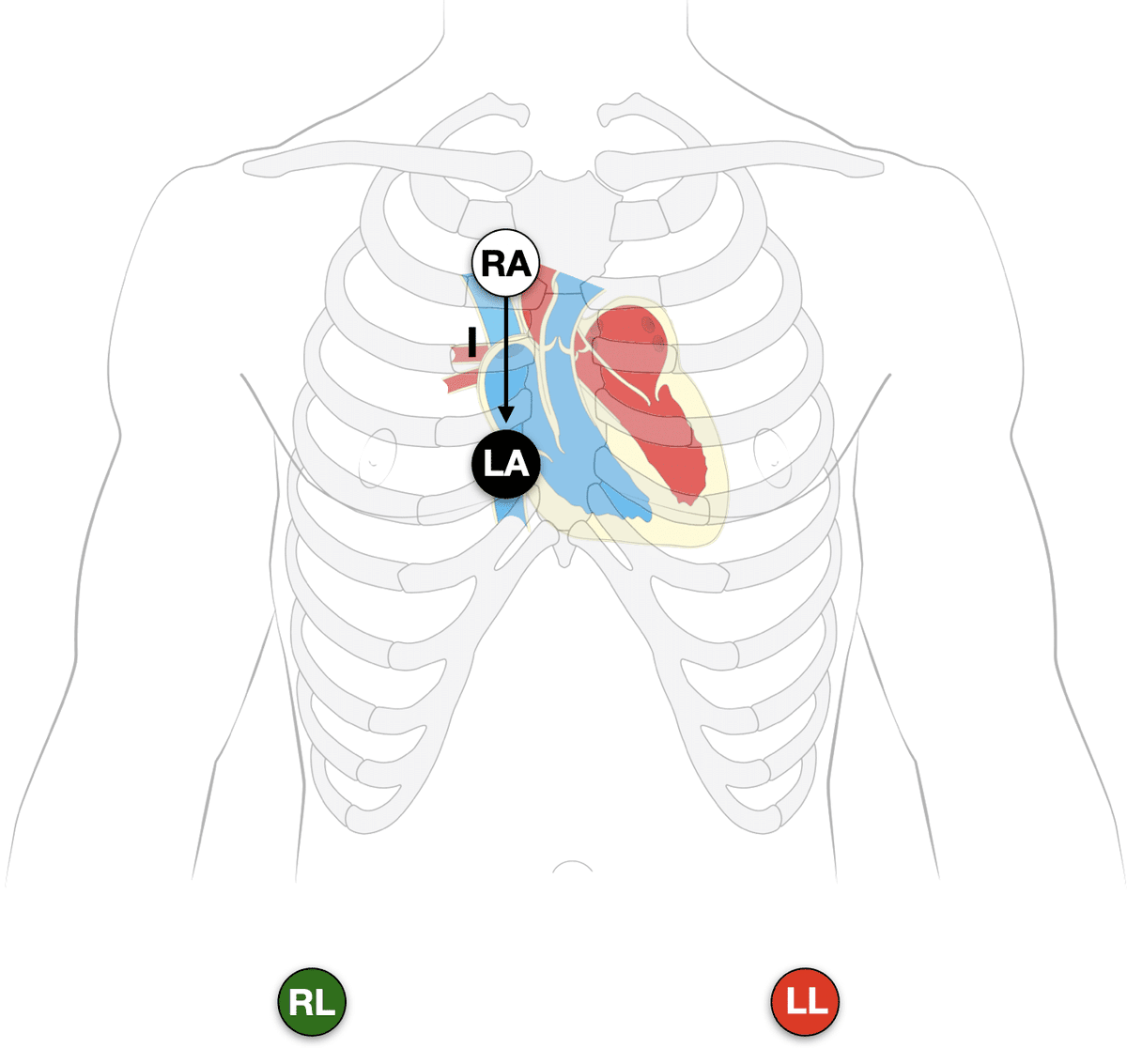
At the same time, try the Lewis Lead configuration, which better detects atrial activity in relation to ventricles.
Place the RA & LA electrodes just to the right of the sternum (2nd & 4th ICS respectively), and monitor lead I. Also useful for detecting AV dissoc. in WCT (7)
Place the RA & LA electrodes just to the right of the sternum (2nd & 4th ICS respectively), and monitor lead I. Also useful for detecting AV dissoc. in WCT (7)
Lastly, adenosine is useful as both a diagnostic and therapeutic tool in stable patients.
It will almost always work for AVNRT and orthodromic AVRT, and aborts some paroxysmal FATs.
Whilst it won't revert atrial flutter, it will often reveal flutter waves (8)
It will almost always work for AVNRT and orthodromic AVRT, and aborts some paroxysmal FATs.
Whilst it won't revert atrial flutter, it will often reveal flutter waves (8)
One more thing.
Try to avoid the term SVT when it comes to narrow complex tachycardias. The mere fact that they are narrow complex already tells us they are supraventricular in origin. I reserve this term for describing VT versus SVT with aberrancy. (9)
Try to avoid the term SVT when it comes to narrow complex tachycardias. The mere fact that they are narrow complex already tells us they are supraventricular in origin. I reserve this term for describing VT versus SVT with aberrancy. (9)
• • •
Missing some Tweet in this thread? You can try to
force a refresh