1/ "Do you have a second to chat?"
(i.e., The phrase that results in almost a reflex cringe 😳...)
We all want feedback,
but we dread it at the same time.
How can we deliver better feedback?
Check out this week's thread for some tips!
(i.e., The phrase that results in almost a reflex cringe 😳...)
We all want feedback,
but we dread it at the same time.
How can we deliver better feedback?
Check out this week's thread for some tips!

2/ This week we will discuss giving feedback in the inpatient setting with a focus on integrating it into daily clinical care.
For more detailed threads on feedback, check out our prior 11-week series on the topic:
twitter.com/i/events/13632…
For more detailed threads on feedback, check out our prior 11-week series on the topic:
twitter.com/i/events/13632…

3/ For feedback to be well-received, there needs to be a culture of trust and respect between you and your learner(s).
Seriously, this is THE most important part.
Check out @GStetsonMD's prior thread on the topic:
Seriously, this is THE most important part.
Check out @GStetsonMD's prior thread on the topic:
https://twitter.com/GStetsonMD/status/1361722281324642305
4/ This paper in @AcadMedJournal on the educational alliance describes the importance of the supervisor-trainee relationship in feedback. 

5/ So how can we create an effective educational alliance?
Well, I think it's helpful to use a coaching framework to rethink our feedback delivery.
See my schema below, which provides a more familiar example of how coaching is used in a sport, like tennis.
Well, I think it's helpful to use a coaching framework to rethink our feedback delivery.
See my schema below, which provides a more familiar example of how coaching is used in a sport, like tennis.

6/ But we should teach feedback in medicine in the same way.
Because our goal it to improve our learners' performance, no matter what level they are at when they join us.
So let's be a coach!
Right, @ETSshow? #MedLasso
Because our goal it to improve our learners' performance, no matter what level they are at when they join us.
So let's be a coach!
Right, @ETSshow? #MedLasso
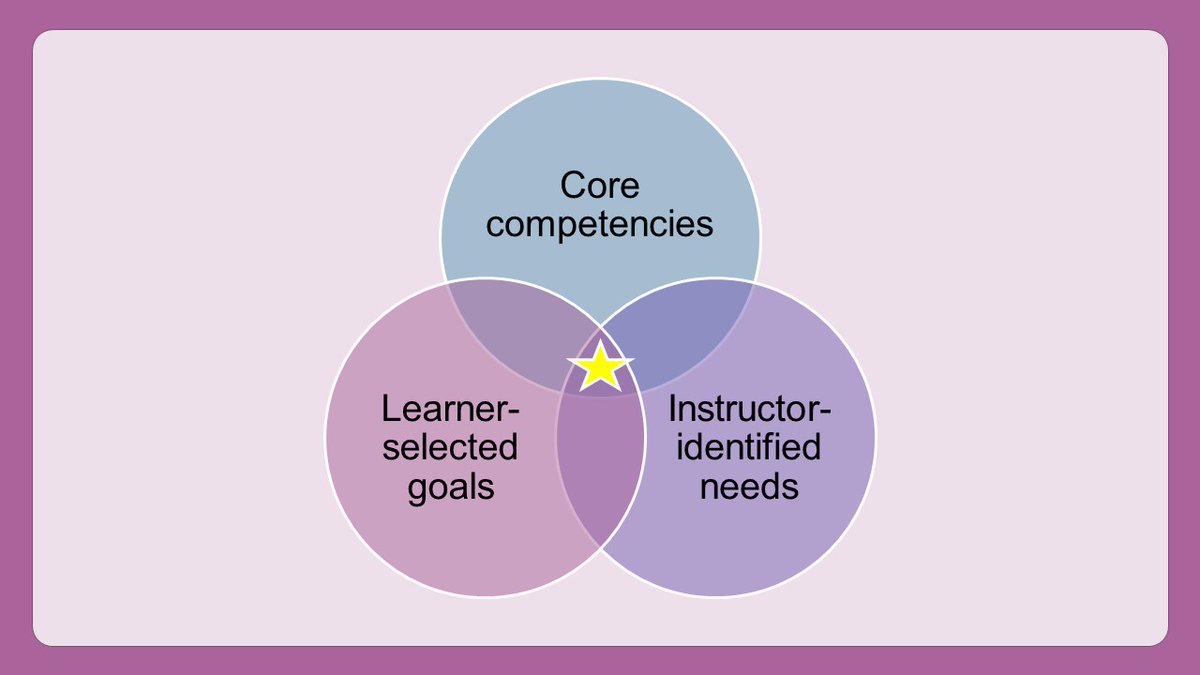
7/ Step 1: Goal Setting
To do this, I ask each learner to identify 2 things that they want to work on during their time with me.
I help them refine their goals to align with core competencies & include any areas that I have identified as an area of need.
To do this, I ask each learner to identify 2 things that they want to work on during their time with me.
I help them refine their goals to align with core competencies & include any areas that I have identified as an area of need.
8/ Here's an example of how I would negotiate goal-setting with a learner who wants to work on "efficiency" which is one of the most common goals that I hear from learners.
Notice that I still keep the goal related to their interest. I just help them refine it.
Notice that I still keep the goal related to their interest. I just help them refine it.

9/ Now, you may be wondering what to do if you have a learner who isn't meeting expectations and doesn't identify a goal that aligns with difficult feedback you need to give.
Thankfully @GStetsonMD has already written a thread specifically on that topic!
Thankfully @GStetsonMD has already written a thread specifically on that topic!
https://twitter.com/GStetsonMD/status/1376945713515528192
10/ Step 2: Observation
There are SO MANY opportunities for us to observe learners during the day (see below).
For the efficiency example that I've provided, it would be important to actually watch a learner work up a new patient. Use this time to staff a new patient early!
There are SO MANY opportunities for us to observe learners during the day (see below).
For the efficiency example that I've provided, it would be important to actually watch a learner work up a new patient. Use this time to staff a new patient early!

11/ Step 3: Evaluation
The term "evaluation" is loaded.
But the idea is that we are just communicating to the learner what we have observed.
We can give indirect or direct feedback. Both have their place. But most of our feedback should be on the right side of this spectrum.
The term "evaluation" is loaded.
But the idea is that we are just communicating to the learner what we have observed.
We can give indirect or direct feedback. Both have their place. But most of our feedback should be on the right side of this spectrum.

12/ And it's important that this feedback occurs FREQUENTLY, not JUST at the end of the rotation. Because the feedback is what helps them improve.
13/ Ex: If I'm giving feedback on efficiency of their notes, then I should give them daily tips on how to improve their efficiency - new SmartPhrases to add, options for making the notes more succinct, etc.
Then, at the end of the rotation, I can reinforce changes they've made.
Then, at the end of the rotation, I can reinforce changes they've made.
14/ Step 4: Action Plan
Then, at the end, it's important for us to co-formulate an action plan for continued growth with the learner.
Notice that this should be CO-CREATED. I often ask learners for their ideas first. Then I build on them with my own ideas.
Then, at the end, it's important for us to co-formulate an action plan for continued growth with the learner.
Notice that this should be CO-CREATED. I often ask learners for their ideas first. Then I build on them with my own ideas.
15/ You'll notice that we've already started creating an action plan in our example since we've provided some efficiency tips. So the action plan is being enacted during the rotation.
But at the end, I try to create an action plan for continued improvement (or something new!).
But at the end, I try to create an action plan for continued improvement (or something new!).
16/ So, in summary, use coaching to help you deliver better feedback.
It allows you to engage in continual feedback throughout the rotation. And, because it's feedback on a learner-selected goal, they will be excited to have those feedback conversations!
It allows you to engage in continual feedback throughout the rotation. And, because it's feedback on a learner-selected goal, they will be excited to have those feedback conversations!

17/ Join us next Tuesday when @YihanYangMD discusses how to teach with family meetings.
In the meantime, follow @MedEdTwagTeam, @GStetsonMD, & @ChrisDJacksonMD so that you don't miss any content!
In the meantime, follow @MedEdTwagTeam, @GStetsonMD, & @ChrisDJacksonMD so that you don't miss any content!

• • •
Missing some Tweet in this thread? You can try to
force a refresh