1/
I posted this case last week as a mystery case.
Lots of votes for dissection, which I agree would seem totally plausible. But...
This was not a dissection!
I left out some key details to make it more interesting
So... what *was* going on here?
#EmoryNCCTweetorials
I posted this case last week as a mystery case.
Lots of votes for dissection, which I agree would seem totally plausible. But...
This was not a dissection!
I left out some key details to make it more interesting
So... what *was* going on here?
#EmoryNCCTweetorials
https://twitter.com/caseyalbin/status/1529976886369165312
2/
Before diving in, major shout outs to fellows @maness_caroline & @stevefylypiw & @b3ta_lacTAM for their help investigating!!🤩
So... best guess, where is the stroke?
Reminder, the symptoms:
👁️ Unilateral (Left) Miosis
😵💫Vertigo
😴 Altered consciousness
Before diving in, major shout outs to fellows @maness_caroline & @stevefylypiw & @b3ta_lacTAM for their help investigating!!🤩
So... best guess, where is the stroke?
Reminder, the symptoms:
👁️ Unilateral (Left) Miosis
😵💫Vertigo
😴 Altered consciousness
3/
Of these, the best guess is the lateral medulla.
✨Descending sympathetic fibers = Horner’s syndrome (miosis. Hard to eval ptosis, anhidrosis in this acute situation)
✨Vestibular nuclei = vertigo
(Lateral pons can cause these as well, but that wasn’t an option)
Of these, the best guess is the lateral medulla.
✨Descending sympathetic fibers = Horner’s syndrome (miosis. Hard to eval ptosis, anhidrosis in this acute situation)
✨Vestibular nuclei = vertigo
(Lateral pons can cause these as well, but that wasn’t an option)
4/
But -- What about the altered consciousness??
The altered mental status was due to acute hypercarbic respiratory failure resulting from Ondine’s curse.
....What's this Ondine’s curse, you say...?
I have a whole #Tweetorial for you!
But -- What about the altered consciousness??
The altered mental status was due to acute hypercarbic respiratory failure resulting from Ondine’s curse.
....What's this Ondine’s curse, you say...?
I have a whole #Tweetorial for you!
https://twitter.com/caseyalbin/status/1387781213306376195
5/
The patient was significantly hypercarbic on the first ABG after intubation & continued to become apneic on SBT any time they slept.
This is due to the loss of respiration pattern generators in the lateral medulla (explained in more detail in the linked #tweetorial ⬆️)
The patient was significantly hypercarbic on the first ABG after intubation & continued to become apneic on SBT any time they slept.
This is due to the loss of respiration pattern generators in the lateral medulla (explained in more detail in the linked #tweetorial ⬆️)
6/
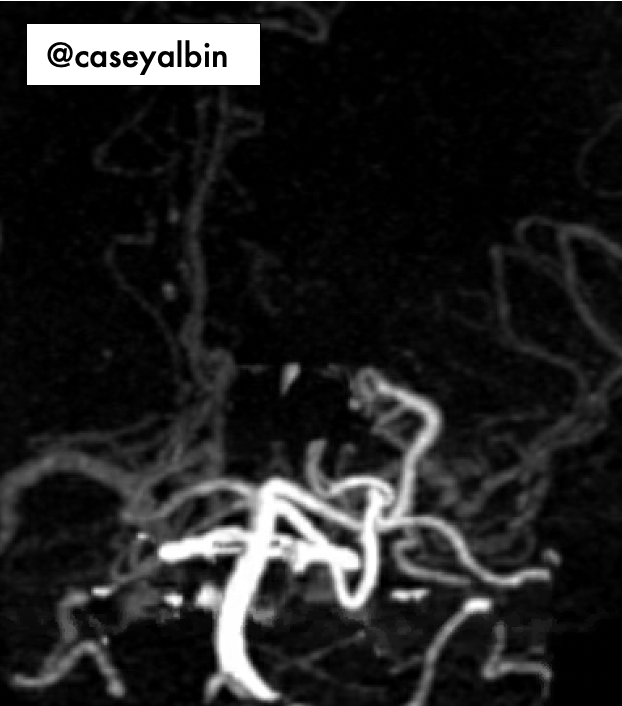
So, we have a suspected left lateral medullary stroke. The arterial supply is either the
🩸L vertebral artery or
🩸L PICA (usually a branch of the left vert)…
Back to the imaging:
The whole left side of the vertebral-basilar system is brighter than the right side. 🤔
So, we have a suspected left lateral medullary stroke. The arterial supply is either the
🩸L vertebral artery or
🩸L PICA (usually a branch of the left vert)…
Back to the imaging:
The whole left side of the vertebral-basilar system is brighter than the right side. 🤔
7/
Here’s a source image.
You can see highlighted that left vert opacifies and the right doesn’t.
In a dissection, the side that is dissected loses/has diminished opacification due to tear/associated thrombus.
*Vert distribution* pathology is often ipsilateral to the tear.
Here’s a source image.
You can see highlighted that left vert opacifies and the right doesn’t.
In a dissection, the side that is dissected loses/has diminished opacification due to tear/associated thrombus.
*Vert distribution* pathology is often ipsilateral to the tear.

8/
Said differently, in this case, the stroke localizes ipsilateral to the side that opacifies with contrast.
Another fun recon to emphasis this.
Left = opacified, right = not so much.
⬇️⬇️⬇️
Said differently, in this case, the stroke localizes ipsilateral to the side that opacifies with contrast.
Another fun recon to emphasis this.
Left = opacified, right = not so much.
⬇️⬇️⬇️

9/
What is going on!?
Well, the big fact I left out in this case: the patient is in the CV-ICU on ECMO.
I know, I know. That’s really an important nugget of context! 😉 But for the fun of guessing...
What is going on!?
Well, the big fact I left out in this case: the patient is in the CV-ICU on ECMO.
I know, I know. That’s really an important nugget of context! 😉 But for the fun of guessing...
10/
Next question: is why is the patient on ECMO?
Answer:
💔 Very advanced heart failure awaiting transplant
Which means the patient was on *VA-ECMO*
Next question: is why is the patient on ECMO?
Answer:
💔 Very advanced heart failure awaiting transplant
Which means the patient was on *VA-ECMO*
11/
In VA-ECMO the blood is removed from a venous cannula -> oxygenated -> returned to the arterial side to perfuse the rest of the body.
The ECMO circuit does the work of the 🫁 AND ♥️!
Image:link.springer.com/article/10.100…
In VA-ECMO the blood is removed from a venous cannula -> oxygenated -> returned to the arterial side to perfuse the rest of the body.
The ECMO circuit does the work of the 🫁 AND ♥️!
Image:link.springer.com/article/10.100…

12/
There are a lot of models and configurations of ECMO. We do a fair number of consults with the CV-team, and I still find the different set-ups confusing.
BUT, if you take away nothing else, remember that it is so helpful to understand the setup when doing a stroke eval!
There are a lot of models and configurations of ECMO. We do a fair number of consults with the CV-team, and I still find the different set-ups confusing.
BUT, if you take away nothing else, remember that it is so helpful to understand the setup when doing a stroke eval!
13/
In this case the patient had a sport configuration:
a left subclavian venous cannula sent blood to the ECMO and a left axillary arterial cannula returned the blood
Similar to this but on the left.
ahajournals.org/doi/10.1161/CI…
In this case the patient had a sport configuration:
a left subclavian venous cannula sent blood to the ECMO and a left axillary arterial cannula returned the blood
Similar to this but on the left.
ahajournals.org/doi/10.1161/CI…

14/
The reason this matters?
ECMO set-up and native heart function affect where the mixing cloud is!
🔁Mixing cloud = where does the blood returning from the circuit meets the blood that has been pumped from the patient’s native heart.
The reason this matters?
ECMO set-up and native heart function affect where the mixing cloud is!
🔁Mixing cloud = where does the blood returning from the circuit meets the blood that has been pumped from the patient’s native heart.
15/
Can we see this with contrast?
1⃣st, how does contrast circulate if the patient is on ECMO?
Most contrast is removed via the venous cannula ➡️ circulates through ECMO ➡️flows to the arterial side ➡️ travels to the rest of the body. Review: tinyurl.com/2p92h29a
Can we see this with contrast?
1⃣st, how does contrast circulate if the patient is on ECMO?
Most contrast is removed via the venous cannula ➡️ circulates through ECMO ➡️flows to the arterial side ➡️ travels to the rest of the body. Review: tinyurl.com/2p92h29a
16/
So most contrast re-enters the circulation from the ECMO device!
A quick scroll down the CTA demonstrates the contrast-rich blood (from ECMO) mixes with the contrast-poor blood (from native heart) in the aortic arch between the left common carotid and the left subclavian.
So most contrast re-enters the circulation from the ECMO device!
A quick scroll down the CTA demonstrates the contrast-rich blood (from ECMO) mixes with the contrast-poor blood (from native heart) in the aortic arch between the left common carotid and the left subclavian.

17/
This is tricky to visualize, right?
Fortunately, Tammy Lin (@b3ta_lacTAM), CV-ICU fellow and illustrator extraordinary made a beautiful figure to illustrate this!!
Dark red = pumped from heart (*note* this blood is not hypoxic! Lungs were fine)
Light red = pumped from ECMO
This is tricky to visualize, right?
Fortunately, Tammy Lin (@b3ta_lacTAM), CV-ICU fellow and illustrator extraordinary made a beautiful figure to illustrate this!!
Dark red = pumped from heart (*note* this blood is not hypoxic! Lungs were fine)
Light red = pumped from ECMO

18/
So! The difference in opacification reflects the difference in the source of perfusion: contrast-rich from ECMO versus contrast-poor from native heart.
So! The difference in opacification reflects the difference in the source of perfusion: contrast-rich from ECMO versus contrast-poor from native heart.

19/
In this case the brachiocephalic & left common carotid got perfusion directly from the heart.
The left subclavian (and vert) received perfusion from the ECMO circuit.
Meaning that of the 4 vessels perfusing the brain, only the left vert received direct-from-ECMO blood!
In this case the brachiocephalic & left common carotid got perfusion directly from the heart.
The left subclavian (and vert) received perfusion from the ECMO circuit.
Meaning that of the 4 vessels perfusing the brain, only the left vert received direct-from-ECMO blood!
20/
So... where did the lateral medullary stroke come from??
The ECMO circuit.
Here, a few days later, you can see that something seems off at the base of the brainstem on the left. MRI would be better.. but #ECMO.
So... where did the lateral medullary stroke come from??
The ECMO circuit.
Here, a few days later, you can see that something seems off at the base of the brainstem on the left. MRI would be better.. but #ECMO.
21/
Finally, it’s hard to time a perfusion study for a patient on ECMO, so it may also be the perfusion is attenuated because of poor timing… but here is the CTP.
Finally, it’s hard to time a perfusion study for a patient on ECMO, so it may also be the perfusion is attenuated because of poor timing… but here is the CTP.

22/
So perfectly watershed-y, which fits with how the blood is traveling to the anterior circulation & right posterior circulation from a failing heart (seems plausible it would have delayed transit times). Notably, there is no green in the the L cerebellum.
Rads-- thoughts?
So perfectly watershed-y, which fits with how the blood is traveling to the anterior circulation & right posterior circulation from a failing heart (seems plausible it would have delayed transit times). Notably, there is no green in the the L cerebellum.
Rads-- thoughts?
23/
Ultimately, this was a challenging case for many reasons.
But some takeaways are:
1⃣ Always look for pupil asymmetry in a pt with AMS
2⃣ Stroke consult? Ask the CV people to review the ECMO circuitry with you
3⃣ When possible find the contrast-mixing cloud
Ultimately, this was a challenging case for many reasons.
But some takeaways are:
1⃣ Always look for pupil asymmetry in a pt with AMS
2⃣ Stroke consult? Ask the CV people to review the ECMO circuitry with you
3⃣ When possible find the contrast-mixing cloud
24/
Thanks again to @maness_caroline, @stevefylypiw, @b3ta_lacTAM!! And @CajalButterfly for marveling at the images with me in real time.
Thoughts from ECMO and vascular gurus, did we miss anything?? @emcrit @rkchoi @ShadiYaghi2 @SVINJournal @drdangayach @ThinkingCC
Thanks again to @maness_caroline, @stevefylypiw, @b3ta_lacTAM!! And @CajalButterfly for marveling at the images with me in real time.
Thoughts from ECMO and vascular gurus, did we miss anything?? @emcrit @rkchoi @ShadiYaghi2 @SVINJournal @drdangayach @ThinkingCC
@PulmCrit @a_charidimou @MicieliA_MD @EmoryNeuroCrit @EM_RESUS @MelHerbert @TrinaAugustinMD @Capt_Ammonia @EricLawson90 @sigman_md @namorrismd @pouyeah @SubinMatthews @theABofPharmaC @CaseyMayPharmD @KeatonSmetana @aartisarwal @neurologyrules
@threadreaderapp unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh











