THREAD on LONG COVID for non-specialists (GPs, patients). Covers what it is, who gets it, what causes it, what to do, what the outlook is. Drawing on in-preparation paper with @bcdelaney @ruairidhm @REvans_Breathe @sivanmanoj @LOCOMOTIONstudy
1/
[mute thread if not interested]
1/
[mute thread if not interested]
DEFINITION
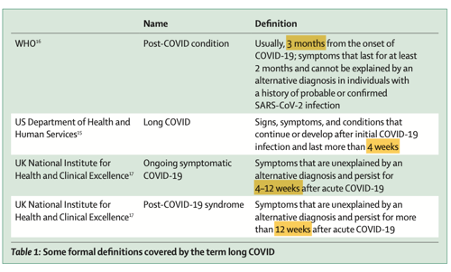
A ‘patient-made’ term referring to symptoms persisting > 4 weeks after an acute covid-19 illness, and not explained by any other diagnosis. Includes ‘ongoing symptomatic covid-19’ (4-12w) and ‘post covid-19 syndrome’ (beyond 12w) [NICE].
nice.org.uk/guidance/ng188…
2/
A ‘patient-made’ term referring to symptoms persisting > 4 weeks after an acute covid-19 illness, and not explained by any other diagnosis. Includes ‘ongoing symptomatic covid-19’ (4-12w) and ‘post covid-19 syndrome’ (beyond 12w) [NICE].
nice.org.uk/guidance/ng188…
2/
The term ‘long covid’ also aligns with the World Health Organisation’s clinical case definition of ‘post-covid-19 condition’
who.int/publications/i…
3/
who.int/publications/i…
3/
HOW COMMON?
Whilst most people who get acute covid-19 get better quickly, some don’t. In UK, 2 million people report symptoms for >4 weeks, 826,000 (42% of all long covid patients) in more than 1 year and 376,000 (19%) in more than 2 years.
ons.gov.uk/peoplepopulati…
4/
Whilst most people who get acute covid-19 get better quickly, some don’t. In UK, 2 million people report symptoms for >4 weeks, 826,000 (42% of all long covid patients) in more than 1 year and 376,000 (19%) in more than 2 years.
ons.gov.uk/peoplepopulati…
4/
SYMPTOMS
Long covid is a constellation of symptoms across many organ systems. Fatigue is the commonest. Symptoms may fluctuate and flare up in response to triggers (physical or emotional). Great diagram here from David Jiang et al’s paper.
jacc.org/doi/abs/10.101…
5/
Long covid is a constellation of symptoms across many organ systems. Fatigue is the commonest. Symptoms may fluctuate and flare up in response to triggers (physical or emotional). Great diagram here from David Jiang et al’s paper.
jacc.org/doi/abs/10.101…
5/

Whilst the symptom list for long covid (previous tweet) is long and ‘non-specific’, they tend to occur in recognisable patterns (‘phenotypes’), as this paper from the @Join_ZOE study showed.
nature.com/articles/s4159…
6/
nature.com/articles/s4159…
6/
WHO GETS LONG VOCID?
Anyone can. It’s more likely after more severe acute illness and if
- female
- aged 35-69
- poor
- overweight
- other activity-limiting long-term conditions e.g. diabetes, heart disease
Systematic review:
ncbi.nlm.nih.gov/pmc/articles/P…
7/
Anyone can. It’s more likely after more severe acute illness and if
- female
- aged 35-69
- poor
- overweight
- other activity-limiting long-term conditions e.g. diabetes, heart disease
Systematic review:
ncbi.nlm.nih.gov/pmc/articles/P…
7/
WHAT CAUSES LONG COVID?
Many viral illnesses (including other coronaviruses SARS and MERS) produce prolonged illness (with fatigue a dominant symptom). But we don’t know why this happens in some people while others recover quickly.
tandfonline.com/doi/full/10.10…
8/
Many viral illnesses (including other coronaviruses SARS and MERS) produce prolonged illness (with fatigue a dominant symptom). But we don’t know why this happens in some people while others recover quickly.
tandfonline.com/doi/full/10.10…
8/
In long covid, the body reacts in a counterproductive way to the virus. Mechanisms include chronic inflammation, thrombosis (‘micro clots’) and endothelial damage. This impacts various organs—e.g. autonomic nervous system.
ncbi.nlm.nih.gov/pmc/articles/P…
9/
ncbi.nlm.nih.gov/pmc/articles/P…
9/
In some people, there is an auto-immune type reaction where the body starts to recognise its own tissues as foreign.
science.org/doi/10.1126/sc…
(But claims of ‘lupus-like’ syndrome and a major role for anti phosophilipid antibody are speculative)
10/
science.org/doi/10.1126/sc…
(But claims of ‘lupus-like’ syndrome and a major role for anti phosophilipid antibody are speculative)
10/
MENTAL AND SOCIAL EFFECTS
Being chronically ill and with unpredictable relapses may lead to loss of work, income and social interaction, leading to poor mental health. (But just because someone with LC has anxiety/depression doesn’t mean that’s what *caused* the LC).
11/
Being chronically ill and with unpredictable relapses may lead to loss of work, income and social interaction, leading to poor mental health. (But just because someone with LC has anxiety/depression doesn’t mean that’s what *caused* the LC).
11/
Paper here on the illness narratives of people with long covid. When this condition was first described, nobody believed in it and symptoms were dismissed by family, friends and health professionals. We know more now; this disease is real!
sciencedirect.com/science/articl…
12/
sciencedirect.com/science/articl…
12/
WHAT CAN GPs DO?
Patients with long covid greatly value input from their primary care clinician. Notwithstanding uncertainties and lack of definitive curative therapies, generalist clinicians can help patients a lot: see next tweet. Several appointments may be needed.
13/
Patients with long covid greatly value input from their primary care clinician. Notwithstanding uncertainties and lack of definitive curative therapies, generalist clinicians can help patients a lot: see next tweet. Several appointments may be needed.
13/
GPs can help by hearing the patient’s story and validating their experience; providing holistic, relationship-based care; examining the patient in a face-to-face appointment; excluding alternative diagnoses; and directing to resources (links below).
14/
14/
GPs can also manage specific symptoms & comorbidities (esp diabetes /CVS); monitor progress (physical and mental) and share the uncertainties of prognosis; helping set realistic goals for recovery; provide sick notes and support self-advocacy (e.g. with employer)
15/
15/
WHAT TESTS ARE NEEDED?
There is no ‘standard panel’ of blood tests, images or other investigations for a person with long covid. This is because management is currently geared to identifying and managing risk factors and comorbidities, and treating specific symptoms.
16/
There is no ‘standard panel’ of blood tests, images or other investigations for a person with long covid. This is because management is currently geared to identifying and managing risk factors and comorbidities, and treating specific symptoms.
16/
Unexplained fatigue needs basic tests to exclude anaemia, low vit D levels, heart failure etc. Breathlessness needs basic tests of lung function including oximetry and (if indicated) a chest x-ray. If pulmonary embolus suspected, patient probably needs specialist referral.
17/
17/
Cardiac-sounding chest pain requires ECG and rapid-access clinic referral. Symptoms of autonomic dysfunction (rapid rise in pulse rate on standing) may indicate POTS (postural orthostatic tachycardia syndrome). (Often misdiagnosed as anxiety, sadly.)
ncbi.nlm.nih.gov/pmc/articles/P…
18/
ncbi.nlm.nih.gov/pmc/articles/P…
18/
‘Brain fog’ (poor cognitive function, memory probs) often accompanies (+ fluctuates with) fatigue. Use brief cognitive screening test (e.g. Mini Mental State). If unable to work or safety-critical occupation, refer for formal neuropsychological tests.
pubmed.ncbi.nlm.nih.gov/35136912/
19/
pubmed.ncbi.nlm.nih.gov/35136912/
19/
Allergic-type symptoms (urticarial rash, conjunctivitis, abdominal bloating, regurgitation) may respond to over the counter antihistamines. There are ongoing RCTs of specific antihistamines e.g. in the STIMULATE-ICP study.
stimulate-icp.org/about
20/
stimulate-icp.org/about
20/
Sleep disturbance may respond to sleep hygiene measures, and possibly to melatonin if circadian rhythm is disrupted.
21/
ncbi.nlm.nih.gov/pmc/articles/P…
21/
ncbi.nlm.nih.gov/pmc/articles/P…
Patients may have heard about tests of clotting and inflammatory function. These are the subject of much research but are not routinely used in clinical practice (yet).
22/
22/
ONLINE LONG COVID RESOURCES FOR PATIENTS
Nice one here from NHS Hertfordshire aimed at UK patients
Downloadable from hct.nhs.uk/media/4529/lon….
23/
Nice one here from NHS Hertfordshire aimed at UK patients
Downloadable from hct.nhs.uk/media/4529/lon….
23/
Support for rehabilitation: self-management after COVID-19 related illness—a World Health Organisation guide for patients.
apps.who.int/iris/handle/10…
24/
apps.who.int/iris/handle/10…
24/
For those who prefer a website, try Long Covid Recovery run by physiotherapists
yourcovidrecovery.nhs.uk
26/
yourcovidrecovery.nhs.uk
26/
If the patient’s main symptom is problems with breathing, there’s a specialist physio website on ‘Breathing Pattern Disorders’
physiotherapyforbpd.org.uk
27/
physiotherapyforbpd.org.uk
27/
SUPPORT GROUPS FOR LONG COVID
There are many. These are good:
Long Covid SOS longcovidsos.org
Long Covid Support longcovid.org
Long Covid Kids longcovidkids.org
29/
There are many. These are good:
Long Covid SOS longcovidsos.org
Long Covid Support longcovid.org
Long Covid Kids longcovidkids.org
29/
e-learning resource from the UK Royal College of General Practitioners:
‘Long term effects of COVID-19 and Post-COVID-19 syndrome’ elearning.rcgp.org.uk/course/view.ph…
31/
‘Long term effects of COVID-19 and Post-COVID-19 syndrome’ elearning.rcgp.org.uk/course/view.ph…
31/
e-learning modules for health professionals from Health Education England on long covid
e-lfh.org.uk/programmes/lon…
32/
e-lfh.org.uk/programmes/lon…
32/
VACCINATION
Vaccination against covid-19 helps prevent long covid by reducing the chance of symptomatic infection, but it doesn’t fully protect. Some people will develop long covid after acute infection even if vaccinated.
ons.gov.uk/peoplepopulati…
33/
Vaccination against covid-19 helps prevent long covid by reducing the chance of symptomatic infection, but it doesn’t fully protect. Some people will develop long covid after acute infection even if vaccinated.
ons.gov.uk/peoplepopulati…
33/
If you weren’t fully vaccinated when you developed long covid, a vaccination might help improve your symptoms but the improvement may be modest and isn’t guaranteed.
bmj.com/content/377/bm…
34/
bmj.com/content/377/bm…
34/
MONITORING SYMPTOMS AND FUNCTIONAL STATUS
The best current guide to whether a patient is getting better from long covid is whether they feel better. The C19-YRS is a validated patient-reported outcome measure for use in clinic and research.
ncbi.nlm.nih.gov/pmc/articles/P…
35/
The best current guide to whether a patient is getting better from long covid is whether they feel better. The C19-YRS is a validated patient-reported outcome measure for use in clinic and research.
ncbi.nlm.nih.gov/pmc/articles/P…
35/
DISCLAIMER: I have not checked every word of every resource. Please don't send me abuse if you find a sentence that you don't agree with! (sorry but this happens a LOT).
Will add to this thread as new research findings emerge or review articles appear.
36/ end (for now)
Will add to this thread as new research findings emerge or review articles appear.
36/ end (for now)
• • •
Missing some Tweet in this thread? You can try to
force a refresh