1/
#NeuroPostItPearls #8 (early!): Practice thinking like a Neurologist.
To help you, a #Tweetorial Case adapted from my colleague and dear friend @emeltzermd's new book
“How to Think like a Neurologist.” amazon.com/How-Think-Like…
✨The Case✨
The Man Who Began To Drool.
#NeuroPostItPearls #8 (early!): Practice thinking like a Neurologist.
To help you, a #Tweetorial Case adapted from my colleague and dear friend @emeltzermd's new book
“How to Think like a Neurologist.” amazon.com/How-Think-Like…
✨The Case✨
The Man Who Began To Drool.
2/
A 41 yo M w/ history of testicular cancer presents with a vague headache & several days of fatigue. A few days after these vague symptoms began, he developed burning over with left abdomen and right retroauricular pain. A day later his wife points out that he’s drooling.
🤤
A 41 yo M w/ history of testicular cancer presents with a vague headache & several days of fatigue. A few days after these vague symptoms began, he developed burning over with left abdomen and right retroauricular pain. A day later his wife points out that he’s drooling.
🤤
3/
🛑Pause Here! (the book instructs you to do so!) 🛑
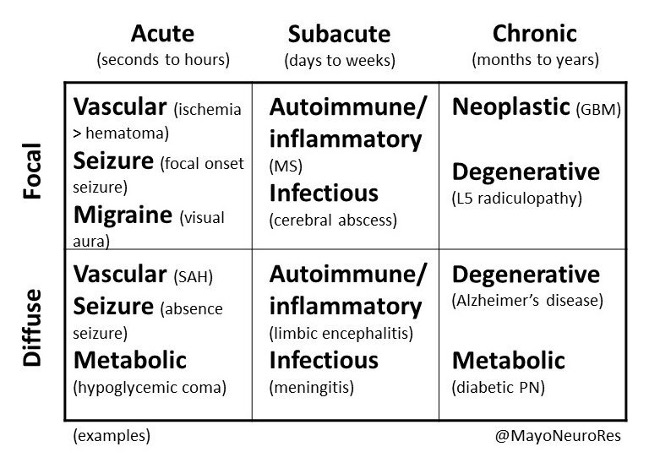
Just as suggested by this awesome chart shared by @LyellJ & @mayoneurores, all neurologic diagnosis starts with determining the tempo and focal/diffuse
🛑Pause Here! (the book instructs you to do so!) 🛑
Just as suggested by this awesome chart shared by @LyellJ & @mayoneurores, all neurologic diagnosis starts with determining the tempo and focal/diffuse

So what do you think
4/
This sounds diffuse and subacute to me!
Now to localization📍:
You suspect he has facial weakness.
But how will you localize it?
[Admit it, you (like me) all just thought, “upper face involvement means LMN facial weakness.” Done.]
From: emdocs.net/wp-content/upl…
This sounds diffuse and subacute to me!
Now to localization📍:
You suspect he has facial weakness.
But how will you localize it?
[Admit it, you (like me) all just thought, “upper face involvement means LMN facial weakness.” Done.]
From: emdocs.net/wp-content/upl…

5/
Fair.
But there is so much more you can OBJECTIVELY test!
🛎️Bell’s phenomenon
👁️Corneal reflex
🦻Hearing acuity
👅Taste on the anterior 2/3s of the tongue
Fair.
But there is so much more you can OBJECTIVELY test!
🛎️Bell’s phenomenon
👁️Corneal reflex
🦻Hearing acuity
👅Taste on the anterior 2/3s of the tongue
6/
Bell’s phenomenon (the palpebral oculogyric reflex) – omg don’t you love neurology speak?!
I have almost certainly never said oculogyric reflex, def not since critical care training… but 100% am going now.
What *is* the Bell’s phenomenon?
⏱️here: tinyurl.com/yc7jw5wu
Bell’s phenomenon (the palpebral oculogyric reflex) – omg don’t you love neurology speak?!
I have almost certainly never said oculogyric reflex, def not since critical care training… but 100% am going now.
What *is* the Bell’s phenomenon?
⏱️here: tinyurl.com/yc7jw5wu
7/
Understanding the other exam findings relies on understanding the anatomy of the facial nerve.
Ethan has you covered with a nice diagram of it in the book:
Understanding the other exam findings relies on understanding the anatomy of the facial nerve.
Ethan has you covered with a nice diagram of it in the book:

8/
👁️The corneal reflex is mediated by V (sens) & VII (motor). CN VII injury = no corneal reflex.
🦻Paralysis of the stapedius, innervated by VII results in the inability to appropriately dampen sound = hyperacusis
👅Taste to the anterior 2/3 of the tongue is also VII mediated!
👁️The corneal reflex is mediated by V (sens) & VII (motor). CN VII injury = no corneal reflex.
🦻Paralysis of the stapedius, innervated by VII results in the inability to appropriately dampen sound = hyperacusis
👅Taste to the anterior 2/3 of the tongue is also VII mediated!
9/
The point here is that by understanding the neuroanatomy, you can confirm a bedside diagnosis with greater accuracy by picking the right exam maneuvers.
With the cost of a Q-tip and some sugar we’ve confirmed a LMN pattern of CN VII injury!
The point here is that by understanding the neuroanatomy, you can confirm a bedside diagnosis with greater accuracy by picking the right exam maneuvers.
With the cost of a Q-tip and some sugar we’ve confirmed a LMN pattern of CN VII injury!
10/
But what about this pain over the thorax?
On exam there were sensory changes in the T10 and T11 dermatome distribution.
📍Localization here is either a radiculopathy or neuropathy of the thoracic roots/intercostal nerves.
But what about this pain over the thorax?
On exam there were sensory changes in the T10 and T11 dermatome distribution.
📍Localization here is either a radiculopathy or neuropathy of the thoracic roots/intercostal nerves.
11/
So, our patient has an acute onset VII-nerve palsy and a thoracic neuropathy or possible radiculopathy.
Ok, great! MRI Brain + C + T spine!?!
So, our patient has an acute onset VII-nerve palsy and a thoracic neuropathy or possible radiculopathy.
Ok, great! MRI Brain + C + T spine!?!
13/
So the “Syndromic Diagnosis” (provided for every case!):
✨“acute onset VII-nerve palsy and thoracic radiculopathy or neuropathy due to a leptomeningeal process"✨
But what’s the etiologic diagnosis?
Back to @LyellJ chart. Looking for something inflammatory, but...
So the “Syndromic Diagnosis” (provided for every case!):
✨“acute onset VII-nerve palsy and thoracic radiculopathy or neuropathy due to a leptomeningeal process"✨
But what’s the etiologic diagnosis?
Back to @LyellJ chart. Looking for something inflammatory, but...
14/
We'll need to confirm that the patient does in fact have an "-itis." One of the best ways to do this?
C🧪S🧪F (hopefully not green tho!)
Lumbar puncture reveals:
➡️WBC 21 (high!!!)
➡️Protein 41 (nl)
➡️Glucose 57 (nl)
We'll need to confirm that the patient does in fact have an "-itis." One of the best ways to do this?
C🧪S🧪F (hopefully not green tho!)
Lumbar puncture reveals:
➡️WBC 21 (high!!!)
➡️Protein 41 (nl)
➡️Glucose 57 (nl)
16/
This confirms that we have an “-itis”!!
You could now google “meningitis, facial palsy, and radiculopathy”:
This confirms that we have an “-itis”!!
You could now google “meningitis, facial palsy, and radiculopathy”:

18/
“So, patient... by the way, did you go camping in New England anytime recently?”
“Why, yes, actually! How did you know!? We went to Vermont a few weeks ago! Check out this rash I came back with!”
(multifocal erythema migrans)
“So, patient... by the way, did you go camping in New England anytime recently?”
“Why, yes, actually! How did you know!? We went to Vermont a few weeks ago! Check out this rash I came back with!”
(multifocal erythema migrans)

19/
And there you have It, folks, neuroborreliosis!
Treated and fully recovered. No wasteful tests, no unnecessary imaging. An elegant syndromic and etiologic diagnosis just by Thinking Like a Neurologist! 🕵️🧠
amazon.com/How-Think-Like…
And there you have It, folks, neuroborreliosis!
Treated and fully recovered. No wasteful tests, no unnecessary imaging. An elegant syndromic and etiologic diagnosis just by Thinking Like a Neurologist! 🕵️🧠
amazon.com/How-Think-Like…
20/
Best part! Ethan has agreed to give away two copies of the book!
Retweet the thread and of those people I'll select two people at random to get a copy.
Look at this awesome artwork on the cover. I'm obsessed!
Best part! Ethan has agreed to give away two copies of the book!
Retweet the thread and of those people I'll select two people at random to get a copy.
Look at this awesome artwork on the cover. I'm obsessed!

21/
@zach_london @harvardneuromds @NMatch2023 @gabifpucci @FTeixeiraMD @EmoryNeurology @EricLawson90 @sigman_md @AANmember @ContinuumAAN @syaddana_neuro @WNGtweets @ShadiYaghi2 @PulmCrit @drdangayach @MoiseyWoisey @JimSiegler @JimmySuhMD @AvrahamCooperMD @RebeccaFasanoMD @DxRxEdu
@zach_london @harvardneuromds @NMatch2023 @gabifpucci @FTeixeiraMD @EmoryNeurology @EricLawson90 @sigman_md @AANmember @ContinuumAAN @syaddana_neuro @WNGtweets @ShadiYaghi2 @PulmCrit @drdangayach @MoiseyWoisey @JimSiegler @JimmySuhMD @AvrahamCooperMD @RebeccaFasanoMD @DxRxEdu
@threadreaderapp unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh













