I'm putting together a lecture on AKI for emergency medicine doctors. Here is my outline. What am I missing? #AskRenal 

I wanted to be practical and stick with the realities of AKI management today rather than forward looking technologies that may be impactful in the future. 







Since the pretest probability that fluids will help AKI, physicians should not try to find volume depleted people, but should give fluids to everyone unless the fluids would be harmful.
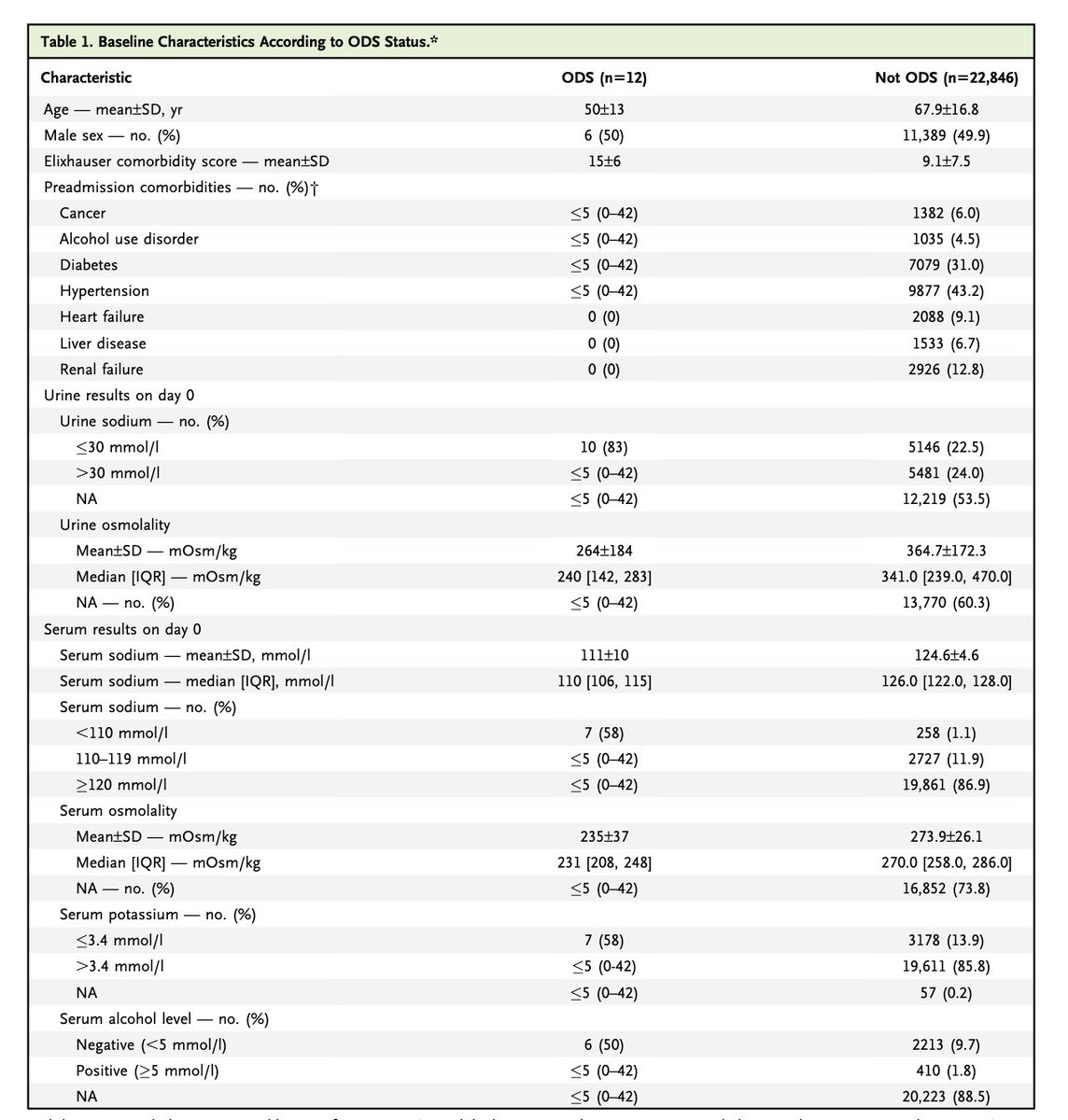
The FENa and FEUrea are “An Elegant Weapon for a More Civilized Age.” but are not very helpful on the routine evaluation of AKI. 

Urine eosinophils, please tell me your still not doing this and hopefully not teaching students to do this. 



If ~90% of AKI is fixed with a foley and some crystalloids, what about remaining 10%? Most of that is ATN and you just need to be patient. But be careful of the "Do not miss diagnosis." These require intervention. 







On to cardiorenal syndrome in a few slides. The last two show that bumps in Cr (worsening renal function if you are a cardiologist) while treating CRS do not cause kidney biomarkers to go up. MORE DIURETICS. 







STARRT, AKIKI, and IDEAL-ICU in a GIF. TL;DR: no dialysis until they need dialysis.
Furosemide stress test as GIF
• • •
Missing some Tweet in this thread? You can try to
force a refresh