
So many @CareQualityComm reports into so called care/support of learning disabled and/or autistic people.
I don't have enough hours in day to detail all of it, so back to thread with links and cpl comments each
Inadequates will be covered in detail
It's grim out there
1/25+
I don't have enough hours in day to detail all of it, so back to thread with links and cpl comments each
Inadequates will be covered in detail
It's grim out there
1/25+
These were published last wk but my soul was too tired to share them all then.
First up, Eeze Old School House in Telford - requires improvement in every area
Care home providing personal care to five people at time of the inspection (room for 7)
api.cqc.org.uk/public/v1/repo…
2/
First up, Eeze Old School House in Telford - requires improvement in every area
Care home providing personal care to five people at time of the inspection (room for 7)
api.cqc.org.uk/public/v1/repo…
2/

Although The Old School House is a smaller building, part of a local community, people still did not always have the opportunity to gain new skills or experience new things.
3/
3/
Ppl were not supported by staff to have max. possible choice, control and independence, as ppl's capacity had not been considered or best interests decisions made. There was lack of understanding around this, staff provided us with inconstant views of how ppl shd be supported
4/
4/
People were supported by enough staff, further improvements were needed to ensure staff fully understood the needs, wishes and aspirations of the people they supported.
5/
5/
When people chose not to verbally communicate, more development and understanding was needed to ensure they were involved in the home equally as the other people who lived there.
[Would love to know why ppl were choosing not to verbally communicate... ]
6/
[Would love to know why ppl were choosing not to verbally communicate... ]
6/
People... needed to be empowered to ensure they were involved with making bigger decisions.
Improvements were needed to ensure people were involved with their care and reviews and to ensure information was presented to them in a format they understood.
7/
Improvements were needed to ensure people were involved with their care and reviews and to ensure information was presented to them in a format they understood.
7/
Staff did not always have the relevant skills or experience to ensure they received the appropriate care. Although training had increased since our last inspection, we could not always see how staff had implemented this and how this had impacted on people.
8/
8/
People continued to not always be always supported by a management team and staff who fully understood the holistic needs of supporting people with learning disability and autism.
9/
9/
People were not empowered by a staff team to live a fulfilled life that included taking positive risks.
The culture of the home restricted people as the ethos, values and attitudes of the management team and staff were not empowering.
10/
The culture of the home restricted people as the ethos, values and attitudes of the management team and staff were not empowering.
10/
Was a lack of understanding around how people should be involved with the service delivery.
[So enough staff, who tick boxed their training but have no real knowledge or skill to ensure ppl lead good lives.
Yet more evidence why mandatory training aint a magic bullet]
11/
[So enough staff, who tick boxed their training but have no real knowledge or skill to ensure ppl lead good lives.
Yet more evidence why mandatory training aint a magic bullet]
11/
Last rating for this service was inadequate (published 4 May 2022) and there were breaches of regulations.
At this inspection we found the provider remained in breach of regulations. The provider had not complied with the warning notice for Regulation 11 and this remains.
12/
At this inspection we found the provider remained in breach of regulations. The provider had not complied with the warning notice for Regulation 11 and this remains.
12/
Service has been in Special Measures since 11 Mar 22. During this inspection the provider demonstrated that improvements have been made.
Service is no longer rated as inadequate overall or in any of the key questions. Therefore, this service is no longer in Special Measures
13/
Service is no longer rated as inadequate overall or in any of the key questions. Therefore, this service is no longer in Special Measures
13/
[Frighteningly, despite remaining in breach of regulation, despite the care and support sounding pretty shite, just getting enough staff on rota is enough to remove this place from special measures. I can't imagine what it's like for the 5ppl stuck there]
On to next report
14/
On to next report
14/
Next up @DimensionsUK South Hampshire Domiciliary Care Office.
They claim on their website:
Everything we do is personalised to the individual and our staff are ambitious for each and every person we support.
Let's see shall we
api.cqc.org.uk/public/v1/repo…
15/
They claim on their website:
Everything we do is personalised to the individual and our staff are ambitious for each and every person we support.
Let's see shall we
api.cqc.org.uk/public/v1/repo…
15/

At the time of this inspection people received personal care support from the service in a variety of supported living services spread across Hampshire. The service supported people with a variety of care needs, including people living with autism and learning disabilities.
16/
16/
More needed to be done to ensure that people were consistently supported to be kept safe.
Improvements were needed to ensure medicines and risks were managed in a way that ensured the best possible outcomes.
17/
Improvements were needed to ensure medicines and risks were managed in a way that ensured the best possible outcomes.
17/
Staff needed to ensure people were supported safely to make decisions and record outcomes of best interest decisions staff supported people to have the maximum possible choice, control and independence and they had control over their own lives.
18/
18/
Managers had not always ensured that risks faced by people had been assessed and planned for.
[Hmmmm.
With the country’s largest positive behaviour support team, @DimensionsUK is well placed to plan community based support for people currently in (hospital/ATUs)]
19/
[Hmmmm.
With the country’s largest positive behaviour support team, @DimensionsUK is well placed to plan community based support for people currently in (hospital/ATUs)]
19/
Staff were committed to providing an individualised response to people's needs, but this was at times difficult as there were not always enough permanent staff resulting in a high use of agency staff].
[Maybe high use agency staff shd automatically flag need for inspection]
20/
[Maybe high use agency staff shd automatically flag need for inspection]
20/
People's support plans did not always reflect their needs or demonstrate that the person's care had been reviewed.
Checks to ensure that records were effective and up to date were not always completed appropriately.
21/
Checks to ensure that records were effective and up to date were not always completed appropriately.
21/
Whilst the provider demonstrated a commitment to create a culture of improvement that provided good quality care to people, the success of this approach had been affected by changes in leadership at the service and the high use of agency staff.
22/
22/
We have identified breaches in relation to medicines, Mental Capacity Act 2005 and good governance at this inspection.
[I'm gonna dig a little deeper on this one, to see what breaches were found, given how @DimensionsUK are positioning themselves as sector experts]
23/
[I'm gonna dig a little deeper on this one, to see what breaches were found, given how @DimensionsUK are positioning themselves as sector experts]
23/
Medicine administration records (MARs) confirmed most people had received their medicines as prescribed.
However, we did see some gaps in records and a recent audit had recorded no gaps in records when there were gaps in records seen.
24/
However, we did see some gaps in records and a recent audit had recorded no gaps in records when there were gaps in records seen.
24/
We found no evidence anyone had been harmed by this, we could not be assured people were always receiving their medicines as prescribed.
[I hate statement 'found no evidence anyone had been harmed'... luck, fluke, hidden.
Not finding evidence ≠ not harmed]
25/
[I hate statement 'found no evidence anyone had been harmed'... luck, fluke, hidden.
Not finding evidence ≠ not harmed]
25/
We spoke with the registered manager about our concerns.
Their response was to re-do staff competencies and check their understanding and knowledge.
However, there was no indications they planned to investigate the errors in more detail and identify any lessons learnt.
26/
Their response was to re-do staff competencies and check their understanding and knowledge.
However, there was no indications they planned to investigate the errors in more detail and identify any lessons learnt.
26/
This placed people at increased risk of harm.
[Ongoing, increased risk of harm. Maybe @CareQualityComm should spend more time actively engaging with inquests into the deaths of learning disabled and autistic ppl to find the causal links to harm... and do more to prevent it]
27/
[Ongoing, increased risk of harm. Maybe @CareQualityComm should spend more time actively engaging with inquests into the deaths of learning disabled and autistic ppl to find the causal links to harm... and do more to prevent it]
27/
Some improvements were required for ppl's medicines administration and management...
Another person... prescribed one medicine three times a day was only being supported to have it twice a day according to their MAR records. This had not been picked up by the provider.
28/
Another person... prescribed one medicine three times a day was only being supported to have it twice a day according to their MAR records. This had not been picked up by the provider.
28/
[And we wonder why so many learning disabled people die from poorly managed epilepsy, with the get out of jail SUDEP card... or constipation... or any manner of illnesses/health conditions managed with medication.
When someone dies the paperwork nearly always goes missing]
29/
When someone dies the paperwork nearly always goes missing]
29/
Information about people's medicines was not always recorded consistently across different records. Protocols for the use of 'when required' or 'PRN' medicines were not always available or lacked information.
[PBS experts remember...with this level of attention to detail]
30/
[PBS experts remember...with this level of attention to detail]
30/
We found no evidence that people had been harmed however, medicines were not always robust enough to keep people safe.
This demonstrates a breach of Regulation 12 (Safe care and treatment) of The Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
31/
This demonstrates a breach of Regulation 12 (Safe care and treatment) of The Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
31/
We viewed many records across different services provided by the provider and most had information to keep people safe and were sufficiently detailed.
[Most isn't good enough really is it, when we're talking in life and death, care and support]
32/
[Most isn't good enough really is it, when we're talking in life and death, care and support]
32/
However, one person's epilepsy support plan did not contain detailed information on their epilepsy and how to support them to manage it safely.
[Remember this is a service with a high reliance on agency staff... and poor risk assessments... and missed medication....]
33/
[Remember this is a service with a high reliance on agency staff... and poor risk assessments... and missed medication....]
33/
The service was having difficulty recruiting permanent members of staff and as a result had a high use of agency staff to cover the gaps in staffing and in one service we visited 90 % of the staff were agency staff.
34/
34/
Staff told us "Recruitment is difficult, but we always seem to cover the shift or at least make it safe for the people we support"
[Are they making it safe though? For people to live a life? Families may report their loved one is safe, but how would they actually know?]
35/
[Are they making it safe though? For people to live a life? Families may report their loved one is safe, but how would they actually know?]
35/
Staff told us, "Safe minimum staffing levels are always achieved, but there have been times that the people we support have not received all of the hours they are funded for in order to access the community."
[Does the money for support not received get returned?]
36/
[Does the money for support not received get returned?]
36/
The provider was not acting in accordance with the MCA and were not following the Deprivation of Liberty Safeguards.
We spoke with some of the registered managers about applications made to the court of protection.
37/
We spoke with some of the registered managers about applications made to the court of protection.
37/
There was some confusion about who had an application in place and if they were authorised.
We saw no records that people had an application in place.
We were informed that the operations director was looking at these ... part of a service improvement plan.
38/
We saw no records that people had an application in place.
We were informed that the operations director was looking at these ... part of a service improvement plan.
38/
We found that some significant decisions were being made without following legal frameworks.
We spoke to the registered managers across the service and some informed us they were in place and would send these to the inspector to review remotely.
39/
We spoke to the registered managers across the service and some informed us they were in place and would send these to the inspector to review remotely.
39/
We did receive some records. However, for one person there was concerns about locked doors and no MCA or best interest decision was in place to support this.
[Some not all. Not following the law, pah, but Dimensions claim they're well placed to get ppl out of ATUs]
40/
[Some not all. Not following the law, pah, but Dimensions claim they're well placed to get ppl out of ATUs]
40/
Failure to follow legal frameworks of the MCA is a breach of Regulation 13 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014; Safeguarding service users from abuse and improper treatment.
41/
41/
Care plans described people's needs in a range of areas including personal care, oral health and daily living activities.
However, one relative told us "Oral hygiene is not best. He has had to have a tooth out because they were not helping him to clean his teeth properly."
42/
However, one relative told us "Oral hygiene is not best. He has had to have a tooth out because they were not helping him to clean his teeth properly."
42/
[When @CareQualityComm say they find no evidence of harm, what is this exactly?
Remember Rachel Johnston, who died after having all her teeth removed.
Much anger was misdirected at the dentist.
It wasn't the dentist that caused her teeth to rot] georgejulian.co.uk/inquests/rache…
43/
Remember Rachel Johnston, who died after having all her teeth removed.
Much anger was misdirected at the dentist.
It wasn't the dentist that caused her teeth to rot] georgejulian.co.uk/inquests/rache…
43/
Each registered manager had several services they managed. Working alongside assistant managers in people's homes. This was a new role for staff as before the service was managed by one registered manager.
44/
44/
Not all registered managers we spoke with were happy having the responsibility of being a registered manager.
One staff member told us, "I have worked with Dimensions for a long time. I find that although line managers work very hard the infrastructure is ineffective..."
45/
One staff member told us, "I have worked with Dimensions for a long time. I find that although line managers work very hard the infrastructure is ineffective..."
45/
"I often find it frustrating with the on call service, staff not turning up and when you contact on call their answer is often call agency, well if this is a night shift myself and my colleagues that have supposed to finish at 22.00 end up staying to cover the night..."
46/
46/
"...impacting on the next day. Senior managers need to be more supportive to line managers so they can be more involved with what's going on with the frontline staff. There are many times I personally feel undervalued by senior managers...."
47/
47/
"...The people we support are well looked after but that is down to the frontline staff."
There were a number of systems and processes in place for monitoring the quality of care. These included STOMP and quarterly health and safety audits.
48/
There were a number of systems and processes in place for monitoring the quality of care. These included STOMP and quarterly health and safety audits.
48/
However, we found these were not always effective in medicines audits.
We could not see audits on care plans, and some viewed were unclear when written, last updated or reviewed.
[Performative scrutiny, tick box processes, non action]
49/
We could not see audits on care plans, and some viewed were unclear when written, last updated or reviewed.
[Performative scrutiny, tick box processes, non action]
49/
One registered manager seemed surprised there were concerns with the care plans as they told us they would have all been completed when Dimensions took over service in July 2019. We asked them how often they should be reviewed and they didn't seem to know.
[3yrs, no review]
50/
[3yrs, no review]
50/
Provider audits were also in place to review the service's progress.
Audits viewed were not always effective as some of the concerns identified during the inspection hadn't been picked up on.
We found no evidence that people had been harmed however...
51/
Audits viewed were not always effective as some of the concerns identified during the inspection hadn't been picked up on.
We found no evidence that people had been harmed however...
51/
...systems were either not in place or robust enough to ensure the quality and safety of the service was assessed and monitored effectively. The above evidence is a breach of Regulation 17 of the Health and Social Care Act 2008 (Regulated Activities) Regulation 2014
52/
52/
There was an open and transparent culture in the service.
Staff member told us "I have always found Dimensions to be open and honest, they aren't perfect but if they make a mistake, they will admit to the mistake and do all in their power to rectify it."
[If they notice]
53/
Staff member told us "I have always found Dimensions to be open and honest, they aren't perfect but if they make a mistake, they will admit to the mistake and do all in their power to rectify it."
[If they notice]
53/
[Here's the deal. Their audit systems clearly aint up to scratch. They aren't identifying issues. They aren't providing medication safely. Services reliant on 90% agency staff... so being open and honest aint that straight forward is it]
Report and action plans needed
54/
Report and action plans needed
54/

Next up @autismwestmids Gorse Farm which despite the name is a residential care home not a petting zoo.
It can provide for 14 ppl with a sensory impairment, learning disability or autism, but had 13 residents at time of inspection
api.cqc.org.uk/public/v1/repo…
55/
It can provide for 14 ppl with a sensory impairment, learning disability or autism, but had 13 residents at time of inspection
api.cqc.org.uk/public/v1/repo…
55/

Environmental risk and some aspects of medicine management required improvement. Some action was taken to address this.
The prevention and control of infection was not always managed safely and in line with the provider's guidance and procedures.
56/
The prevention and control of infection was not always managed safely and in line with the provider's guidance and procedures.
56/
Service oversight and audits used to monitor the quality and safety of the service required improvement.
Last rating for this service was good (19 June 2018). Overall rating for the service has changed from good to requires improvement based on findings of this inspection.
57/
Last rating for this service was good (19 June 2018). Overall rating for the service has changed from good to requires improvement based on findings of this inspection.
57/
This service is required to have a registered manager.
At the time of our inspection there was not a registered manager in post. The manager had submitted an application to register with us. The manager was not present on the day of the inspection.
58/
At the time of our inspection there was not a registered manager in post. The manager had submitted an application to register with us. The manager was not present on the day of the inspection.
58/
This inspection was unannounced.
We were not assured the provider was using Personal Protective Equipment (PPE) effectively and safely.
We saw one staff member was not wearing a face mask whilst supporting a person.
59/
We were not assured the provider was using Personal Protective Equipment (PPE) effectively and safely.
We saw one staff member was not wearing a face mask whilst supporting a person.
59/
Throughout the inspection other staff, including senior support workers, were observed wearing their face masks under their chins and noses.
[How hard is it. If ppl can't wear masks on their mouths and noses in front of @CareQualityComm inspectors]
60/
[How hard is it. If ppl can't wear masks on their mouths and noses in front of @CareQualityComm inspectors]
60/
Used personal protective equipment had been disposed of in domestic waste bins, some of which did not have lids and were not pedal operated. This posed a risk of cross contamination.
61/
61/
We were not assured the provider was promoting safety through the layout and hygiene practices of the premises.
Staff had not consistently completed cleaning schedules and records were not available to show frequently touched points for example, door handles, were cleaned.
62/
Staff had not consistently completed cleaning schedules and records were not available to show frequently touched points for example, door handles, were cleaned.
62/
Some completed cleaning schedules contained inaccurate information.
One recorded the kitchen had been deep cleaned. We saw all areas of the kitchen were dirty.
This was an infection prevention and control (IPC) risk and increased the risk of infection transmission.
63/
One recorded the kitchen had been deep cleaned. We saw all areas of the kitchen were dirty.
This was an infection prevention and control (IPC) risk and increased the risk of infection transmission.
63/
[Of course it's also a lie. A blatant lie.
Why is there no real consequence for "inaccurate information"... given how important things are to keeping people safe and having a good life?
The state of record keeping is beyond woeful across the board with zero consequence]
64/
Why is there no real consequence for "inaccurate information"... given how important things are to keeping people safe and having a good life?
The state of record keeping is beyond woeful across the board with zero consequence]
64/
We were not assured provider was preventing visitors from catching and spreading infections.
Staff permitted CQC inspectors to enter home without asking for their lateral flow test results and taking or checking temperatures to make sure their visit cld take place safely.
65/
Staff permitted CQC inspectors to enter home without asking for their lateral flow test results and taking or checking temperatures to make sure their visit cld take place safely.
65/
In addition, records for May to June did not show staff had checked their temperatures prior to starting their shift. This was IPC poor practice and placed people at risk.
We found no evidence that people had been harmed however the provider's guidance was not followed...
66/
We found no evidence that people had been harmed however the provider's guidance was not followed...
66/
...to ensure risk associated with infection prevention and control was effectively managed. This placed people at risk of harm. This was a breach of regulation 12 (Safe Care and Treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
67/
67/
At our last inspection, improvements had been made to ensure medicines were managed safely in line with the provider policy and best practice guidance.
At this inspection we found some of these improvements had not been maintained.
68/
At this inspection we found some of these improvements had not been maintained.
68/
Medication administration records (MAR) showed two people were prescribed a medicated toothpaste.
Both people's MAR charts were inaccurate and did not record if this medicine was being consistently used.
[Again, remember Rachel Johnston and have you ever had toothache?]
69/
Both people's MAR charts were inaccurate and did not record if this medicine was being consistently used.
[Again, remember Rachel Johnston and have you ever had toothache?]
69/
Environmental risk had not always been identified and mitigated.
Ground floor lounge windows did not have window restrictors... This was unsafe. Immediate action was taken to fit window restrictors during our inspection.
[First inspection in 4yrs. Four years of risk]
70/
Ground floor lounge windows did not have window restrictors... This was unsafe. Immediate action was taken to fit window restrictors during our inspection.
[First inspection in 4yrs. Four years of risk]
70/
People and relatives said staff were available when needed.
However, relatives had some concerns about the high use of agency staff.
One relative said, "The problem is they use so many agency and I don't know if they know [names] needs."
71/
However, relatives had some concerns about the high use of agency staff.
One relative said, "The problem is they use so many agency and I don't know if they know [names] needs."
71/
The home had a number of staff vacancies which were covered by agency staff. A permanent staff member said, "Consistency is important for the residents We use the same agency staff. It works well."
[If you're using agency staff that regularly, surely they shd be employees]
72/
[If you're using agency staff that regularly, surely they shd be employees]
72/
Provider and manager level oversight of the service required improvement. Limited oversight meant some previously evidenced standards and areas of regulatory compliance had not been maintained.
73/
73/
The provider's systems to monitor the quality and safety of the service were not always effective.
The provider had not ensured staff followed their guidance and procedures to prevent and control the
spread of infection.
74/
The provider had not ensured staff followed their guidance and procedures to prevent and control the
spread of infection.
74/
We found no evidence that people had been harmed, however service oversight and governance systems were not effective.
This was a breach of Regulation 17 (Good Governance) of The Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
75/
This was a breach of Regulation 17 (Good Governance) of The Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
75/
Throughout our inspection the operations director and manager were open and honest.
They welcomed our inspection and acknowledged our inspection findings.
The manager said "We have come a long way. Really positive things are happening..."
[Welcomed, 4yrs without scrutiny]
76/
They welcomed our inspection and acknowledged our inspection findings.
The manager said "We have come a long way. Really positive things are happening..."
[Welcomed, 4yrs without scrutiny]
76/
"There are things we need to do, things I want to do and will do. My focus is ensuring they (people) have the best quality of life and staff want to stay because Gorse Farm is the best place to work."
[They.
Good to require improvement in 4yrs.
Really positive things]
77/
[They.
Good to require improvement in 4yrs.
Really positive things]
77/

Next Essex Shared Lives
[It's not clear from @CareQualityComm report whether they are supporting people with learning disabilities and/or autism but their own website advertises as got a spare room? "Willing" to support adults with care and support needs such as LD/autism]
78/
[It's not clear from @CareQualityComm report whether they are supporting people with learning disabilities and/or autism but their own website advertises as got a spare room? "Willing" to support adults with care and support needs such as LD/autism]
78/

[Such interesting phraseology... are you willing to support... like it's a gift, or favour.
Where I live we get this advertising for host families for international students coming to Torbados (which really isn't a city) for the summer, but at least it's sold as reciprocal]
79/

Where I live we get this advertising for host families for international students coming to Torbados (which really isn't a city) for the summer, but at least it's sold as reciprocal]
79/


Anyhow, What did CQC find at Shared Lives Essex run by @Essex_CC
Although the scheme has been operational since 2007, it is only since June 2021 that the scheme was integrated within Essex County Council.
api.cqc.org.uk/public/v1/repo…
80/
Although the scheme has been operational since 2007, it is only since June 2021 that the scheme was integrated within Essex County Council.
api.cqc.org.uk/public/v1/repo…
80/

The shared lives scheme provides people aged 18 years and over with long-term placements, short breaks and respite care, within shared lives carers [SLC] own homes. At the time of our inspection the Essex Shared Lives scheme was supporting 45 adults.
81/
81/
24 out of 45 people were receiving the regulated activity of personal care.
Since January 2022, the term 'shared lives carers' was no longer being used by the Essex Shared Live scheme. Throughout this report we have used the term shared live hosts.
[Hosts... right]
82/
Since January 2022, the term 'shared lives carers' was no longer being used by the Essex Shared Live scheme. Throughout this report we have used the term shared live hosts.
[Hosts... right]
82/
Following the service being transferred to Essex County Council in June 2021 from another provider, the above arrangements identified there were significant gaps in record keeping relating to people using the service and existing shared live hosts.
83/
83/
Above related to people's support plans, risk management strategies, Medication Administration Records and included training shortfalls for shared live hosts. However, there was no evidence to demonstrate this impacted on the support being provided for ppl using service.
84/
84/
Steps were being taken by Essex Shared Lives to address these shortfalls.
[Head wrecking... significant gaps... yet no evidence it impacted on support provided.
Either it's all unnecessary in first place, so stop with training fanfare, or impact is just not 'evidenced']
85/
[Head wrecking... significant gaps... yet no evidence it impacted on support provided.
Either it's all unnecessary in first place, so stop with training fanfare, or impact is just not 'evidenced']
85/
Not all shared live hosts had up to date or completed training relating to safeguarding vulnerable people.
Registered manager told us this training was being prioritised as a matter of urgency.
[A whole year after taking over. I wish @CareQualityComm would define urgency]
86/
Registered manager told us this training was being prioritised as a matter of urgency.
[A whole year after taking over. I wish @CareQualityComm would define urgency]
86/
The registered manager confirmed they were in the process of recruiting additional shared live officers to support the existing team. Not all shared live officers felt current caseloads were manageable in the longer term and stated their caseload could be overwhelming.
87/
87/
The registered manager confirmed recruitment to the team for additional staff members were proceeding
[Always. Always just happening. Planned for. Starting. @essex_cc had been providing this service for a year at this point, and presumably commissioning it before then]
88/
[Always. Always just happening. Planned for. Starting. @essex_cc had been providing this service for a year at this point, and presumably commissioning it before then]
88/
Information viewed for two people showed an additional family member was on occasions either providing personal care and/or looking after the person using the service to give the shared live host a break.
89/
89/
The previous organisation had not completed the vetting and assessment process or approved either family member as a shared lives respite host.
This remained outstanding at this inspection and had not been picked by Essex Shared Lives
[@essex_CC hadn't even noticed]
90/
This remained outstanding at this inspection and had not been picked by Essex Shared Lives
[@essex_CC hadn't even noticed]
90/
Not all shared lives hosts had up to date or completed training on how to safely support people with their medicines.
The registered manager told us this training was being prioritised as a matter of urgency.
[A year in, urgent, pah it's only medication]
91/
The registered manager told us this training was being prioritised as a matter of urgency.
[A year in, urgent, pah it's only medication]
91/
Not all shared lives hosts had up to date or completed training relating to infection control.
[No statement that the registered manager told CQC it was being prioritised as a matter of urgency, so I guess infection control aint urgent, in a global pandemic. Who knows]
92/
[No statement that the registered manager told CQC it was being prioritised as a matter of urgency, so I guess infection control aint urgent, in a global pandemic. Who knows]
92/
People told us their shared live hosts were kind, caring and supportive. One person told us, "[Shared Live Host] is wonderful to me, they do everything for me. [Shared Live Host] looks after me."
93/
93/
People told us they had a good rapport and relationship with the hosts, and this included extended family members.
Hosts spoke fondly and warmly about the people they supported. Shared live hosts told us people were fully integrated with their families and 'family life'.
94/
Hosts spoke fondly and warmly about the people they supported. Shared live hosts told us people were fully integrated with their families and 'family life'.
94/
Essex Shared Live team members commented that due to the registered manager's role and responsibilities, they spent a lot of their time attending meetings and this impacted on the amount of time they were available for support and advice.
[No breaches/no required action]
95/
[No breaches/no required action]
95/
Bridgeway Care Home, Preston
Residential care home providing personal and nursing care.
Provides support to adults aged between 18 and 65... with a physical disability and adults with a learning disability and or autistic spectrum disorder.
api.cqc.org.uk/public/v1/repo…
96/
Residential care home providing personal and nursing care.
Provides support to adults aged between 18 and 65... with a physical disability and adults with a learning disability and or autistic spectrum disorder.
api.cqc.org.uk/public/v1/repo…
96/

[Registered support 29 ppl, 28 at time of inspection]
Care took place within a care home environment making it difficult to have different opportunities to maximise people's choice, control and independence. However, at times people were supported with their own interests
97/
Care took place within a care home environment making it difficult to have different opportunities to maximise people's choice, control and independence. However, at times people were supported with their own interests
97/
The last rating for this service was good (published 18 August 2021).
At our last inspection we made recommendations about the incident recording process and audits. At this inspection we found that some improvements had been made in these areas.
[Some]
98/
At our last inspection we made recommendations about the incident recording process and audits. At this inspection we found that some improvements had been made in these areas.
[Some]
98/
Overall rating for the service has changed from good to requires improvement based on the findings of this inspection.
We have identified a breach in relation to the safe management of medicines at this inspection.
This inspection was unannounced.
99/
We have identified a breach in relation to the safe management of medicines at this inspection.
This inspection was unannounced.
99/
Some aspects of the service were not always safe and there was limited assurance about safety.
There was an increased risk that people could be harmed.
The service did not always manage medicines safely.
100/
There was an increased risk that people could be harmed.
The service did not always manage medicines safely.
100/
We found a container of 'thickener' left in a communal area, which was not locked away.
Thickeners are added to drinks to make them safer for people who are at risk of choking.
Accidental ingestion of thickener could cause harm.
101/
Thickeners are added to drinks to make them safer for people who are at risk of choking.
Accidental ingestion of thickener could cause harm.
101/
Two people were prescribed thickeners according to their care plans.
Staff described using different amounts of thickener to what care plans stated, and we cld not see any instructions for staff in kitchen or dining room.
[We know this is how learning disabled ppl die]
102/
Staff described using different amounts of thickener to what care plans stated, and we cld not see any instructions for staff in kitchen or dining room.
[We know this is how learning disabled ppl die]
102/
Staff did not record how much thickener they added to people's drinks.
This meant there was a risk the wrong amount of thickener could be added to a person's drink.
Although we found no harm as a result, safe use of medicines and thickeners had not been established...
103/
This meant there was a risk the wrong amount of thickener could be added to a person's drink.
Although we found no harm as a result, safe use of medicines and thickeners had not been established...
103/
...to protect people that used the service.
This placed people at risk of harm.
This was a breach of regulation 12(1) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
[Altho we found no harm... how cld CQC find harm except by chance?]
104/
This placed people at risk of harm.
This was a breach of regulation 12(1) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
[Altho we found no harm... how cld CQC find harm except by chance?]
104/
At the last inspection we made a recommendation about how incidents were recorded and monitored. The provider had made improvements.
There was a new electronic system in place and staff were starting to record incidents on this
[Starting, always starting, but wait for it]
105/
There was a new electronic system in place and staff were starting to record incidents on this
[Starting, always starting, but wait for it]
105/
Some further updates were needed to the electronic system to make sure that themes and lessons learned could be recorded, as these were still being recorded on paper.
Registered manager audited incidents to find out if there were any themes.
106/
Registered manager audited incidents to find out if there were any themes.
106/
For example, around falls and actions were taken to minimise the risk of these for people
[But the very same registered manager and shiny new electronic system hadn't identified the very real risks of inappropriate care being given to someone at risk of choking]
107/
[But the very same registered manager and shiny new electronic system hadn't identified the very real risks of inappropriate care being given to someone at risk of choking]
107/
Service management and leadership was inconsistent. This meant the service leadership, management and governance did not always ensure the delivery of high-quality, person-centred care.
108/
108/
At our last inspection we made a recommendation about recording more detail in the auditing process.
Although some improvements had been made, the medicines audit did not highlight issues about the safe management of medicines that we found during this inspection.
109/
Although some improvements had been made, the medicines audit did not highlight issues about the safe management of medicines that we found during this inspection.
109/
We recommend the provider reviews their auditing processes to make sure issues are identified and acted
upon in a timely manner.
[So much review, so much time to just stop, reflect and consider, while people's lives are at risk of harm]
110/
upon in a timely manner.
[So much review, so much time to just stop, reflect and consider, while people's lives are at risk of harm]
110/
Although there was a registered manager in post, they were also the proprietor of this home and another, which could cause difficulties in providing a high level of oversight for Bridgeway Care Home.
[Surely there should be a limit?]
111/
[Surely there should be a limit?]
111/
To prevent such difficulties, the provider told us they were actively recruiting a different registered manager however had not yet found someone suitable
[One action required to be taken - report and action plan]
112/
[One action required to be taken - report and action plan]
112/

Buckle up, time for another, from the leading voice of learning disability @mencap_charity
And again they're found to require improvement...
Again when are @ChtyCommission going to start paying attention to charities providing poor care
api.cqc.org.uk/public/v1/repo…
113/
And again they're found to require improvement...
Again when are @ChtyCommission going to start paying attention to charities providing poor care
api.cqc.org.uk/public/v1/repo…
113/

A supported living service providing personal care to people with a learning disability and autistic people
This service provides care and support to 27 people living in eight 'supported living' settings so that they can live in their own home as independently as possible
114/
This service provides care and support to 27 people living in eight 'supported living' settings so that they can live in their own home as independently as possible
114/
CQC does not regulate premises used for supported living; this inspection looked at people's personal care and support.
[No-one regulates Supported Living. Mencap have a spin out arm called @GoldenLaneHouse providing it altho am not sure if they're the provider here]
115/
[No-one regulates Supported Living. Mencap have a spin out arm called @GoldenLaneHouse providing it altho am not sure if they're the provider here]
115/
Not everyone who used the service received personal care. CQC only inspects where people receive personal care. This is help with tasks related to personal hygiene and eating. Where they do, we also consider any wider social care provided.
116/
116/
There were some risks for people with dysphagia (swallowing difficulties) as staff were not consistently following expert guidelines on supporting some people with eating and drinking.
117/
117/
The care two people needed at night time was not written clearly so there was a risk they may have unmet needs during the night.
118/
118/
There were some safety concerns where two people had not been protected from the risk of avoidable harm. In both cases people had been at risk of harm from a person they lived with.
[Who arranged for these people to live together? Who provided support? Who didn't notice?]
119/
[Who arranged for these people to live together? Who provided support? Who didn't notice?]
119/
The provider had implemented new initiatives to improve the culture within services.
This had not yet been implemented in this service but staff were preparing for it.
[Always planning. Always due to improve. Always]
120/
This had not yet been implemented in this service but staff were preparing for it.
[Always planning. Always due to improve. Always]
120/
Last rating for this service was good (published 17/07/2018).
The inspection was prompted in part by notification of a specific incident. This incident is subject to a criminal investigation. As a result, this inspection did not examine the circumstances of the incident.
121/
The inspection was prompted in part by notification of a specific incident. This incident is subject to a criminal investigation. As a result, this inspection did not examine the circumstances of the incident.
121/
The information CQC received about the incident indicated concerns about the management of risk and safeguarding people from abuse.
This inspection examined those risks.
The overall rating for the service has changed from good to requires improvement
122/
This inspection examined those risks.
The overall rating for the service has changed from good to requires improvement
122/
We have found evidence that the provider needs to make improvements.
We have identified breaches in relation to keeping people safe, safeguarding people from risk of abuse and the management of the service at this inspection.
123/
We have identified breaches in relation to keeping people safe, safeguarding people from risk of abuse and the management of the service at this inspection.
123/
We gave the service notice of the inspection. This was because we wanted to be sure the registered manager would be available at the office and to arrange to visit people in their homes.
[Always interesting which settings get advance warning]
124/
[Always interesting which settings get advance warning]
124/
Inspection activity started on 18 May 2022 and ended on 31 May. We visited the office location on 18 May and three of supported living houses on 24 May. On other days we reviewed records, spoke with relatives, people using the service and staff in telephone and video calls.
125/
125/
People were not always protected from the risks of abuse.
There had been incidents where the service had failed to protect a person from the risk of abuse by another person in the service where they lived.
[How can this be?]
126/
There had been incidents where the service had failed to protect a person from the risk of abuse by another person in the service where they lived.
[How can this be?]
126/
The service had also not responded in the quickest and most appropriate way to these incidents to protect people
[Maybe @mencap_charity should quit wasting resources on training campaigns, myth busting nonsense and actually just sort themselves out. It's shameful]
127/
[Maybe @mencap_charity should quit wasting resources on training campaigns, myth busting nonsense and actually just sort themselves out. It's shameful]
127/
We found for two people insufficient action had been taken to protect them from the risk of being assaulted by another person who lived with them.
[What is the point of @mencap_charity Anyone?]
128/
[What is the point of @mencap_charity Anyone?]
128/
Records showed one person was at risk of being physically assaulted by a person they lived with and no risk assessment had been undertaken to minimise this risk.
[The same organisation who are banging on about mandatory training for others. Can't do the basics]
129/
[The same organisation who are banging on about mandatory training for others. Can't do the basics]
129/
The person's representative had not been informed and there were no records of any action taken to support this person.
[Which has to raise question of how reliable family feedback to @CareQualityComm can ever be... ppl often don't know the reality their relatives endure]
130/
[Which has to raise question of how reliable family feedback to @CareQualityComm can ever be... ppl often don't know the reality their relatives endure]
130/
When we brought this concern to the attention of a senior manager, they took action to raise a safeguarding alert and a person's risk assessment was updated but this did not mention the specific risk of the person physically assaulting the other person.
131/
131/
This risk was not included in either person's risk assessment despite staff knowing about this risk.
One person raised a concern which was about possible psychological abuse which we passed to the registered manager to investigate.
132/
One person raised a concern which was about possible psychological abuse which we passed to the registered manager to investigate.
132/
This was being investigated at the time of writing this report and the outcome not yet known.
Failure to safeguard people from risk of abuse left people at risk of harm.
This was a breach of Regulation 13
[No words]
133/
Failure to safeguard people from risk of abuse left people at risk of harm.
This was a breach of Regulation 13
[No words]
133/
The provider took immediate steps to safeguard a person following this inspection.
[Imagine @mencap_charity needing this pointing out to them. Leading voice of learning disability... sitting at govt tables... supporting dodgy legal cases and campaigns. Can't safeguard ppl]
134/
[Imagine @mencap_charity needing this pointing out to them. Leading voice of learning disability... sitting at govt tables... supporting dodgy legal cases and campaigns. Can't safeguard ppl]
134/
The provider had taken steps to review and improve the management of people's finances following an incident of financial abuse to minimise the risk of this happening again.
[What the hell is going on here?]
135/
[What the hell is going on here?]
135/
Relatives felt assured their relative was safe and treated well. One relative told us; "They cater for his safeguarding very well" and "They always let us know of any incidents."
[Your report just stated relatives weren't told. Mind boggling in the denial of reality here]
136/
[Your report just stated relatives weren't told. Mind boggling in the denial of reality here]
136/
People were not consistently protected against known risks to their safety.
People had individual risk assessments which included guidance for staff on supporting people to stay safe, however we identified some risks to people's safety.
137/
People had individual risk assessments which included guidance for staff on supporting people to stay safe, however we identified some risks to people's safety.
137/
Records showed that there was only one member of staff on duty sleeping in one service at night.
The risk of fire and how one staff member could safely evacuate the home had not been appropriately assessed.
There was no clear night-time fire procedure.
138/
The risk of fire and how one staff member could safely evacuate the home had not been appropriately assessed.
There was no clear night-time fire procedure.
138/
Staff had no guidance on how to support people outside the service safely once evacuated.
The fire risk assessment and fire procedure did not address the specific risks.
139/
The fire risk assessment and fire procedure did not address the specific risks.
139/
People had personal emergency evacuation plans but these were online only and therefore not available for staff to quickly refer to and share with fire brigade in event of a fire at night.
Staff were not clear about how to evacuate ppl safely if there was a fire at night
140/
Staff were not clear about how to evacuate ppl safely if there was a fire at night
140/
[Ahhh yes @mencap_charity who took legal action to prevent care workers being paid minimum wage at night... who don't provide enough waking night staff.... who put ppl at risk.
Dont think anyone will be surprised at this really]
141/
Dont think anyone will be surprised at this really]
141/
For two people there was a lack of written guidance on what support they needed at night.
One person was checked on every hour during the night, but their support plan stated they should be checked three times during the night.
142/
One person was checked on every hour during the night, but their support plan stated they should be checked three times during the night.
142/
There was no evidence to suggest this person was not supported safely but practice and guidance did not match so there was a risk that staff on duty at night may not follow current guidelines.
[At least they were providing overly restrictive support I suppose]
143/
[At least they were providing overly restrictive support I suppose]
143/
One person's risk assessment stated they shd be monitored half hourly due to risk of choking, but their support plan gave different information, to visually check three times a night plus epilepsy and audio monitor all night but did not specify what staff should be checking
144/
144/
Night care records did not specify at what time staff checked on the person.
[Oh come on, if records didn't specify what time checked, do we believe ppl are checked?
Nominated individual John Cowman, who instructed legal counsel at @TozerInquest georgejulian.co.uk/inquests/danny…]
145/
[Oh come on, if records didn't specify what time checked, do we believe ppl are checked?
Nominated individual John Cowman, who instructed legal counsel at @TozerInquest georgejulian.co.uk/inquests/danny…]
145/

Both people were supported with continence and changing position regularly during the day but did not have a night support plan stating whether they needed the same support during the night.
146/
146/
One person's pressure care support plan said they were not repositioned at night as there was only funding for one waking night staff but did not state whether the person needed any support for their safety or comfort at night.
[Imagine the discomfort for that person]
147/
[Imagine the discomfort for that person]
147/
Some ppl had dysphagia (swallowing difficulties) and had written guidelines from Speech and Language Therapists on how to support them to eat and drink safely following an assessment.
Guidelines were clearly displayed in kitchens of each house for staff to follow.
148/
Guidelines were clearly displayed in kitchens of each house for staff to follow.
148/
Guidelines and eating and drinking support plans in place were accessible and mostly very detailed but practice did not always match guidelines.
[How many times? Known risks.
"Problems with eating and drinking can be life-threatening" @mencap_charity Treat Me Right 2004]
149/
[How many times? Known risks.
"Problems with eating and drinking can be life-threatening" @mencap_charity Treat Me Right 2004]
149/
We looked at the food records for four people and observed a mealtime with three people. Staff were not following the guidelines for the four people.
One person's guidelines stated that meat needed to be minced or pureed and meals with mixed textures were not recommended
150/
One person's guidelines stated that meat needed to be minced or pureed and meals with mixed textures were not recommended
150/
Records of food eaten and discussion with staff showed this person was regularly being served meals with mixed textures and meat which was not minced or pureed.
Staff were trained in supporting people to eat and drink safely, their competence was assessed by a manager...
151/
Staff were trained in supporting people to eat and drink safely, their competence was assessed by a manager...
151/
...who would observe them supporting a person at a mealtime.
We noted that a staff member had been assessed as competent when supporting this person to eat a high-risk food which it was not clear they could eat safely.
[No words]
152/
We noted that a staff member had been assessed as competent when supporting this person to eat a high-risk food which it was not clear they could eat safely.
[No words]
152/
A second person had written guidelines stating that they should eat soft and bitesize foods cut into 1.5- centimetre pieces.
We observed this person eating a meal that did not comply with these guidelines.
[This is how learning disabled people die]
153/
We observed this person eating a meal that did not comply with these guidelines.
[This is how learning disabled people die]
153/
A third person had specific guidance for two staff to support them in a specific way at mealtimes.
We observed that this support did not take place.
Although the eating and drinking support plan had been recently reviewed staff were not following the guidance...
154/
We observed that this support did not take place.
Although the eating and drinking support plan had been recently reviewed staff were not following the guidance...
154/
and it was not clear whether the guidance reflected the person's current needs which staff said had changed.
A staff member told us there were specific foods this person could not eat as they caused coughing, but we noted all these foods were on the menu for that week...
155/
A staff member told us there were specific foods this person could not eat as they caused coughing, but we noted all these foods were on the menu for that week...
155/
... there was no accessible list of these foods available to refer to so there was a risk staff may give the person one of these foods.
Altho ppl did not experience harm and we did not see anyone struggling with their meal, there was a risk staff did not fully understand
156/
Altho ppl did not experience harm and we did not see anyone struggling with their meal, there was a risk staff did not fully understand
156/
...the speech and language therapy eating and drinking guidelines and therefore may have been giving unsafe meals.
[We did not see anyone struggling with their meal... while observing one meal time....]
157/
[We did not see anyone struggling with their meal... while observing one meal time....]
157/
This meant there was a risk of staff not supporting people safely with eating and drinking due to discrepancy between records and practice.
The provider failed to accurately assess and mitigate risks to people's safety. This was a breach of regulation 12
158/
The provider failed to accurately assess and mitigate risks to people's safety. This was a breach of regulation 12
158/
People's medicines were generally managed safely but there were some risks not addressed.
One person's medicines admin record stated there were no known allergies but another document stated the person should not be given a specific medicine as they might be allergic to it
159/
One person's medicines admin record stated there were no known allergies but another document stated the person should not be given a specific medicine as they might be allergic to it
159/
Where two people had prescribed topical medicines (patches, creams etc) the MAR did not specify the part of the body where staff should apply creams.
One person's MAR was signed twice a day when the medicine was prescribed for once a day. This appeared to be an admin error
160/
One person's MAR was signed twice a day when the medicine was prescribed for once a day. This appeared to be an admin error
160/
[Apathetic and care-less
Medicines
Feeding
Getting people out in a fire
These are not complicated things, these are the basics.
@mencap_charity who want:
"the UK to be the best place in the world for people with a learning disability to live happy and healthy lives"
161/
Medicines
Feeding
Getting people out in a fire
These are not complicated things, these are the basics.
@mencap_charity who want:
"the UK to be the best place in the world for people with a learning disability to live happy and healthy lives"
161/
2ppl's "how to support at home" plans stated medicines shd be placed in pot on top of food. Another document said mix medicine with thickener 2.5 spoons to 160ml medicines
Neither person took 160ml medicine, was a lack of clear written guidance how staff shd support people
162/
Neither person took 160ml medicine, was a lack of clear written guidance how staff shd support people
162/
One person's MAR indicated they were given a "when needed" medicine every morning.
There was no clear protocol for when this person should have this medicine.
[As needed. Whenever. Just give it. @mencap_charity who're always on about STOMP]
163/
There was no clear protocol for when this person should have this medicine.
[As needed. Whenever. Just give it. @mencap_charity who're always on about STOMP]
163/
Where a medicine was prescribed as a variable dose (i.e. give one or two) staff didn't record whether they had given one or two tablets.
Whilst we found no evidence that people had been harmed, the provider failed to manage some people's medicines safely.
164/
Whilst we found no evidence that people had been harmed, the provider failed to manage some people's medicines safely.
164/
This placed people at risk of harm and was a breach of Regulation 12 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
165/
165/
Service management and leadership was inconsistent. Leaders and the culture they created did not always support the delivery of high-quality, person-centred care.
The provider had a quality team who carried out audits in the service as well as giving advice.
166/
The provider had a quality team who carried out audits in the service as well as giving advice.
166/
There were specialist teams such as fire safety and positive behaviour support.
However, although the systems and tools were comprehensive, they had not identified and addressed some of the safety concerns that we found at this inspection.
[Comprehensively rubbish then]
167/
However, although the systems and tools were comprehensive, they had not identified and addressed some of the safety concerns that we found at this inspection.
[Comprehensively rubbish then]
167/
[This is where I feel for smaller providers. All these big boys get to copy and paste their forms, audits, systems, and still can't deliver basic safe care.
The fact they have specialist teams is neither here nor there if they aint doing their jobs and producing results]
168/
The fact they have specialist teams is neither here nor there if they aint doing their jobs and producing results]
168/
This was a breach of Regulation 17 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
The provider was working on promoting good cultures and empowering teams in services to take responsibility for the culture of the service.
This had not yet been implemented in this service but there were plans to do so.
[Future performance, always, one day]
170/
This had not yet been implemented in this service but there were plans to do so.
[Future performance, always, one day]
170/
There was one house where records indicated the culture might not have been as person centred as in other houses.
We discussed this with managers who told us they were going to take steps to assess and improve culture of the service with support of provider's quality team
171/
We discussed this with managers who told us they were going to take steps to assess and improve culture of the service with support of provider's quality team
171/
[The self proclaimed leading voice of learning disability really shouldn't need the CQC to come in and inspect, and highlight poor culture, before the 'quality team' get zoomed in.
So underwhelming. So much charitable cash. So many risks to lives]
172/
So underwhelming. So much charitable cash. So many risks to lives]
172/
Provider understood duty of candour. There was an open culture and they listened to feedback and informed ppl when something went wrong, apologised and explained what the service intended to do about it.
Despite this we were concerned in 2 houses ppl's families may not...
173/
Despite this we were concerned in 2 houses ppl's families may not...
173/
...have been informed of issues that could affect their relative's safety or wellbeing.
[How can @CareQualityComm write this as consecutive bullets in same report. It's completely incongruous.
Open culture ≠ families not being told stuff
Three breaches. Myth bust that]
174/
[How can @CareQualityComm write this as consecutive bullets in same report. It's completely incongruous.
Open culture ≠ families not being told stuff
Three breaches. Myth bust that]
174/

Next @OutreachSupport 86 Meade Hill Road, Manchester
A residential care home that provides care and accommodation for up to five people with a learning disability, or with autism.
Requirements improvement across the board
api.cqc.org.uk/public/v1/repo…
175/
A residential care home that provides care and accommodation for up to five people with a learning disability, or with autism.
Requirements improvement across the board
api.cqc.org.uk/public/v1/repo…
175/

A large, adapted, detached house within its own grounds. People living there have their own bedrooms, and home also has communal living areas, including a living room, dining room and kitchen.
People's needs were not always met because of staffing levels within the service
176/
People's needs were not always met because of staffing levels within the service
176/
The service had basic paper-based care records. There were some assessments of risk, but these needed to be reviewed and updated to reflect people's increasing dependencies.
177/
177/
Care plans required reviewing and updating so they provided staff with true picture of ppl's current needs and wishes.
Were quality and assurance systems in place to monitor safety and quality of care provided. However, further work and more regular audits were required
178/
Were quality and assurance systems in place to monitor safety and quality of care provided. However, further work and more regular audits were required
178/
We found the service was not able to demonstrate how they were meeting the underpinning principles of right support, right care and right culture.
The service did not support people to have maximum choice, control and independence.
179/
The service did not support people to have maximum choice, control and independence.
179/
This meant people were not able to work towards identified goals.
Staffing levels impacted on people's opportunities to go on trips out and take part in pastimes and activities both in and away from the home.
180/
Staffing levels impacted on people's opportunities to go on trips out and take part in pastimes and activities both in and away from the home.
180/
People were able to express their views, but routines existed in the service based on the availability of staff.
People did not always have opportunities to do things spontaneously.
[The option to do so has to be a fundamental facet of adult life, surely?]
181/
People did not always have opportunities to do things spontaneously.
[The option to do so has to be a fundamental facet of adult life, surely?]
181/
Actions to improve people's experiences were not taken in a timely manner.
Routines were established within the home that did not promote person-centred care.
182/
Routines were established within the home that did not promote person-centred care.
182/
People had access to independent advocates to help represent their wishes, but best interest decisions were not always formally documented.
183/
183/
People were not consistently supported to have maximum choice and control of their lives and staff did not always support them in the least restrictive way possible and in their best interests; the policies and systems in the service did not support this practice.
184/
184/
Access to the outside garden space was not always safe for people due to their increased frailty. Following a discussion with residential service manager they contacted the landlord to make accessing the garden easier so that ppl remained safe.
[Last inspection 3yrs ago]
185/
[Last inspection 3yrs ago]
185/
Due to the model of care and staffing levels in the service, there were not always enough staff on duty for people to take part in activities and visits how and when they wanted.
[Half lives, safe'ish but bored]
186/
[Half lives, safe'ish but bored]
186/
Written guidance about the use of homely remedies needed to be individualised further. More detail was needed about how people expressed the need for treatment of minor ailments.
[No idea what a homely remedy is, like my Gran saying to put Vicks on the soles of your feet?]
187/
[No idea what a homely remedy is, like my Gran saying to put Vicks on the soles of your feet?]
187/
People's needs had been assessed. Care plan updates occurred but a full review of people's needs was required, given their increasing ages and dependencies.
[How does it take a @CareQualityComm inspector to point this out?]
188/
[How does it take a @CareQualityComm inspector to point this out?]
188/
Goals and aspirations had been identified for people. However, these had not been reviewed or revisited for some time to check they remained valid or achievable.
[5yrs ago I wanted to get fit, now I've given up, imagine if you were held to new years resolutions for 5yrs]
189/
[5yrs ago I wanted to get fit, now I've given up, imagine if you were held to new years resolutions for 5yrs]
189/
Hospital passports had been developed... Some details needed to be updated to reflect changes in people's needs.
[Initiatives like hospital passports are good intentioned, but IMO can be both othering and dangerous - no use at all, give false reassurance, if not accurate]
190/
[Initiatives like hospital passports are good intentioned, but IMO can be both othering and dangerous - no use at all, give false reassurance, if not accurate]
190/
People had lived at the home for a number of years. Their needs had changed and more needed to be done to help people to access the rear garden safely.
[How, honestly, how could this have been missed; so sad after a pandemic where ppl revelled in their gardens too]
191/
[How, honestly, how could this have been missed; so sad after a pandemic where ppl revelled in their gardens too]
191/
When ppl needed to make an important decision, and there was doubt about their capacity to do so, there was a lack of evidence the decision had been made in their best interests.
One person had relinquished their mobility car... reasons... were not formally documented.
192/
One person had relinquished their mobility car... reasons... were not formally documented.
192/
Whilst people were able to express their views, routines existed in the service based on the availability of staff.
Care plans contained information across a wide range of areas but required updating.
Photographs of the people living in the home also needed updating.
193/
Care plans contained information across a wide range of areas but required updating.
Photographs of the people living in the home also needed updating.
193/
People's needs had changed but they had not been consulted whether original goals and aspirations were still current.
People were not able to make choices about what they did and when. They did not have the freedom to go out when they wanted.
194/
People were not able to make choices about what they did and when. They did not have the freedom to go out when they wanted.
194/
People had nominated days for individual staff support.
One person was looking forward to attending the leisure club, run by the provider and held at head office. They were told on the day this was cancelled.
[Wonder if they'd be charged to attend, like in review last wk]
195/
One person was looking forward to attending the leisure club, run by the provider and held at head office. They were told on the day this was cancelled.
[Wonder if they'd be charged to attend, like in review last wk]
195/
The provider had no contingency plans in place in the absence of a key member of staff.
The person was obviously disappointed at the cancellation and told us so.
196/
The person was obviously disappointed at the cancellation and told us so.
196/
More needed to be done to ensure that people were adequately supported to take part in their chosen social and leisure interests on a regular basis.
Resources to enable people to leave the service had not been made more readily available.
197/
Resources to enable people to leave the service had not been made more readily available.
197/
This was a breach of Regulation 9 (Person-centred care) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
198/
198/
Communication plans were in place but needed reviewing and updating.
One plan indicated that when a person collected their jacket and pulled staff to the door this meant they wanted to go for a drive.
However, the person no longer had access to a car.
199/
One plan indicated that when a person collected their jacket and pulled staff to the door this meant they wanted to go for a drive.
However, the person no longer had access to a car.
199/
Whilst audits had been completed the regularity of these checks were not in line with company policy.
All the concerns we found on inspection... were not identified through the provider's own quality monitoring systems.
[Performative scrutiny, be seen to do it, no more]
200/
All the concerns we found on inspection... were not identified through the provider's own quality monitoring systems.
[Performative scrutiny, be seen to do it, no more]
200/
The provider shared a range of policies with us that were out of date, most having been last reviewed in February 2018.
[Over 4 years ago]
201/
[Over 4 years ago]
201/
The last on-site visit undertaken by the provider had been carried out in June 2018.
There was no clear plan in place to drive forward improvements at the service.
[4 long, stale, stagnating lives. Such apathy]
202/
There was no clear plan in place to drive forward improvements at the service.
[4 long, stale, stagnating lives. Such apathy]
202/
The registered manager was also responsible for two other services.
This meant their time at this service was limited.
We were not assured the registered manager, or the provider, had clear oversight and governance of the service.
203/
This meant their time at this service was limited.
We were not assured the registered manager, or the provider, had clear oversight and governance of the service.
203/
This was a breach of Regulation 17 (Good governance) of the Health and Social Care Act 2008
Staff felt supported in their role but felt that staffing levels could be improved.
204/
Staff felt supported in their role but felt that staffing levels could be improved.
204/
Audits carried out by registered manager identified where improvements were needed.
However, these audits had not identified the gaps and inaccuracies in care plans, and need for regular review of records. There was little evidence of continuous learning in the service.
205/
However, these audits had not identified the gaps and inaccuracies in care plans, and need for regular review of records. There was little evidence of continuous learning in the service.
205/
There was no evidence that the provider kept up to date with national policy and guidance, such as closed cultures guidance.
[Two breaches @OutreachSupport. A report. A plan. While people stagnate]
206/
[Two breaches @OutreachSupport. A report. A plan. While people stagnate]
206/

Sorry twitter, I feel quite queasy there is so much of this non-care and support to get thru.
Next up Your Life Care Group Supported Living Service in Sheerness
A supported living service providing personal care to one person at the time of the inspection
[One person]
207/
Next up Your Life Care Group Supported Living Service in Sheerness
A supported living service providing personal care to one person at the time of the inspection
[One person]
207/

Governance processes were not always effective in monitoring the quality of care. Some of people's key records with regards to their health and safety were not up to date.
None of the providers policies had been reviewed since 2020.
208/
None of the providers policies had been reviewed since 2020.
208/
There had not been a registered manager at the service for 19 months.
The service was being managed jointly by a part-time manager and the provider.
[They're not even pretending to care. How can you not have a registered manager for over 1.5yrs with no consequence?]
209/
The service was being managed jointly by a part-time manager and the provider.
[They're not even pretending to care. How can you not have a registered manager for over 1.5yrs with no consequence?]
209/
The service was not able to demonstrate how they were meeting some of the underpinning principles of Right support, right care, right culture.
Staff had not supported people to make decisions following best practice in decision-making.
210/
Staff had not supported people to make decisions following best practice in decision-making.
210/
Decision making processes did not include key information about how people had been involved in making decisions. People's goals and aspirations were understood by staff, but these had yet to be recorded so progress towards them could be monitored.
211/
211/
People's wishes, needs and rights were not always put at the heart of the service as the provider had situated their main office in people's homes.
The model of supported living is that people's rather than the provider's concerns come first.
[If only]
212/
The model of supported living is that people's rather than the provider's concerns come first.
[If only]
212/
This service was registered with us on 20 December 2019 and this is the first inspection.
[How can people be allowed to go so long without an inspection? How can that be safe?]
213/
[How can people be allowed to go so long without an inspection? How can that be safe?]
213/
Staff had not demonstrated best practice around assessing mental capacity, supporting decision-making and best interest decision-making.
Capacity assessments had been insufficiently completed as they gave no details as to how a specific decision had been made
214/
Capacity assessments had been insufficiently completed as they gave no details as to how a specific decision had been made
214/
We recommend the provider seeks advice and guidance from a reputable source around assessing and recording people's mental capacity.
215/
215/
People's health actions plans and hospital passports did not contain up to date information about ppl's health, as they had not been reviewed since 2019.
Provider's assessment process did not follow best practice guidance such as REACH standards and The Real Tenancy Test
216/
Provider's assessment process did not follow best practice guidance such as REACH standards and The Real Tenancy Test
216/
People's assessments were not available to look at the inspection as the nominated individual could not locate them.
However, care plans reflected a good understanding of people's needs, including relevant assessments of people's communication support.
217/
However, care plans reflected a good understanding of people's needs, including relevant assessments of people's communication support.
217/
People's privacy and dignity was upheld when being supported with their care.
However, the practice of citing the provider's main 'office' in peoples' home did not follow best practice
218/
However, the practice of citing the provider's main 'office' in peoples' home did not follow best practice
218/
This 'office' contained the providers equipment and staff files, including staff files of staff who worked at another of the provider's services.
[On what planet is this acceptable, standards or not. Imagine if your window cleaner moved their office into your home]
219/
[On what planet is this acceptable, standards or not. Imagine if your window cleaner moved their office into your home]
219/
Service management and leadership was inconsistent. Leaders and the culture they created did not always support the delivery of high-quality, person-centred care.
The provider has failed to register a manager at the service in line with their condition of registration.
220/
The provider has failed to register a manager at the service in line with their condition of registration.
220/
Service was registered on 20 Dec 2019, with a registered manager in post. This manager left on 12 October 2020. There had not been a manager, who was registered with us since this time. This is a period of 19 months. We are dealing with this outside the inspection process.
221/
221/
Service was managed jointly by part-time manager and the provider.
There had been a lack of consistency in how well the service was managed.
Governance processes and quality monitoring were not always effective in identifying service shortfalls and areas for improvement
222/
There had been a lack of consistency in how well the service was managed.
Governance processes and quality monitoring were not always effective in identifying service shortfalls and areas for improvement
222/
The provider information return submitted before the inspection visit gave minimal information about the running of the service and did not identify any planned improvements.
[Yet since notified of inspection, all this training is planned, odd really]
223/
[Yet since notified of inspection, all this training is planned, odd really]
223/
Weekly audits had identified that people's health and social care documentation were all up-to-date.
However, people's hospital passport and fire evacuation plan had not been reviewed since September 2019 and October 2020 respectively.
224/
However, people's hospital passport and fire evacuation plan had not been reviewed since September 2019 and October 2020 respectively.
224/
There was a potential risk this information was not-up-to date due to people's changing needs.
All the providers' policies and procedures were dated 2020.
They had not been reviewed and updated to reflect policy and legislation changes [or a global pandemic]
225/
All the providers' policies and procedures were dated 2020.
They had not been reviewed and updated to reflect policy and legislation changes [or a global pandemic]
225/
Although staff understood people's goals and aspirations, these had not been recorded so progress towards them could be monitored.
226/
226/
There were not effective systems to assess, monitor and improve the quality and safety of the service.
Nor to keep up to date records in respect of each service user and the management of the regulated activity of personal care.
This was a breach of regulation 17
227/
Nor to keep up to date records in respect of each service user and the management of the regulated activity of personal care.
This was a breach of regulation 17
227/
Provider had not always kept up-to-date with national guidance to inform improvements to the service.
However, the management team understood the aims of supported living to promote and encourage people's independence and choices.
[Except the office in someone's home?]
228/
However, the management team understood the aims of supported living to promote and encourage people's independence and choices.
[Except the office in someone's home?]
228/
The vision and values of the service focused on matching staff to people who used the service, and this had been well managed.
[One breach, a report, a plan]
229/
[One breach, a report, a plan]
229/

Local one now, Kazlum Support in Crediton.
A supported living service providing personal care to 12 people at the time of the inspection. It provides personal care to people living in their own houses and flats, and in a 'supported living' setting
api.cqc.org.uk/public/v1/repo…
230/
A supported living service providing personal care to 12 people at the time of the inspection. It provides personal care to people living in their own houses and flats, and in a 'supported living' setting
api.cqc.org.uk/public/v1/repo…
230/

Staff supported people to make choices about their daily lives and engage in activities, however, staff were not always supporting people in the least restrictive way possible and in their best interests.
231/
231/
This meant the care and support model did not always maximise people's choice, control and independence.
People were supported by enough staff who knew them well, and staff communicated with people in ways that met their needs.
232/
People were supported by enough staff who knew them well, and staff communicated with people in ways that met their needs.
232/
People's risk assessments were clear and up to date, however, people's support plans did not always contain enough information to enable staff to support them in a person-centred way.
233/
233/
Staff understood how to protect people from poor care and abuse but did not always recognise where their practice might be abusive or restrict people's rights.
234/
234/
People's positive behaviour support plans did not always contain sufficient detailed information which led to staff sometimes working with people in inconsistent ways.
The Provider, Registered Manager and manager were not alert to the culture of the service
235/
The Provider, Registered Manager and manager were not alert to the culture of the service
235/
The culture did not ensure staff truly valued and promoted people's individuality, protected their rights and enabled them to develop and flourish.
Management were defensive of practice which we highlighted as poor and outdated.
236/
Management were defensive of practice which we highlighted as poor and outdated.
236/
Written records indicated a culture which lacked respect for ppl and indicated staff felt they knew what was best for the person and imposed that upon them.
Concerns had been raised in advance of our inspection about a potential closed culture within management of service
237/
Concerns had been raised in advance of our inspection about a potential closed culture within management of service
237/
Most staff told us they felt managers were open and approachable, however, some comments did indicate some elements of a closed culture.
238/
238/
The failure to meet the underpinning principles of Right support, right care, right culture, meant we could not be assured that people who used the service were able to live as full a life as possible and achieve the best possible outcomes.
239/
239/
Systems were not operated effectively to identify where people may have experienced abuse or been put at risk of harm, and it not been identified that some people had been subject to degrading treatment.
240/
240/
People were subject to daily restrictions such as limited use of technology, restrictions on what they could spend their money on and restrictions around food.
No mental capacity assessments had been completed in relation to these decisions.
241/
No mental capacity assessments had been completed in relation to these decisions.
241/
People's support plans referred to staff making decisions and taking action in people's best interest, however, no mental capacity assessments or best interest decisions had been completed.
242/
242/
Peoples care was not always delivered in line with standards, guidance and the law and there were no clear pathways to future goals and aspirations, including skills teaching in people's support plans.
Staff completed regular training.
[Clearly pointless training]
243/
Staff completed regular training.
[Clearly pointless training]
243/
Governance processes were ineffective and did not hold staff to account, keep people safe, protect their rights or ensure good quality care and support.
There were no audit and improvement tools in place, which impacted on people achieving good outcomes.
244/
There were no audit and improvement tools in place, which impacted on people achieving good outcomes.
244/
The service did not always act on the duty of candour appropriately.
Where the service did identify an allegation of abuse, referrals to the Local Authority safeguarding team were made and investigations carried out.
[Where they identified... and where they didn't...]
245/
Where the service did identify an allegation of abuse, referrals to the Local Authority safeguarding team were made and investigations carried out.
[Where they identified... and where they didn't...]
245/
Following our inspection, we made nine safeguarding referrals to the Local Authority that had not been identified by the service to ensure people were safely protected from harm.
[Nine. What goes on behind closed doors when inspections aren't regular. Grim]
246/
[Nine. What goes on behind closed doors when inspections aren't regular. Grim]
246/
The inspection was prompted in part due to concerns received about the management and leadership within the service and the management of allegations of abuse.
As a result, we undertook a focused inspection to review the key questions of safe, effective and well-led only.
247/
As a result, we undertook a focused inspection to review the key questions of safe, effective and well-led only.
247/
The overall rating for the service has changed from good to requires improvement. This is based on the findings at this inspection. We have found evidence that the provider needs to make improvement.
248/
248/
Systems were not operated effectively to identify where people may have experienced abuse or been put at risk of harm.
It had not been identified that some people had been subject to degrading treatment, including being admonished by staff, having 'treats' withheld and...
249/
It had not been identified that some people had been subject to degrading treatment, including being admonished by staff, having 'treats' withheld and...
249/
...being made to apologise to staff for behaviours they considered unacceptable. Treats were items people were supported to buy with their own money.
Positive behaviour systems had been used in a negative and punitive way.
[I hate PBS, and this is just one reason why]
250/
Positive behaviour systems had been used in a negative and punitive way.
[I hate PBS, and this is just one reason why]
250/
Records showed staff using 'star' rewards and the removal of treats as punishment.
Comments within incident records included, 'Lost his treat after so many times being asked to do something and due to poor listening skills.'
251/
Comments within incident records included, 'Lost his treat after so many times being asked to do something and due to poor listening skills.'
251/
'Staff member told him he would lose a star and he still continued to ignore staff.'
'Staff told him he lost a star as he had a few warnings throughout the day as well but still didn't listen.'
[This is abuse]
252/
'Staff told him he lost a star as he had a few warnings throughout the day as well but still didn't listen.'
[This is abuse]
252/
'He apologised; staff responded that his sorry doesn't mean anything unless he truly means it. Staff made him aware that he won't be receiving his treat this upcoming week.'
[So much abuse of power. Imagine the distress this person will have experienced]
253/
[So much abuse of power. Imagine the distress this person will have experienced]
253/
'I told [Name] that this is unacceptable and will lose a star. He was not happy but explained what stars are for and that he had not deserved this.'
[No words]
254/
[No words]
254/
Another person's care record said
'[Name] was told he can't behave like this as people don't like it and it's unacceptable and if it would continue, he may not be able to visit nice places like the circus.'
255/
'[Name] was told he can't behave like this as people don't like it and it's unacceptable and if it would continue, he may not be able to visit nice places like the circus.'
255/
The Provider told us this was the 'natural consequence of their behaviour.'
[I'm not really sure how any provider who holds these views is a fit and proper person to provide care and support]
256/
[I'm not really sure how any provider who holds these views is a fit and proper person to provide care and support]
256/
One person had an identified risk around food. Their support plan said they should be supervised when in the kitchen... However, records showed several occasions where they were able to access and eat food, including on one occasion from the waste bin.
257/
257/
Following our inspection, we made nine safeguarding referrals to the Local Authority to ensure people were safely protected from harm.
Systems and processes to safeguard people from the risk of abuse were not operated effectively.
This was a breach of Regulation 13
258/
Systems and processes to safeguard people from the risk of abuse were not operated effectively.
This was a breach of Regulation 13
258/
Staff supporting people in one particular house raised concerns about staffing levels, one told us
"There aren't enough staff at this house as a few have left and they haven't got any more staff for our house. Our house is the only house that needs people."
259/
"There aren't enough staff at this house as a few have left and they haven't got any more staff for our house. Our house is the only house that needs people."
259/
Another staff member reflected that the high level of needs of one of the people they support could impact upon the support other people living in the house received.
["Natural consequences" no doubt]
260/
["Natural consequences" no doubt]
260/
The effectiveness of people's care, treatment and support did not always achieve good outcomes or was inconsistent.
People's rights under the Mental Health Act were not being protected.
261/
People's rights under the Mental Health Act were not being protected.
261/
No systems in place to monitor applications to the Court of Protection... Manager was of belief that applications to deprive two people of their liberty had been made in 2017, when they had not been.
[If anyone else held someone hostage for 5yrs, there'd be consequences]
262/
[If anyone else held someone hostage for 5yrs, there'd be consequences]
262/
People were subject to daily restrictions such as limited use of technology, restrictions on what they could spend their money on and restrictions around food.
No mental capacity assessments had been completed in relation to these decisions.
263/
No mental capacity assessments had been completed in relation to these decisions.
263/
People's support plans referred to staff making decisions and taking action in people's best interest, however, no mental capacity assessments or best interest decisions had been completed.
264/
264/
Kazlum Support were managing people's finances... without legal authority to do so.
2ppl had been assessed as lacking capacity to manage their finances in 2017, no action had been taken to ensure an appropriate person was appointed to manage finances on their behalf
265/
2ppl had been assessed as lacking capacity to manage their finances in 2017, no action had been taken to ensure an appropriate person was appointed to manage finances on their behalf
265/
Training records indicated staff should complete Mental Capacity Act training every 3 years.
However, 13 out of 34 staff had not completed the training within the past three years.
[While training is so often pointless, they don't even pretend here. What consequences?]
266/
However, 13 out of 34 staff had not completed the training within the past three years.
[While training is so often pointless, they don't even pretend here. What consequences?]
266/
People's rights under the Mental Health Act were not being protected.
This was a breach of Regulation 11 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
267/
This was a breach of Regulation 11 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
267/
Peoples care was not always delivered in line with standards, guidance and the law.
There were no clear pathways to future goals and aspirations for individuals, including skills teaching, in people's support plans.
268/
There were no clear pathways to future goals and aspirations for individuals, including skills teaching, in people's support plans.
268/
There was insufficient information within people's support plans to enable staff to effectively support and understand their mental health needs.
One person had a 'star chart' system in place and their support plan said 'All staff MUST work within the same firm boundaries"
269/
One person had a 'star chart' system in place and their support plan said 'All staff MUST work within the same firm boundaries"
269/
...as if not then their behaviour will escalate to unacceptable levels which will impact on the other service users.
Being consistent with the boundaries is a must at all times.'
[You can guess how that panned out]
270/
Being consistent with the boundaries is a must at all times.'
[You can guess how that panned out]
270/
There was no guidance as to what constituted the boundaries or what was considered 'unacceptable.'
One staff member told us that different staff would implement different boundaries.
271/
One staff member told us that different staff would implement different boundaries.
271/
Care records indicated another person was not being supported to choose when they would like to get up each day, and staff used judgemental and institutionalised language.
For example, '[Name] refused to get out of bed this morning at an acceptable time.'
272/
For example, '[Name] refused to get out of bed this morning at an acceptable time.'
272/
'Refusing to get up and complete his PH routine.'
'[name] refused to get out of bed and have breakfast.'
People were not always supported to spend their day in the way they wished to.
273/
'[name] refused to get out of bed and have breakfast.'
People were not always supported to spend their day in the way they wished to.
273/
One person's support plan said they
'will often try and opt out of household chores preferring to stay in his room and listen to his music or say he is tired; however he must be encouraged and supported to carry out his share of the household tasks on a daily basis.'
274/
'will often try and opt out of household chores preferring to stay in his room and listen to his music or say he is tired; however he must be encouraged and supported to carry out his share of the household tasks on a daily basis.'
274/
Two staff members told us people's routines and activities had not been reviewed in a meaningful way, some people attended organised activities because 'that's what they've always done.'
275/
275/
Peoples care was not always delivered in line with standards, guidance and the law.
This was a breach of Regulation 9 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
276/
This was a breach of Regulation 9 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
276/
At the last inspection this key question was rated as good.
At this inspection this key question has now deteriorated to requires improvement.
This meant the service management and leadership was inconsistent.
277/
At this inspection this key question has now deteriorated to requires improvement.
This meant the service management and leadership was inconsistent.
277/
Leaders and the culture they created did not always support the delivery of high-quality, person-centred care.
Governance processes were ineffective and did not hold staff to account, keep people safe, protect their rights or ensure good quality care and support.
278/
Governance processes were ineffective and did not hold staff to account, keep people safe, protect their rights or ensure good quality care and support.
278/
There were no systems in place to audit care records, which meant managers did not analyse information to ensure people were supported in line with their support plans or identify areas for improvement.
279/
279/
Whilst the manager told us they reviewed all incident records, they had not identified themes and trends of positive behaviour systems being used in a punitive way, nor recognised this as abuse.
Were no systems in place to ensure people's rights under the MHA were upheld
280/
Were no systems in place to ensure people's rights under the MHA were upheld
280/
Registered Manager had limited involvement in day to day running of service. Did not participate in this inspection process.
They attended a feedback session, where they told us they had been unable to be actively involved in running of service due to family commitments
281/
They attended a feedback session, where they told us they had been unable to be actively involved in running of service due to family commitments
281/
[No words, honestly, contemptuous. What do they think their job is? Imagine being the registered manager, the person responsible, and not bothering to pitch up when @CareQualityComm inspectors arrive]
Notifications were not always submitted to CQC in line with regulations.
282/
Notifications were not always submitted to CQC in line with regulations.
282/
The Provider did not complete any formal quality checks.
Governance processes were ineffective.
This was a breach of Regulation 17 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
283/
Governance processes were ineffective.
This was a breach of Regulation 17 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
283/
The Provider, Registered Manager and manager were not alert to the culture of the service; the culture did not ensure staff truly valued and promoted people's individuality, protected their rights and enabled them to develop and flourish.
284/
284/
Management were defensive of poor and outdated practice, and written records indicated a culture which lacked respect for people, and indicated staff felt they knew what was best for the person and imposed that upon them.
285/
285/
Concerns had been raised in advance of our inspection about a potential closed culture within the management of the service.
Most staff told us they felt managers were open and approachable, however, some comments did indicate some elements of a closed culture.
286/
Most staff told us they felt managers were open and approachable, however, some comments did indicate some elements of a closed culture.
286/
Staff said 'It's quite a small company. I think that means there's quite a lot of family members who work together and are close friends, they're friends as well as colleagues. If you're in that circle fine, but if you're not you're an outsider.. it can be quite isolating'
287/
287/
Second Staff Member told us they had experienced some problems with their line manager.
They had tried to raise their concerns, but said they were 'friends with the manager and seem to get away with a lot'.
Third Staff Member told us 'I see all the managers as friends'
288/
They had tried to raise their concerns, but said they were 'friends with the manager and seem to get away with a lot'.
Third Staff Member told us 'I see all the managers as friends'
288/
Service did not always act on duty of candour appropriately.
Where service identified things had gone wrong, such as an allegation of abuse, they shared information appropriately with LA and people's families. However, in other instances information was not shared openly.
289/
Where service identified things had gone wrong, such as an allegation of abuse, they shared information appropriately with LA and people's families. However, in other instances information was not shared openly.
289/
A health professional told us a person they supported was served 'notice' after one allegation of abuse and had to be supported to find alternative accommodation and care.
290/
290/
They said
'They weren't forthcoming about talking to him about the move. I had to pick him up on the day and he didn't really know what was going on - even now (several) months later, he says he didn't know why he had to leave.'
[Imagine what that does to your trust]
291/
'They weren't forthcoming about talking to him about the move. I had to pick him up on the day and he didn't really know what was going on - even now (several) months later, he says he didn't know why he had to leave.'
[Imagine what that does to your trust]
291/
A second healthcare professional told us, 'There have been issues around trying to obtain information.'
The provider carried out an annual quality assurance exercise to gain feedback. We were told the most recent surveys were completed in 2021, however...
292/
The provider carried out an annual quality assurance exercise to gain feedback. We were told the most recent surveys were completed in 2021, however...
292/
...no report of findings was produced, and no action plan was developed as a result of the feedback.
[Performative scrutiny. Nothing more than ticking a box to say you've ticked it. Pure performance]
293/
[Performative scrutiny. Nothing more than ticking a box to say you've ticked it. Pure performance]
293/
[Unusually, given how many of these I've read, @CareQualityComm appeared to take action and have imposed conditions on the providers registration, although they don't say what yet.
Such a clique, sounds like an awful place to live. Not sure why it's not inadequate really]
294/
Such a clique, sounds like an awful place to live. Not sure why it's not inadequate really]
294/

10th report of the day, I feel so grubby
Oakfield Psychological Services Wellfield
A residential placement for young people aged 13-17-years with complex emotional, mental health and behavioural needs, as well as neuro-developmental disorders
api.cqc.org.uk/public/v1/repo…
295/
Oakfield Psychological Services Wellfield
A residential placement for young people aged 13-17-years with complex emotional, mental health and behavioural needs, as well as neuro-developmental disorders
api.cqc.org.uk/public/v1/repo…
295/

Provider can accommodate two young people at a time.
The provider is currently registered with @CareQualityComm as a care home, for the regulated activities of 'accommodation for persons requiring nursing or personal care' and 'treatment of disease, disorder or injury'
296/
The provider is currently registered with @CareQualityComm as a care home, for the regulated activities of 'accommodation for persons requiring nursing or personal care' and 'treatment of disease, disorder or injury'
296/
Wellfield does not provide a service for adults, a service 'wholly or mainly for children', and functions as a children's home.
As such, the regulation of accommodation and care provided by Wellfield is the responsibility of @Ofstednews as regulator for children's homes.
297/
As such, the regulation of accommodation and care provided by Wellfield is the responsibility of @Ofstednews as regulator for children's homes.
297/
At the time of our inspection there were two young people using the service.
The management and organisation of most record keeping in Wellfield was good.
[Most doing some heavy lifting there methinks]
298/
The management and organisation of most record keeping in Wellfield was good.
[Most doing some heavy lifting there methinks]
298/
Recording of medicines administration and the disposal of medicines was not always completed in line with the service's own guidance and protocol.
For example, we saw instances where only one staff member had signed to confirm administration and disposal of medicines...
299/
For example, we saw instances where only one staff member had signed to confirm administration and disposal of medicines...
299/
...limiting the assurance that young people received their prescribed medicines in a safe, and effective manner; and also not preventing the misuse of unused drugs.
Incidents were not always notified to CQC in accordance with regulatory registration.
300/
Incidents were not always notified to CQC in accordance with regulatory registration.
300/
We found an example where a member of staff had been removed for professional misconduct whilst at work and several examples where notifications were not completed in a timely manner.
[Whattttt. How do you remove someone for professional misconduct and forget notify CQC?]
301/
[Whattttt. How do you remove someone for professional misconduct and forget notify CQC?]
301/
Medicines management and reconciliation records were comprehensive and when completed, ensured enough oversight and assurance that medicines were maintained and monitored appropriately.
[When completed]
302/
[When completed]
302/
Processes were clear and understood by staff, however, adherence to these procedures was inconsistent.
We cld not be assured records for the young person in the 'Acorns' were accurate or consistently completed in accordance with service's medicine's management policy...
303/
We cld not be assured records for the young person in the 'Acorns' were accurate or consistently completed in accordance with service's medicine's management policy...
303/
...and accompanying guidance.
We saw instances where only one staff member signed to confirm administration, disposal or stock take of medicines. This had previously been highlighted by the RMN who completes regular medicines audits for the provider.
304/
We saw instances where only one staff member signed to confirm administration, disposal or stock take of medicines. This had previously been highlighted by the RMN who completes regular medicines audits for the provider.
304/
Observed one staff member dispose of medicines incorrectly, against provider's clear protocols.
Systems not been established to assess, monitor and mitigate risks to health, safety and welfare of young people and others, as provider cld not ensure staff followed policies
305/
Systems not been established to assess, monitor and mitigate risks to health, safety and welfare of young people and others, as provider cld not ensure staff followed policies
305/
This placed people at risk of harm. This was a breach of regulation 17(1) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
306/
306/
[Effective, caring and responsive were rated good, so I'm not focusing on them here, save to share this, which made my dark heart sing]
Young people were also supported to engage in activities in the community with assistance from staff.
[Wait for it...]
307/
Young people were also supported to engage in activities in the community with assistance from staff.
[Wait for it...]
307/
They were also encouraged to have pets and a kitten had recently been adopted. This brought with it responsibilities for care which the young person had embraced.
[Well-led required improvement]
308/
[Well-led required improvement]
308/
Leaders and the culture they created did not always support the delivery of high-quality, person-centred care.
There was a thorough process for accurately and comprehensively reporting incidents internally, including the provision of regular incident analysis reports
309/
There was a thorough process for accurately and comprehensively reporting incidents internally, including the provision of regular incident analysis reports
309/
Lack of clarity to support incident reporting and sharing with CQC in line with regulatory registration.
We found example where a member of staff had been removed for professional misconduct whilst at work and several where notifications was not completed in timely manner
310/
We found example where a member of staff had been removed for professional misconduct whilst at work and several where notifications was not completed in timely manner
310/
Processes had not been established to assess, monitor and mitigate the quality and safety of services provided in the carrying on of the regulated activity.
Such processes must enable registered person, in particular, to evaluate and improve their practice in respect...
311/
Such processes must enable registered person, in particular, to evaluate and improve their practice in respect...
311/
...the processing of information, namely incident reporting.
This placed people at risk of harm.
This was a breach of regulation 17(1) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
312/
This placed people at risk of harm.
This was a breach of regulation 17(1) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
312/
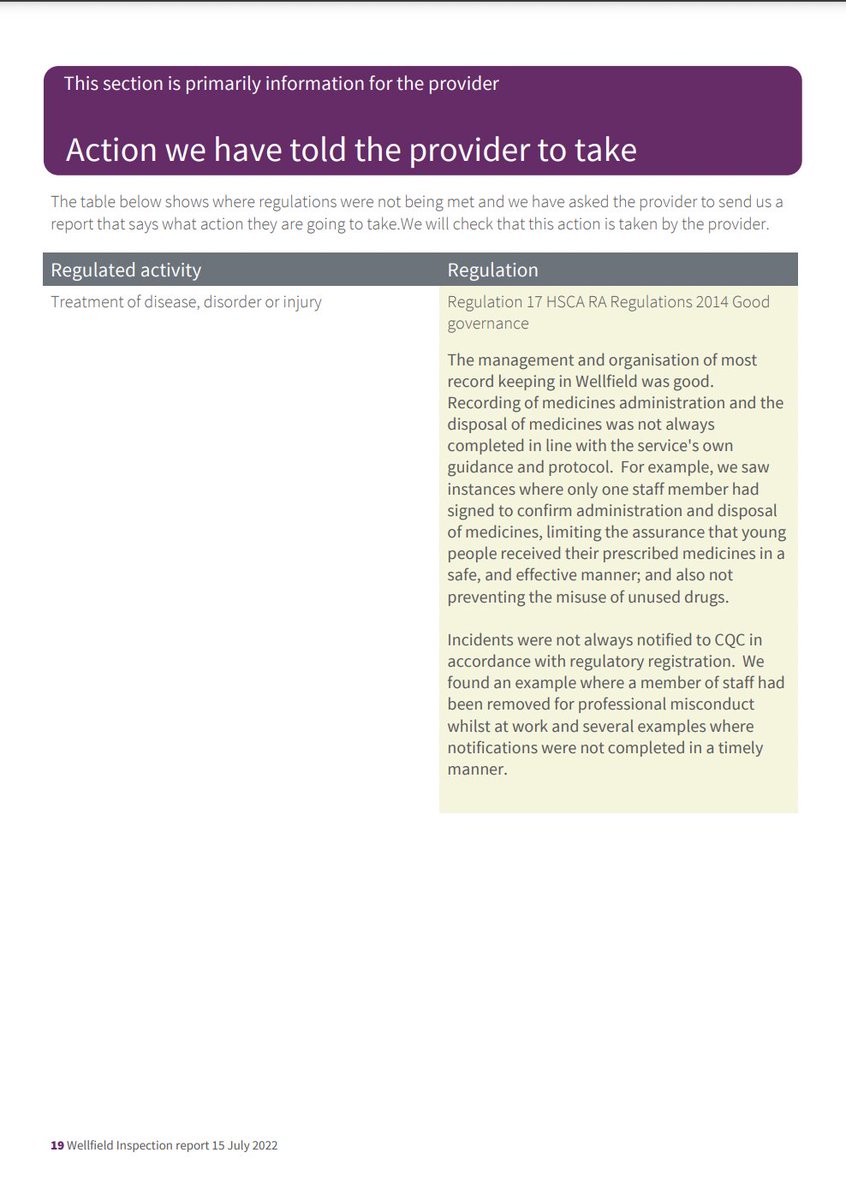
OK, am going in, will try finish requires improvement provision (this is penultimate one) and then tomorrow will do separate threads for two latest inadequate places.
Homebeech - a care home providing personal and nursing care to up to 66 people
api.cqc.org.uk/public/v1/repo…
313/
Homebeech - a care home providing personal and nursing care to up to 66 people
api.cqc.org.uk/public/v1/repo…
313/

Service provides support to younger and older adults who live with physical disabilities and/or mental health needs, some ppl were living with dementia or learning disabilities. At the time of our inspection were 55 ppl using the service.
[55 ppl with such varied needs]
314/
[55 ppl with such varied needs]
314/
[Homebeech is part of the Saffronland Homes group. Their tagline is Dignity through Respect and they claim:
"Each of our homes is unique in its offering and in all cases it is our people, staff and residents alike, who truly make the home"
Let's take a look at Homebeech]
315/
"Each of our homes is unique in its offering and in all cases it is our people, staff and residents alike, who truly make the home"
Let's take a look at Homebeech]
315/
People were not always protected from risks. COVID-19 infection prevention and control measures were not robust; visiting professionals were not always asked to provide proof their lateral flow device test results.
316/
316/
People's medicines were not always stored and disposed of safely, expiry dates of medicines were not
always checked.
People were not always treated with dignity and respect.
317/
always checked.
People were not always treated with dignity and respect.
317/
Staff did not always communicate with people before assisting them in their wheelchairs.
[How's that Dignity through Respect working out exactly?]
Some confidential information about people were accessible to others who did not require to know them.
318/
[How's that Dignity through Respect working out exactly?]
Some confidential information about people were accessible to others who did not require to know them.
318/
People did not always experience person-centred care.
For example, people's care records did not always contain person-centred techniques to help support people when they were anxious.
319/
For example, people's care records did not always contain person-centred techniques to help support people when they were anxious.
319/
Some people receiving end of life support had care plans which contained basic information which meant staff could not provide them personalised support.
The provider did not demonstrate a full understanding of regulatory requirements.
320/
The provider did not demonstrate a full understanding of regulatory requirements.
320/
[Funny isn't it how these providers apparently don't understand their regulatory requirements, but never have any difficulty understanding how to navigate commissioning services and get paid. Coincidence am sure]
321/
321/
Consideration had not been given to CQC's publication 'Right support, right care, right culture' to support people living with a learning disability.
[But it's the people who make the home]
322/
[But it's the people who make the home]
322/
Provider had not updated their registration with CQC to include providing a service to ppl living with a learning disability but subsequently did so following our inspection.
[So @CareQualityComm found out they were supporting learning disabled ppl by accident]
323/
[So @CareQualityComm found out they were supporting learning disabled ppl by accident]
323/
Quality assurance processes had not identified areas of improvement highlighted at the inspection, such as, recruitment records not being in line with CQC regulations and care records not reflecting people's current needs.
324/
324/
We received mixed feedback about the food provided.
One person told us, "The food was good but some of it I don't like, some not cooked properly but you get fish and chips"
325/
One person told us, "The food was good but some of it I don't like, some not cooked properly but you get fish and chips"
325/
The last rating for this service was requires improvement (published 28 August 2020). There were no breaches of regulation, the inspection looked at safe and well-led only and had met the breach of regulation 17 at that time.
326/
326/
The rating for the previous inspection was requires improvement (published 26 April 2019) and there were multiple breaches of regulation. The provider completed an action plan to show what they would do and by when to improve.
327/
327/
We looked at all of these breaches at this inspection.
Service has been rated requires improvement for the last six consecutive inspections.
[How on earth can anyone be allowed to require improvement for SIX consecutive inspections. Six. What must people's lives be like]
328/
Service has been rated requires improvement for the last six consecutive inspections.
[How on earth can anyone be allowed to require improvement for SIX consecutive inspections. Six. What must people's lives be like]
328/
At this inspection some improvements had been made and the provider was no longer in breach of regulations 14 and 18.
Not enough improvement had been made and the provider remained in breach of regulation 9 (Person-centred care).
[Wait for it...there's more]
329/
Not enough improvement had been made and the provider remained in breach of regulation 9 (Person-centred care).
[Wait for it...there's more]
329/
We found new breaches of regulation 10 (Dignity and respect), regulation 12 (Safe care and treatment) and regulation 17 (Good governance).
The inspection was prompted in part due to concerns received about medicines and pressure area care.
330/
The inspection was prompted in part due to concerns received about medicines and pressure area care.
330/
This meant some aspects of the service were not always safe and there was limited assurance about safety.
There was an increased risk that people could be harmed.
Medicines were not always stored and disposed of safely.
331/
There was an increased risk that people could be harmed.
Medicines were not always stored and disposed of safely.
331/
Inspection was in part prompted by concerns regarding medicines management. Where people required oxygen, the cylinders were not always safely secured to avoid the risk of them falling or rolling. This increased risk of gasses becoming unstable and cld pose as a fire hazard
332/
332/
There were some out of date medicines and dressings stored at the service.
Some medicines held in anticipation of people requiring end of life care or rescue treatments for infections were stored beyond their expiry date.
333/
Some medicines held in anticipation of people requiring end of life care or rescue treatments for infections were stored beyond their expiry date.
333/
Whilst these medicines had not been administered to people, they may be ineffective or cld be harmful if taken.
The medicines fridge records showed the fridge was safe to use. However, the fridge thermometer not been reset, and the minimum and maximum readings indicated...
334/
The medicines fridge records showed the fridge was safe to use. However, the fridge thermometer not been reset, and the minimum and maximum readings indicated...
334/
...the medicines may have been stored outside of the recommended temperature range.
Staff were unaware of when the thermometer had last been reset, without accurate readings people could not be assured their medicines would remain effective.
335/
Staff were unaware of when the thermometer had last been reset, without accurate readings people could not be assured their medicines would remain effective.
335/
We were not assured that the provider was preventing visitors from catching and spreading infections.
On both days of the inspection, members of the inspection team were not asked to show proof of their lateral flow device (LFD) tests.
336/
On both days of the inspection, members of the inspection team were not asked to show proof of their lateral flow device (LFD) tests.
336/
We were somewhat assured that the provider was promoting safety through the layout and hygiene practices of the premises.
Some high touch points such as keypad locks were visually unclean.
337/
Some high touch points such as keypad locks were visually unclean.
337/
There was a cleaning schedule in place, however, the keypads remained unclean throughout both days of our inspection.
We highlighted this to staff who cleaned the keypads.
338/
We highlighted this to staff who cleaned the keypads.
338/
We were somewhat assured that the provider was using PPE effectively and safely.
A staff member was seen to be wearing their mask under their chin when in very close proximity to a person.
[Somewhat assured]
339/
A staff member was seen to be wearing their mask under their chin when in very close proximity to a person.
[Somewhat assured]
339/
The staff member said this was to aid communication, but there was no risk assessment in place to support this.
Shortly after the inspection, the registered manager told us they had increased their spot checks on staff to ensure PPE was used appropriately.
340/
Shortly after the inspection, the registered manager told us they had increased their spot checks on staff to ensure PPE was used appropriately.
340/
The provider failed to ensure the safe management of medicines and failed to ensure appropriate infection control measures were in place in response to the COVID-19 pandemic.
This was a breach of regulation 12 (Safe care and treatment)
341/
This was a breach of regulation 12 (Safe care and treatment)
341/
People's needs were not always met by the adaptation of the service.
3 units at the service, Daffodil for younger adults with physical disabilities and mental health needs, Homebeech for older adults with physical disabilities and mental health needs and Beechside for...
342/
3 units at the service, Daffodil for younger adults with physical disabilities and mental health needs, Homebeech for older adults with physical disabilities and mental health needs and Beechside for...
342/
...people living with dementia. People living in Daffodil and Homebeech shared a communal living space which included a living and dining area, conservatory and tuck shop. People living in Beechside remained in their unit.
343/
343/
There had been limited consideration to the environment to support ppl living with dementia on the Beechside unit.
Ppl's bedrooms were not clearly identifiable with pictorial or written signage.
There were some ppl living with a learning disability residing at service.
344/
Ppl's bedrooms were not clearly identifiable with pictorial or written signage.
There were some ppl living with a learning disability residing at service.
344/
Staff supported ppl appropriately, altho they had not received training in this area.
After the inspection, the registered manager provided us with assurances that learning disability training had been arranged for staff.
345/
After the inspection, the registered manager provided us with assurances that learning disability training had been arranged for staff.
345/
People's needs were not always thoroughly assessed before to moving into the service.
People were admitted into the service swiftly and at short notice. Staff were not always made aware of people's diagnoses until after they moved into the service.
346/
People were admitted into the service swiftly and at short notice. Staff were not always made aware of people's diagnoses until after they moved into the service.
346/
A person who was new to the service could not communicate their distress or unmet need and showed emotion with their reactions.
Their preadmission assessment did not highlight this need.
347/
Their preadmission assessment did not highlight this need.
347/
We observed occasions where the person expressed emotion and staff did not know how to help them manage those situations.
This caused difficulties in their relationships with others in the home which we observed on both days of the inspection.
348/
This caused difficulties in their relationships with others in the home which we observed on both days of the inspection.
348/
The registered manager told us they were unable to meet the person's needs and they were sourcing an alternative appropriate placement for them.
349/
349/
At our last comprehensive inspection we rated this key question requires improvement. At this inspection the rating for this key question has remained requires improvement.
This meant people did not always feel well-supported, cared for or treated with dignity and respect.
350/
This meant people did not always feel well-supported, cared for or treated with dignity and respect.
350/
Last inspection, ppl were supported and treated with dignity and involved in their care, but their confidentiality was not always respected
This inspection people's confidentiality was still not always maintained and staff did not always uphold and respect people's dignity
351/
This inspection people's confidentiality was still not always maintained and staff did not always uphold and respect people's dignity
351/
We observed some undignified areas of care. For example, on two different occasions people who used wheelchairs were wheeled to different areas of the service by staff without being asked.
352/
352/
On Beechside, a staff member cleaned a person's face without communicating with the person. The person responded "What are you doing?"
Staff did not always knock on ppl's bedroom doors before entering. Whilst we were speaking with a person a staff member entered...
353/
Staff did not always knock on ppl's bedroom doors before entering. Whilst we were speaking with a person a staff member entered...
353/
...the room without requesting permission. The person told us "Sometimes staff forget to knock"
On Beechside, a person was being cared for in bed, their door was open. The person was not covered in a dignified way, people and visitors were able to see them when passing
354/
On Beechside, a person was being cared for in bed, their door was open. The person was not covered in a dignified way, people and visitors were able to see them when passing
354/
Some staff on the Beechside unit spoke with people in a childlike manner.
For example, one person did not wish to eat their lunch, and a staff member told them they would not get pudding if they did not eat more.
355/
For example, one person did not wish to eat their lunch, and a staff member told them they would not get pudding if they did not eat more.
355/
A staff member flicked a person's hair while they were assisting another person to eat.
Whilst it was meant to be a playful gesture, it was inappropriate and unclear whether this advance was welcome.
[In front of inspectors]
356/
Whilst it was meant to be a playful gesture, it was inappropriate and unclear whether this advance was welcome.
[In front of inspectors]
356/
Confidentiality was not always respected. Medication administration records (MAR) containing personal details were left on top of the medicine trolley which could be accessed by people.
357/
357/
People were not treated with dignity and respect and confidentiality was not maintained.
This is a breach of regulation 10 (Dignity and respect) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
358/
This is a breach of regulation 10 (Dignity and respect) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
358/
People's needs were not always met.
At last comprehensive inspection, provider failed to ensure staff routinely followed ppl's assessed plans of care. This was a continued breach of Regulation 9. Not enough improvement had been made at this inspection, still in breach Reg9
359/
At last comprehensive inspection, provider failed to ensure staff routinely followed ppl's assessed plans of care. This was a continued breach of Regulation 9. Not enough improvement had been made at this inspection, still in breach Reg9
359/
Where some people required support to manage expressions of emotions, their care plans did not always contain enough information for staff to support them appropriately.
360/
360/
One person's care plan documented they preferred to be addressed by their nick name.
Staff and management called them by their first name despite what was documented.
361/
Staff and management called them by their first name despite what was documented.
361/
The person's care plan directed staff to reassure them but did not detail what made them anxious and how to do so.
We observed the person to be expressing their emotions throughout the inspection and attempts of staff reassurance were not successful.
362/
We observed the person to be expressing their emotions throughout the inspection and attempts of staff reassurance were not successful.
362/
The provider had failed to ensure people received person centred care and treatment that was appropriate to their needs and reflected their personal preferences.
This is a continued breach of Regulation 9 of the Health and Social Care act (Regulated Activities)
363/
This is a continued breach of Regulation 9 of the Health and Social Care act (Regulated Activities)
363/
At our last comprehensive inspection on 11 Feb 2019, the provider's systems and processes for quality monitoring had failed to identify significant concerns.
Enforcement action was taken against the provider and conditions were placed upon the provider's registration.
364/
Enforcement action was taken against the provider and conditions were placed upon the provider's registration.
364/
We carried out focussed inspection on 5 Aug 2020, altho, the conditions on the provider's registration was not reviewed.
At this inspection we reviewed the report of actions the provider sent us each month against the action taken within the service.
365/
At this inspection we reviewed the report of actions the provider sent us each month against the action taken within the service.
365/
The conditions had been complied with; however, some areas required further improvements.
The registered manager was not always clear about regulatory requirements. They were unaware of 'Right support, right care, right culture'.
366/
The registered manager was not always clear about regulatory requirements. They were unaware of 'Right support, right care, right culture'.
366/
The service did not notify CQC of the intention to support people living with a learning disability. The provider notified CQC of a change of service user bands shortly after the inspection.
[And if the inspectors hadn't visited...]
367/
[And if the inspectors hadn't visited...]
367/
Quality assurance systems for medicines did not highlight medicine practices shortfalls.
Monthly audit noted gaps in recording, however, there were no outcomes of investigations as to whether the medicines had been administered and what potential impact this had on people
368/
Monthly audit noted gaps in recording, however, there were no outcomes of investigations as to whether the medicines had been administered and what potential impact this had on people
368/
Shortfalls identified in quality assurance processes were not always recognised.
Care plan audits did not highlight inconsistencies and lack of person-centred care in some care plans found during our inspection.
[Six inspection reports requiring improvement. Still]
369/
Care plan audits did not highlight inconsistencies and lack of person-centred care in some care plans found during our inspection.
[Six inspection reports requiring improvement. Still]
369/
Record keeping of staff recruitment was not in line with CQC's regulations.
Recruitment records were not maintained to include information relevant to staff employment and their role.
Systems had failed to identify where some recruitment records were incomplete.
370/
Recruitment records were not maintained to include information relevant to staff employment and their role.
Systems had failed to identify where some recruitment records were incomplete.
370/
Evidence of nursing and midwifery council (NMC) checks for trained nurses were not always documented.
Initial checks had been made to ensure trained staff were registered with the NMC but there was no system in place to check for annual updates.
371/
Initial checks had been made to ensure trained staff were registered with the NMC but there was no system in place to check for annual updates.
371/
The provider had failed to effectively establish and operate systems to assess, monitor and improve quality and safety of the services provided which put people at risk.
This was a breach of Regulation 17 (Good governance) of the Health and Social Care Act 2008
372/
This was a breach of Regulation 17 (Good governance) of the Health and Social Care Act 2008
372/
We received mixed feedback from people.
Comments included, "I have made suggestions over the years such as the menu. I have suggested things I wanted to eat, I like dumplings and they haven't made them for me."
[Dumplings. SO simple]
373/
Comments included, "I have made suggestions over the years such as the menu. I have suggested things I wanted to eat, I like dumplings and they haven't made them for me."
[Dumplings. SO simple]
373/
[The action provider is required take is not listed for some reason but @CareQualityComm say they'll request an action plan "to understand what they will do to improve the standards of quality and safety"
Seventh consecutive time they've required improvement.
Seventh]
374/
Seventh consecutive time they've required improvement.
Seventh]
374/
[I'm knackered, sorry, actually can't face another one of these tonight. Will start again tomorrow and hope there aren't more reports published overnight]
375/ tbc
375/ tbc
Final requires improvement @CareQualityComm report into care for learning disabled and/or autistic people for now. Then two inadequates, then we gotta hope and keep our fingers crossed CQC aren't publishing any reports today, so I can get back to other work, or just sleep🤞
376/
376/
@LArcheUK Bognor Regis Bethany, requires improvement in all domains except well-led, where it's inadequate.
L'Arche Bethany is a residential care home providing personal care to six people at the time of the inspection. The service can support up to six people.
377/
L'Arche Bethany is a residential care home providing personal care to six people at the time of the inspection. The service can support up to six people.
377/

People were not always supported to have the maximum possible independence, choice or control over their own lives.
People did not have outcome focused support plans.
Some practices restricted people's independence and choice.
378/
People did not have outcome focused support plans.
Some practices restricted people's independence and choice.
378/
People told us they were not supported to pursue their interests or achieve aspirations and goals.
One person told us this was "Annoying" because they couldn't choose what they wanted to do.
[Non-lives]
379/
One person told us this was "Annoying" because they couldn't choose what they wanted to do.
[Non-lives]
379/
People did not receive support in an environment that was well maintained, well equipped or well furnished.
Staff and visitors to the service told us the poor condition of the environment and furnishing was long standing.
380/
Staff and visitors to the service told us the poor condition of the environment and furnishing was long standing.
380/
One said "It's been like this for years, we just get used to it".
People told us they were not able to decorate their rooms or the communal areas.
[This place is meant to be home, imagine 'getting used' to yr home falling to pieces, even tho you're paying to live there]
381/
People told us they were not able to decorate their rooms or the communal areas.
[This place is meant to be home, imagine 'getting used' to yr home falling to pieces, even tho you're paying to live there]
381/
People's care and support plans did not reflect people's individual needs and aspirations.
People's care and support did not consistently focus on their quality of life or follow best practice.
[What did it focus on then?]
382/
People's care and support did not consistently focus on their quality of life or follow best practice.
[What did it focus on then?]
382/
There was a failure to assess risks people might face and people were not encouraged or enabled to take positive risks.
People were not provided with opportunities to try new activities tailored to them that enhanced and enriched their lives.
383/
People were not provided with opportunities to try new activities tailored to them that enhanced and enriched their lives.
383/
We observed that people participated in group activities facilitated by L'Arche rather than pursuing their own individual interests or seeking opportunities for volunteering or employment.
[The risk with a 'community' is a small, closed off life, sounds evident here]
384/
[The risk with a 'community' is a small, closed off life, sounds evident here]
384/
The provider had not fully considered people's needs and wishes in the planning and deployment of staff.
People were not supported to lead inclusive and empowered lives.
385/
People were not supported to lead inclusive and empowered lives.
385/
There was a failure to identify and mitigate institutionalised practices and risks associated with closed cultures.
People could not be assured of receiving support based on transparency, respect and inclusivity.
386/
People could not be assured of receiving support based on transparency, respect and inclusivity.
386/
People shared their home with staff who lived alongside them.
People told us they did not choose the staff who shared their home.
There was a strong emphasis on meeting people's spiritual needs and valuing people as members of the L'Arche community.
387/
People told us they did not choose the staff who shared their home.
There was a strong emphasis on meeting people's spiritual needs and valuing people as members of the L'Arche community.
387/
Last rating for service was good (27 Sept 2018)
We have identified breaches in relation to protecting people from avoidable harm, restrictive practices, safe care and treatment, medicines, staff skills and knowledge, person centred care and the management of the service.
388/
We have identified breaches in relation to protecting people from avoidable harm, restrictive practices, safe care and treatment, medicines, staff skills and knowledge, person centred care and the management of the service.
388/
Full information about CQC's regulatory response to the more serious concerns found during inspections is added to reports after any representations and appeals have been concluded.
[Will watch this space I guess]
389/
[Will watch this space I guess]
389/
CQC regulates both the premises and the care provided, and both were looked at during this inspection.
The service did not have a manager registered with the Care Quality Commission.
This inspection was unannounced
[How? So many providers without registered managers]
390/
The service did not have a manager registered with the Care Quality Commission.
This inspection was unannounced
[How? So many providers without registered managers]
390/
Some aspects of the service were not always safe and there was limited assurance about safety.
There was an increased risk that people could be harmed.
People were not kept safe from avoidable harm and abuse.
391/
There was an increased risk that people could be harmed.
People were not kept safe from avoidable harm and abuse.
391/
Staff were not knowledgeable about or committed about deploying techniques that promoted the reduction in restrictive practice.
We observed a person being denied their TV remote control throughout the day despite asking for it and this was causing them anxiety.
[No words]
392/
We observed a person being denied their TV remote control throughout the day despite asking for it and this was causing them anxiety.
[No words]
392/
The person told us on numerous occasions "[staff name] has it in the office".
Staff including managers, told us on several occasions and in front of the person staff were looking for the remote control as the person had lost it.
393/
Staff including managers, told us on several occasions and in front of the person staff were looking for the remote control as the person had lost it.
393/
One staff said to the person "You have lost it again haven't you".
This was found to be an incorrect and dishonest account as we later learnt that staff kept the persons remote control in the locked managers office.
[This. Is. Gaslighting.
This. Is. Abuse]
394/
This was found to be an incorrect and dishonest account as we later learnt that staff kept the persons remote control in the locked managers office.
[This. Is. Gaslighting.
This. Is. Abuse]
394/
It was found by the CQC inspector amongst prescribed medicine in the locked office along with the TV remote control for the lounge.
[Imagine the rage the person must feel. Imagine how they must question their reality. Imagine supposedly caring for people and abusing them]
395/
[Imagine the rage the person must feel. Imagine how they must question their reality. Imagine supposedly caring for people and abusing them]
395/
We addressed this with the community leader who told us the person had capacity to agree to staff holding their remote control and this was in place as a behaviour strategy.
We asked to see evidence of this agreement and the behaviour strategy.
[Defensiveness]
396/
We asked to see evidence of this agreement and the behaviour strategy.
[Defensiveness]
396/
[Not to mention separate systems designed to other people further. Perhaps @larcheuk should be concentrating on the regulatory system and requirements, like a registered manager, competency for staff, people having a say in their lives. Not their version of community]
397/
397/
[How can a place supposedly prioritising spiritual needs, infantalise, gaslight and psychologically abuse people in their community?
I'm so disappointed at this. I've often held L'Arche Manchester up as an example of good, to many raised eyebrows. Guess this is the flip]
398/
I'm so disappointed at this. I've often held L'Arche Manchester up as an example of good, to many raised eyebrows. Guess this is the flip]
398/
Community leader and manager were unable to provide this and informed us these were not in place.
The person told us they wld prefer to keep the remote control in their bedroom.
[First inspection in over 3.5yrs. What have people's lives been like. Unseen?]
399/
The person told us they wld prefer to keep the remote control in their bedroom.
[First inspection in over 3.5yrs. What have people's lives been like. Unseen?]
399/
Positive solutions to this had not been sought and the person was denied access to the remote control.
Staff had training on how to recognise and report abuse.
This had not been effective in recognising unlawful and restrictive practices as a form of abuse.
400/
Staff had training on how to recognise and report abuse.
This had not been effective in recognising unlawful and restrictive practices as a form of abuse.
400/
We spoke to the community leader who said they would take immediate action to address the concerns we had raised.
The provider's processes did not ensure the right level of scrutiny and oversight to ensure people were protected from abuse and improper treatment.
401/
The provider's processes did not ensure the right level of scrutiny and oversight to ensure people were protected from abuse and improper treatment.
401/
This was a breach of regulation 13 (safeguarding people from abuse and improper treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
402/
402/
The service failed to keep people safe by sharing of information about risks.
People did not have specific support or risk management plans for health concerns and staff knowledge about how to support people safely was inconsistent.
403/
People did not have specific support or risk management plans for health concerns and staff knowledge about how to support people safely was inconsistent.
403/
Some risks associated with medical conditions such as seizures, diabetes, allergies and food intolerances had not been considered or shared.
[Whaaaat? Are ppl meant to intuit it? How can you identify if someone is unwell if you don't know risks or signs to look out for?]
404/
[Whaaaat? Are ppl meant to intuit it? How can you identify if someone is unwell if you don't know risks or signs to look out for?]
404/
This meant people could not be assured of receiving appropriate support or that staff would recognise the signs of their health deteriorating and the action to take.
Information from medical professionals was not reflected in people's support plans.
405/
Information from medical professionals was not reflected in people's support plans.
405/
For example, specific guidance from a healthcare professional to ensure a person's safety whilst eating had not been shared.
At lunch time we observed the persons meal that was not in line with this guidance.
[Nah, I mean, choking, aspiration, they only result in death]
406/
At lunch time we observed the persons meal that was not in line with this guidance.
[Nah, I mean, choking, aspiration, they only result in death]
406/
We made the manager aware of our concerns and they took immediate action to prepare the meal in a way that was safe for the person to eat.
We observed that it was not explained to the person why their meal had been taken away from them.
[No words]
407/
We observed that it was not explained to the person why their meal had been taken away from them.
[No words]
407/
People's care records did not ensure they received the help and support they needed.
This was because staff failed to keep accurate, complete and up-to-date records.
For example, a known trigger for a person having a seizure was not reflected with their support plan.
408/
This was because staff failed to keep accurate, complete and up-to-date records.
For example, a known trigger for a person having a seizure was not reflected with their support plan.
408/
Another person's care plan did not reflect their significant respiratory condition, or the risks associated with this.
Where the hospital had recorded a drug allergy for a person their care passport recorded no known adverse reactions to medicines.
409/
Where the hospital had recorded a drug allergy for a person their care passport recorded no known adverse reactions to medicines.
409/
We spoke to staff about these risks and their knowledge was inconsistent.
This meant people could not be assured of receiving consistent and appropriate support to keep safe.
The safety of the living environment was not well managed.
410/
This meant people could not be assured of receiving consistent and appropriate support to keep safe.
The safety of the living environment was not well managed.
410/
The first day of our inspection was unannounced and, on our arrival, the front door was wide open and remained open throughout the day.
We were told by ppl and staff this was usual practice. The house was on a busy road with a constant flow of passing cars and pedestrians.
411/
We were told by ppl and staff this was usual practice. The house was on a busy road with a constant flow of passing cars and pedestrians.
411/
Consideration had not been given to the risks associated with intruders or the safety of staff and people or their possessions.
We observed damaged flooring on the stairs and in the kitchen that was a potential trip hazard.
412/
We observed damaged flooring on the stairs and in the kitchen that was a potential trip hazard.
412/
New stair carpet had been ordered altho hole in current one had not been made safe.
We spoke with the manager, community leader and housing coordinator about our concerns and were provided with assurances areas wld be addressed and made safe.
[So many ppl. So much apathy]
413/
We spoke with the manager, community leader and housing coordinator about our concerns and were provided with assurances areas wld be addressed and made safe.
[So many ppl. So much apathy]
413/
People could not be assured that accidents and incidents would be investigated appropriately.
Processes for manager oversight of accidents and incidents was not effective.
414/
Processes for manager oversight of accidents and incidents was not effective.
414/
Since March 2022 there had been six incident and accidents reported by staff.
None of these had the managers part completed or signed and there was no evidence of manager oversight, investigation or trends analysis.
415/
None of these had the managers part completed or signed and there was no evidence of manager oversight, investigation or trends analysis.
415/
For example, one person had recently fallen towards the bottom of the stairs.
Staff had recorded the cause of the fall as tiredness.
At inspection there was a hole in the stairs carpet and the person told us this was the area they had fallen.
[No words]
416/
Staff had recorded the cause of the fall as tiredness.
At inspection there was a hole in the stairs carpet and the person told us this was the area they had fallen.
[No words]
416/
The lack of management oversight and investigation meant we could not be assured that all potential causes of the fall had been considered such as a seizure or environmental factors.
The provider had failed to do all that is reasonably practicable to mitigate risks.
417/
The provider had failed to do all that is reasonably practicable to mitigate risks.
417/
Care and treatment were not provided in a safe way.
Risks to the health and safety and wellbeing of people had not been assessed.
This was a breach of regulation 12 (Safe care and treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
418/
Risks to the health and safety and wellbeing of people had not been assessed.
This was a breach of regulation 12 (Safe care and treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
418/
We spoke with the community leader about the lack of accurate and up to date information in people's care plans and the absence of risk management plans.
They provided assurances that all care records would be reviewed over the next six weeks...
419/
They provided assurances that all care records would be reviewed over the next six weeks...
419/
... to ensure they reflected up to date and person-centred information.
Where there were known risks, risk management plans would be implemented as a priority.
[Maybe someone local cld just pop round and check, I mean the door will always be open]
420/
Where there were known risks, risk management plans would be implemented as a priority.
[Maybe someone local cld just pop round and check, I mean the door will always be open]
420/
Staff raised concerns and recorded incidents and near misses and this helped keep ppl safe.
As a direct result of staff reporting improvements had been made to the way the service operates and the care people receive.
For example, staff had received additional training
421/
As a direct result of staff reporting improvements had been made to the way the service operates and the care people receive.
For example, staff had received additional training
421/
... to address some concerns about medicine errors and handover between shift changes was introduced to improve communication.
[But not to trip hazards, or psychological abuse when it comes to your remote - those weren't recognised, therefore not reported]
422/
[But not to trip hazards, or psychological abuse when it comes to your remote - those weren't recognised, therefore not reported]
422/
People were not supported by staff who followed safe medicine systems and processes.
We were not assured the processes in place to dispose of waste medicines were robust.
Medicines held in the medicine's fridge were several months out of date.
423/
We were not assured the processes in place to dispose of waste medicines were robust.
Medicines held in the medicine's fridge were several months out of date.
423/
It is acknowledged these medicines were no longer being administered to people however staff and managers were unaware these were out of date until we showed them.
We identified an extremely large quantity of medicines for disposal in a locked hall cupboard.
[What?]
424/
We identified an extremely large quantity of medicines for disposal in a locked hall cupboard.
[What?]
424/
[It's so odd isn't it. The relaxed approach to large quantities of medicine, just lock them in the hall.
Why not just take them to Boots?
When my lovely ma died, it was one of the first things me and my sis did. I hated knowing there were all these drugs in her home]
425/
Why not just take them to Boots?
When my lovely ma died, it was one of the first things me and my sis did. I hated knowing there were all these drugs in her home]
425/
These dated back to 2021 and were not logged. This left them open to potential misappropriation.
The manager and community leader told us they were not aware of these medicines but would ensure action was taken to dispose of them appropriately.
[Why weren't they aware?]
426/
The manager and community leader told us they were not aware of these medicines but would ensure action was taken to dispose of them appropriately.
[Why weren't they aware?]
426/
Staff did not ensure effective processes to assess and provide the support people needed to take their medicines safely.
For example, we observed a person in the dining room was administered a very large tablet after their breakfast.
427/
For example, we observed a person in the dining room was administered a very large tablet after their breakfast.
427/
This was prescribed three times every day after food. The person was struggling to swallow it and began coughing.
Staff said "Oh, is it stuck again?". Another said, "He always does that it's normal".
The person coughed for several minutes and was very red in the face.
428/
Staff said "Oh, is it stuck again?". Another said, "He always does that it's normal".
The person coughed for several minutes and was very red in the face.
428/
The person said, "This always happens" and described the tablet as, "Difficult to take", "Nasty", and "Tasted awful".
Consideration had not been given to exploring if the medicine was available in another form.
[Non-care]
429/
Consideration had not been given to exploring if the medicine was available in another form.
[Non-care]
429/
Person told us that if they cld have the medicine in a way that was easier it wld be "better, yes please".
Manager provided assurances the GP surgery wld be contacted about prescribing instructions for the tablet or having it in another form.
[Inspector induced action]
430/
Manager provided assurances the GP surgery wld be contacted about prescribing instructions for the tablet or having it in another form.
[Inspector induced action]
430/
People could not be assured of a person-centred approach to medicines management.
We observed medicines being administered openly in communal areas and in front of others.
431/
We observed medicines being administered openly in communal areas and in front of others.
431/
There had been a failure to consider the risk of increased seizure activity for a person whose medicines to manage their epilepsy were being reduced.
432/
432/
Protocols were not in place for people who required medicines to be administered 'as and when required'(PRN) such as pain relief or laxatives.
There were no clear guidelines as to when these should be considered and administered.
433/
There were no clear guidelines as to when these should be considered and administered.
433/
People told us staff would know if they needed medicines. One person said, "They know when I'm not feeling well". Another said, "I can ask for tablets".
[Something I guess]
434/
[Something I guess]
434/
The provider had failed to ensure the safe and proper management of medicines.
This was a breach of regulation 12 (Safe care and treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
435/
This was a breach of regulation 12 (Safe care and treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
435/
Staff who administered medicines were fully trained and had undertaken competency assessments.
Medicine administration records (MAR) were completed accurately.
436/
Medicine administration records (MAR) were completed accurately.
436/
Where appropriate the positive behaviour support (PBS) team also provided support. PBS is a person-centred approach to supporting a person with a learning disability.
[Hmmm. It's also how people end up being abused and gaslit when all they want is the TV remote]
437/
[Hmmm. It's also how people end up being abused and gaslit when all they want is the TV remote]
437/
The service did not always use effective infection, prevention and control measures to keep people safe.
This was because some areas of the environment and furnishings were hard to sanitise effectively due to their poor condition or state of repair.
438/
This was because some areas of the environment and furnishings were hard to sanitise effectively due to their poor condition or state of repair.
438/
The service did not prompt safety through the layout of the premises.
Due to the poor condition of the environment and some furnishings safety not ways implemented effectively.
We made the manager aware of our concerns.
439/
Due to the poor condition of the environment and some furnishings safety not ways implemented effectively.
We made the manager aware of our concerns.
439/
Staff and people consistently told us staffing was a barrier to being able to undertake person centred activities.
People told us they were not able to undertake activities they enjoyed such as swimming.
[Imagine living by the sea, but not going swimming]
440/
People told us they were not able to undertake activities they enjoyed such as swimming.
[Imagine living by the sea, but not going swimming]
440/
Staff told us there were not enough staff to drive the minibus and this prevented them from going further than places they could walk to as a group.
We observed staffing was not always deployed to take account of people's activity needs or preferences.
441/
We observed staffing was not always deployed to take account of people's activity needs or preferences.
441/
This included where people had additional 1-1 funding for staff.
For example, where the local authority funded a person to have an additional 1-1 support for two mornings a week, staff told us, and the rota evidenced that staffing was not increased to provide this.
442/
For example, where the local authority funded a person to have an additional 1-1 support for two mornings a week, staff told us, and the rota evidenced that staffing was not increased to provide this.
442/
At inspection the person's 4hrs of 1-1 time was provided from the existing staffing allocation and the person walked to a group activity with everyone else in the house.
At the activity the person stood by the front door until staff suggested a walk which they accepted.
443/
At the activity the person stood by the front door until staff suggested a walk which they accepted.
443/
On return to the house all staff were involved in preparing lunch.
We observed the person was not provided with any support or encouragement to prepare their own meal.
The service covered gaps on the rota with agency staff and safe staffing levels were maintained.
444/
We observed the person was not provided with any support or encouragement to prepare their own meal.
The service covered gaps on the rota with agency staff and safe staffing levels were maintained.
444/
The service was actively recruiting staff and people were involved in the interview process.
People shared their home with some 'live-in' staff. These staff were mainly recruited from overseas and lived alongside people sharing communal facilities as well as...
445/
People shared their home with some 'live-in' staff. These staff were mainly recruited from overseas and lived alongside people sharing communal facilities as well as...
445/
...mealtimes, activities and spiritual reflection.
This was in line with the L'Arche ethos of sharing lives and valuing diversity.
[Lofty ethos ambitions, huge gap with reality. Is it a shared life? If you don't get the support you need, don't get to make choices]
446/
This was in line with the L'Arche ethos of sharing lives and valuing diversity.
[Lofty ethos ambitions, huge gap with reality. Is it a shared life? If you don't get the support you need, don't get to make choices]
446/
We asked people if they were involved in choosing these staff and how they felt about them living in their home.
People told us they were not involved in the interview and did not have any choice about who shared their home.
447/
People told us they were not involved in the interview and did not have any choice about who shared their home.
447/
The effectiveness of people's care, treatment and support did not always achieve good outcomes or was inconsistent.
People who were new to the service could not be assured that their needs and choices had been effectively communicated and planned for.
448/
People who were new to the service could not be assured that their needs and choices had been effectively communicated and planned for.
448/
For example, important information about a person's very specific health and behaviour support needs related to food had not been included within their support plan.
449/
449/
Person was observed having periods of high anxiety and frustration during inspection and received inconsistent responses from staff.
Guidance had not been provided to staff to enable them to understand persons genetic condition and how this impacted on their daily life.
450/
Guidance had not been provided to staff to enable them to understand persons genetic condition and how this impacted on their daily life.
450/
There was a lack of information to reflect how person wanted to be supported to maintain their own wellbeing.
Support plans and assessments were not robustly reviewed to ensure they contained accurate and up to date information.
451/
Support plans and assessments were not robustly reviewed to ensure they contained accurate and up to date information.
451/
A person who had diabetes did not have this reflected within their support plan which recorded they were 'able to eat anything'.
We observed the person having a carbohydrate rich meal of rice and they had two slices of staff birthday cake.
[At least there is cake]
452/
We observed the person having a carbohydrate rich meal of rice and they had two slices of staff birthday cake.
[At least there is cake]
452/
Following their meal the person was given prescribed medicine to manage their diabetes.
People with epilepsy did not have support or risk management plans in place.
453/
People with epilepsy did not have support or risk management plans in place.
453/
It is acknowledged that people's seizures were rare however, some staff were unable to describe people's individual support needs or how their seizures presented.
[Rare they might be but it only takes one to die from. How is epilepsy non-care so apathetic in social care?]
454/
[Rare they might be but it only takes one to die from. How is epilepsy non-care so apathetic in social care?]
454/
This meant people could not be assured of receiving safe, consistent and appropriate support to manage their health and well-being.
People were not provided with opportunities to be involved in planning, shopping and cooking their own meals in their preferred way.
455/
People were not provided with opportunities to be involved in planning, shopping and cooking their own meals in their preferred way.
455/
Ppl told us staff planned and cooked their meals for them. One person told us they liked macaroni cheese but said this was never on the menu.
A person told us they had helped to make a staff birthday cake but apart from that they were not encouraged to help in the kitchen
456/
A person told us they had helped to make a staff birthday cake but apart from that they were not encouraged to help in the kitchen
456/
We observed breakfast and lunch being prepared for people without their involvement. Teaching plans were not in place to support people to develop skills in preparing or cooking their own meals and snacks. We observed people being supported to make drinks.
457/
457/
One person's support plan said they liked to help with the supermarket shopping, and this was supported by a picture of a shopping trolley full of food.
During the inspection we observed the weekly shop being put away by staff.
458/
During the inspection we observed the weekly shop being put away by staff.
458/
We asked the person if they had been shopping and they said "No".
Staff told us the shopping was ordered online and delivered.
One staff said "It's easier and safer this way and we wouldn't have the staff or transport to go to the shop"
[Non-lives centred around staff]
459/
Staff told us the shopping was ordered online and delivered.
One staff said "It's easier and safer this way and we wouldn't have the staff or transport to go to the shop"
[Non-lives centred around staff]
459/
[Doesn't explain why person wasn't even involved in putting shopping away.
Too many learning disabled people have these small glimpses of things that make a life.
They get to go shopping, they decide they like shopping, but even that is taken away for ease of staff]
460/
Too many learning disabled people have these small glimpses of things that make a life.
They get to go shopping, they decide they like shopping, but even that is taken away for ease of staff]
460/
Consideration had not been given to seeking a solution that enabled the person to participate in food shopping shop at the supermarket which is something they enjoyed.
461/
461/
People told us they were unsure if they had been involved in reviewing their support plans.
Relatives told us they were not involved in the planning and reviewing of their loved one's care.
[Such a paternalistic model]
462/
Relatives told us they were not involved in the planning and reviewing of their loved one's care.
[Such a paternalistic model]
462/
Where care plans had been reviewed this was evidenced by the date being crossed out and a new date added.
There was no evidence of people's outcomes, achievements or new aspirations being reflected or planned for.
[No words]
463/
There was no evidence of people's outcomes, achievements or new aspirations being reflected or planned for.
[No words]
463/
The provider had failed to ensure people received person centred care that that was appropriate to their needs and reflected their personal preferences.
This is a breach of Regulation 9 (Person-centred care) of the Health and Social Care Act 2008
464/
This is a breach of Regulation 9 (Person-centred care) of the Health and Social Care Act 2008
464/
People were not supported by staff who had received relevant training to meet their bespoke needs.
Some people had very specific medical and genetic conditions that impacted on their day to day life including the way they behaved and the support they required.
465/
Some people had very specific medical and genetic conditions that impacted on their day to day life including the way they behaved and the support they required.
465/
Their [staff] knowledge was limited and inconsistent. Staff had not been provided with skills, knowledge or training to meet ppl's specific needs.
This meant people could not be assured of receiving care and support to help them achieve the best quality of life
466/
This meant people could not be assured of receiving care and support to help them achieve the best quality of life
466/
The provider had an induction programme for staff to prepare them for their role.
We were provided with the most up to date record of staff induction and training dated May 2022. This showed that four staff inductions were overdue for completion.
467/
We were provided with the most up to date record of staff induction and training dated May 2022. This showed that four staff inductions were overdue for completion.
467/
Of these, two were overdue by more than 12 months.
The provider was addressing this and where staff mandatory training was not up to date.
Staff received inconsistent support. Formal supervision and appraisal were not provided in line with the providers policy.
468/
The provider was addressing this and where staff mandatory training was not up to date.
Staff received inconsistent support. Formal supervision and appraisal were not provided in line with the providers policy.
468/
Staff... had not received supervision in a long while due to absence of a manager.
Told us they had received occasional informal support from the deputy manager in the form of a general wellbeing check rather than supervision and were able to speak to the community leader
469/
Told us they had received occasional informal support from the deputy manager in the form of a general wellbeing check rather than supervision and were able to speak to the community leader
469/
The provider had failed to ensure staff providing care or treatment had appropriate support, training supervision and appraisal as is necessary to enable them to carry out the duties they are employed to perform.
This was a breach of regulation 18 (Staffing)
470/
This was a breach of regulation 18 (Staffing)
470/
Staff knowledge of how to apply the principles of the MCA was limited.
We observed the fridge door was locked when we arrived and there were locked food cupboards.
Staff gave us various reasons for the restrictions that were in place including...
471/
We observed the fridge door was locked when we arrived and there were locked food cupboards.
Staff gave us various reasons for the restrictions that were in place including...
471/
...for people's health and well-being, budget and to maintain food hygiene.
None of the staff we spoke with considered these practices to be restrictive and had not considered these practices with regards to MCA.
472/
None of the staff we spoke with considered these practices to be restrictive and had not considered these practices with regards to MCA.
472/
Staff failed to demonstrate best practice around supporting decision-making and best interest decision-making.
One person had a DoLS in place.
473/
One person had a DoLS in place.
473/
Where restrictions impacted this person such as access to food and equipment the service were unable to evidence a best interest's decision had been undertaken.
[They couldn't 'find' the TV remote, what odds a best interests decision was recorded?]
474/
[They couldn't 'find' the TV remote, what odds a best interests decision was recorded?]
474/
Where people had capacity to make their own decisions, we were unable to see any documentation that evidenced restrictions in place had been discussed or agreed with them.
475/
475/
People told us they were not consulted about restrictions and accepted these as a condition of living in the service.
One person said, "Staff look after the food". Another said "Well, I suppose that how it is really".
[I suppose that is how it is really. Again and again]
476/
One person said, "Staff look after the food". Another said "Well, I suppose that how it is really".
[I suppose that is how it is really. Again and again]
476/
People told us they could ask staff for food and they had access to yoghurts in a small fridge.
The provider had failed to identify discrimination against service users on grounds of protected characteristics (as defined in the Equality Act 2010).
477/
The provider had failed to identify discrimination against service users on grounds of protected characteristics (as defined in the Equality Act 2010).
477/
This included failure to identify an act intended to control and restrain which is not proportionate.
This was a breach of regulation 13 (safeguarding people from abuse and improper treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
478/
This was a breach of regulation 13 (safeguarding people from abuse and improper treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
478/
People and their relatives told us they did not like the condition of the house.
It was described as 'not homely' and 'poorly maintained'.
People were not supported in a safe, well equipped or well-furnished environment.
479/
It was described as 'not homely' and 'poorly maintained'.
People were not supported in a safe, well equipped or well-furnished environment.
479/
People were not included in decisions relating to the interior decoration and design of their home.
People told us they were not able to decorate their rooms and we observed people's bedrooms to be dull and contained old furniture and fittings.
480/
People told us they were not able to decorate their rooms and we observed people's bedrooms to be dull and contained old furniture and fittings.
480/
A person told us they were not allowed to have their room decorated but if they were, they would like it painted yellow and blue.
Staff told us this was because painting was the responsibility of the landlord.
[So many excuses for non-lives]
481/
Staff told us this was because painting was the responsibility of the landlord.
[So many excuses for non-lives]
481/
Furniture, furnishing and appliances within the house were old and tired.
The environment did not reflect the ages, personalities and personal interests of the people living there.
People told us they liked the location of the house which was in a residential area.
482/
The environment did not reflect the ages, personalities and personal interests of the people living there.
People told us they liked the location of the house which was in a residential area.
482/
One people told us they liked to sit on the bench by the front door and watch the cars, another told us they liked to visit the L'Arche service next door
[Of course, another 'service' next door... no doubt also for ease of staff and 'community']
483/
[Of course, another 'service' next door... no doubt also for ease of staff and 'community']
483/
Staff were caring towards people but sometimes this inhibited ppl's independence and ability to be involved in decisions about how they wanted to live their lives and positive risk taking.
A person who was very independent told us they were restricted from going out alone
484/
A person who was very independent told us they were restricted from going out alone
484/
Staff told us this was because the person might have a seizure.
We did not see any documentation that evidenced this had been discussed or agreed with the person or a DoLS applied for.
Records showed the person's last seizure was 2019.
485/
We did not see any documentation that evidenced this had been discussed or agreed with the person or a DoLS applied for.
Records showed the person's last seizure was 2019.
485/
[No doubt these are the 'rare seizures' that staff weren't able to describe how they'd support earlier in this thread... so you can't go out and live a life because you might have a seizure, but in the house staff can't recognise a seizure.
Truly mind boggling. Non-life]
486/
Truly mind boggling. Non-life]
486/
Guidance to keep them safe not reviewed since 2018 and advised the person had to be where staff could see them.
Consideration had not been given to reviewing this with the person to ensure it was current and reflected the person's views and wishes
[4yrs, no review]
487/
Consideration had not been given to reviewing this with the person to ensure it was current and reflected the person's views and wishes
[4yrs, no review]
487/
People were not involved in managing risks to themselves and in taking decisions about how to keep safe.
One person had a significant medical condition that impacted on their daily life. Self-help guidance provided by a health care professional in July 2021 to support...
488/
One person had a significant medical condition that impacted on their daily life. Self-help guidance provided by a health care professional in July 2021 to support...
488/
...person manage their condition had not been shared with them or staff, was not reflected with their care plan.
Person told us "No, I don't know about that".
Person had been denied the opportunity to have some control over way their condition impacted their daily life.
489/
Person told us "No, I don't know about that".
Person had been denied the opportunity to have some control over way their condition impacted their daily life.
489/
People, and those important to them, did not take part in making decisions and planning of their care and risk assessments.
Relatives told us they were not involved in the planning and reviewing of their loved one's support.
490/
Relatives told us they were not involved in the planning and reviewing of their loved one's support.
490/
One said, "We used to be involved but that's not happened for a few years now".
The provider had failed to ensure people were enabled and supported to participate in making decisions about their care.
491/
The provider had failed to ensure people were enabled and supported to participate in making decisions about their care.
491/
There was a lack of collaboration with relevant people to design care and treatment that ensured people's preferences and needs were met.
This is a breach of Regulation 9 (Person-centred care) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
492/
This is a breach of Regulation 9 (Person-centred care) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
492/
People did not have the opportunity to try new experiences, develop new skills or gain independence.
Support plans recorded people's aspirations however there was a lack of evidence to demonstrate how people were supported to achieve these.
493/
Support plans recorded people's aspirations however there was a lack of evidence to demonstrate how people were supported to achieve these.
493/
It is acknowledged during global pandemic there were long periods of time where govt restrictions were in place.
People told us this time had been boring.
We were unable to see evidence people had used this time at home to learn new skills or develop their independence
494/
People told us this time had been boring.
We were unable to see evidence people had used this time at home to learn new skills or develop their independence
494/
Staff knew when ppl needed their space and privacy and respected this.
We observed a person whose anxiety had begun to rise towards the end of a music session at the L'Arche Hub in Bognor Regis.
Person was able to explain to staff how they were feeling and needed space.
495/
We observed a person whose anxiety had begun to rise towards the end of a music session at the L'Arche Hub in Bognor Regis.
Person was able to explain to staff how they were feeling and needed space.
495/
Staff respect this and person was able to walk home at a slight distance from the rest of the group.
Halfway home the person said, "I'm alright now". Staff responded positively and the person began to engage in conversation for the rest of the way home.
[L'Arche Hub...]
496/
Halfway home the person said, "I'm alright now". Staff responded positively and the person began to engage in conversation for the rest of the way home.
[L'Arche Hub...]
496/
Staff members showed warmth and respect when interacting with people. We observed people receiving kind and compassionate care from staff who used positive, respectful language which people understood and responded well to.
497/
497/
People's needs were not always met.
People were not always enabled to make choices for themselves.
One person told us they would like to go out in the evening but were not allowed because dinner was at 6pm.
498/
People were not always enabled to make choices for themselves.
One person told us they would like to go out in the evening but were not allowed because dinner was at 6pm.
498/
Staff told us the evening meal was important time together as a community and staffing prevented evening activities.
A review of people's daily activities showed they did not go out of an evening.
[Ohhhh my. Non-lives in daytime hours only. Community over individuality]
499/
A review of people's daily activities showed they did not go out of an evening.
[Ohhhh my. Non-lives in daytime hours only. Community over individuality]
499/
People told us that they had to go to bed by 10pm and staff confirmed this was encouraged to support people's well-being.
We found these practices to be restrictive and institutionalised and spoke to the manager and community leader about this.
[They need @StayUpLateUK]
500/
We found these practices to be restrictive and institutionalised and spoke to the manager and community leader about this.
[They need @StayUpLateUK]
500/
Staff did not routinely seek leisure activities or widening of social circles for people.
People's care records prior to the pandemic failed to evidence people had been provided a real opportunity to seek paid or voluntary employment or social activities in local area.
501/
People's care records prior to the pandemic failed to evidence people had been provided a real opportunity to seek paid or voluntary employment or social activities in local area.
501/
People had tended to go to the L'Arche workshop/day service located in the back garden.
Person told us the day service was not reopening and said they missed this as they had enjoyed the woodworking jobs and helping.
[A day service. In the garden. Institution by stealth]
502/
Person told us the day service was not reopening and said they missed this as they had enjoyed the woodworking jobs and helping.
[A day service. In the garden. Institution by stealth]
502/
Staff had not sought to find similar clubs within the local community such as the local men's shed group.
This would provide the person with the opportunity to meet new people whilst participating in woodworking projects.
[No. Not in the actual local community]
503/
This would provide the person with the opportunity to meet new people whilst participating in woodworking projects.
[No. Not in the actual local community]
503/
People were not supported to participate in their chosen social and leisure interests on a regular basis.
People consistently told us they were bored and wanted to go out and do more. One said, "I don't do very much".
504/
People consistently told us they were bored and wanted to go out and do more. One said, "I don't do very much".
504/
A person told us they wanted to go to church rather than watching it online.
Another person wanted to consider joining a gym or the library.
A person's support plan said they were good at swimming and enjoyed this and another person had an interest in horseracing.
505/
Another person wanted to consider joining a gym or the library.
A person's support plan said they were good at swimming and enjoyed this and another person had an interest in horseracing.
505/
A relative told us they would like their loved one to visit the family home. These opportunities had not been explored.
Rotas did not provide evidence of person-centred staffing.
[Surely such a closed environment is dangerous. One inspection in 3.5yrs]
506/
Rotas did not provide evidence of person-centred staffing.
[Surely such a closed environment is dangerous. One inspection in 3.5yrs]
506/
People and staff consistently told us there were
not enough staff to do activities or to drive the minibus. The community leader told us this was due to insufficient funding for staffing and volunteers were being sought to help with this.
[Non-lives. A gazillion excuses]
507/
not enough staff to do activities or to drive the minibus. The community leader told us this was due to insufficient funding for staffing and volunteers were being sought to help with this.
[Non-lives. A gazillion excuses]
507/
People, staff and managers told us L'Arche were still restricting people's social activities as precaution to COVID 19....
Family member told us they believed the service were currently using COVID19 restrictions as an excuse not to do more with their loved one.
508/
Family member told us they believed the service were currently using COVID19 restrictions as an excuse not to do more with their loved one.
508/
Community leader informed us L'Arche were beginning to ease restrictions and were arranging a BBQ over Jubilee weekend.
This wld be an opportunity for all L'Arche services in Bognor Regis to get together.
[Oh my. Where's dividing line between cult and community?]
509/
This wld be an opportunity for all L'Arche services in Bognor Regis to get together.
[Oh my. Where's dividing line between cult and community?]
509/
[I'm no monarchist, had zero interest in celebrating Jubilee, but it can't be denied that for many people it presented an opportunity to mix with their neighbours, and local community.
Why are people living in L'Arche houses restricted to mixing with each other. In 2022]
510/
Why are people living in L'Arche houses restricted to mixing with each other. In 2022]
510/
The provider had failed to ensure people received person centred care that was appropriate to their needs and reflected their personal preferences and interests.
This is a breach of Regulation 9 (Person-centred care)
511/
This is a breach of Regulation 9 (Person-centred care)
511/
Well-Led. We looked for evidence that service leadership, management and governance assured high-quality, person-centred care; supported learning and innovation; and promoted an open, fair culture.
512/
512/
At the last inspection this key question was rated as requires improvement.
At this inspection this key question has deteriorated to inadequate.
This meant there were widespread and significant shortfalls in service leadership.
513/
At this inspection this key question has deteriorated to inadequate.
This meant there were widespread and significant shortfalls in service leadership.
513/
Leaders and the culture they created did not assure the delivery of high-quality care.
Provider's processes for quality assurance and audit were not robustly applied.
Providers quality assurance checks had failed to identify some of the concerns we found at inspection
514/
Provider's processes for quality assurance and audit were not robustly applied.
Providers quality assurance checks had failed to identify some of the concerns we found at inspection
514/
Medicine audits were not undertaken, and this had led to the failure to identify out of date medicines or that processes for correct disposal of medicines were nor being followed in line with national best practice guidance.
515/
515/
There was not a structured approach to monitoring the quality of care plans. This had led to a failure to identify care plans did not always contain enough information and guidance to ensure safe care and support.
516/
516/
The failure to ensure care records and information relating to people's care were contemporaneous meant records could not be relied upon as an accurate record of people's care.
517/
517/
Processes were not robust to protect people from harm. Systems were not in place to identify that some risks to people's health and wellbeing had not been assessed or documented.
518/
518/
For example, quality monitoring had failed to identify the failure to implement a choking risk management plan for a person with a known choking risk.
[I think we can stop #LEDER now. We know the risks to life of choking. We know many care providers disregard the risk]
519/
[I think we can stop #LEDER now. We know the risks to life of choking. We know many care providers disregard the risk]
519/
There was a failure to ensure that all reasonably practicable actions were considered and taken to mitigate risks to people. This meant the provider could not be assured people were safe.
520/
520/
Provider had not ensured a robust process for assessing staff learning, areas for development or if further additional training or support was required.
There was a failure to ensure staff followed best practice guidance...when supporting people with learning disabilities
521/
There was a failure to ensure staff followed best practice guidance...when supporting people with learning disabilities
521/
Some aspects of the care provided reflected institutionalise practices and there were restrictive practices unsupported by best interest's decision.
People were not always provided with the opportunity to be involved in their care and support.
522/
People were not always provided with the opportunity to be involved in their care and support.
522/
This meant the provider could not be assured that staff knowledge and practice were current or that learning, reflective practice and service improvement were adopted.
523/
523/
The provider had failed to establish systems and processes to assess and improve the quality and safety of the service provided or to assess and monitor risks.
This is a breach of Regulation 17 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
524/
This is a breach of Regulation 17 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
524/
We received mixed feedback about communication.
Some relatives told us communication from the service could be improved upon.
Feedback included "I wish they would make the contact instead of relying on us to ask about things".
525/
Some relatives told us communication from the service could be improved upon.
Feedback included "I wish they would make the contact instead of relying on us to ask about things".
525/
And "Sometimes we find out things by chance, they could do better in this area".
When concerns had been raised relatives felt these had been investigated appropriately
526/
When concerns had been raised relatives felt these had been investigated appropriately
526/
[No record of actions taken, presumably because @larcheuk are making representations...]
Full information about CQC's regulatory response to the more serious concerns found during inspections is added to reports after any representations and appeals have been concluded.
527/
Full information about CQC's regulatory response to the more serious concerns found during inspections is added to reports after any representations and appeals have been concluded.
527/
That's last of 12 @CareQualityComm reports into the care and support of learning disabled and/or autistic people that they rated as requiring improvement. All published in the last few days.
There are two inadequates which I'll give threads in their own rights, shortly.
/END
There are two inadequates which I'll give threads in their own rights, shortly.
/END
• • •
Missing some Tweet in this thread? You can try to
force a refresh







