Morning everyone. Here’s a challenge to start the day. Can you figure out what MCS this patient is receiving by looking at these pipes?? 

You can see the 4 cannulae in this X-ray. The RVAD drainage is from the RA and returns to the PA. The LVAD drains LV apex and returns to ascending aorta. You’ll also notice the lungs look ok and the patient isn’t intubated….. so why the oxygenator in the RVAD…….? 

This patient has a dilated cardiomyopathy and deteriorated despite inotropes so needed to be rescued with VA ECMO. Notice the stylet is pulled back during the insertion of the venous drainage cannula, there are markings on the stylet to enable this…. Did you know??
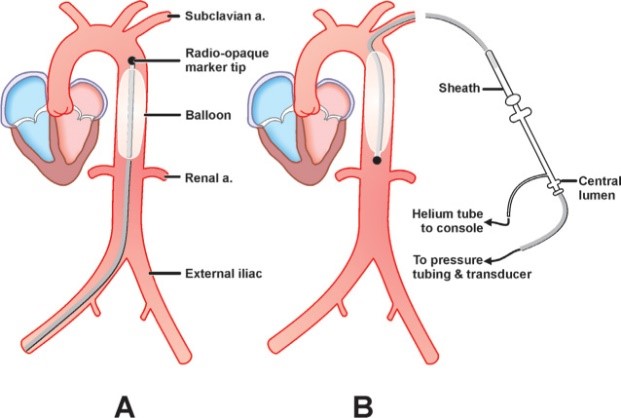
The LVEDP was measured at 40 so we also inserted a #impella and the patient made stabilised with #ecpella therapy. He went into theatre for his bivad well resuscitated and with good end organ function. Despite this he had ICU acquired weekness and so was not able to be extubated
Adding the oxygenator to the RVAD enabled us to remove CO2 and so effectively decrease his work of breathing to a level he could manage. This meant he was able to avoid a tracheotomy and so eat, drink and talk immediately. The oxygenator enabled us to effectively #humanise him.
Here is how a bivad levitronix looks without an oxygenator. Here you can see 2 blue and 2 red pipes, this time with the pumps in shot. The cannulation is identical. Notice how the LVAD chatters with the cardiac cycle.
https://twitter.com/suzehutch/status/1550463460038909953?s=21here’s Suze’s (one of our physios) amazing tweet showing our team’s rehabilitation techniques for patients on these devices.
https://twitter.com/SuzeHutch/status/1550463460038909953
• • •
Missing some Tweet in this thread? You can try to
force a refresh