
100% detection and quantification of SARS-CoV-2 with PBM-HALE, in 1 minute of exhaled breath, requires forced expiration and gives Ct's as low as 25.8. We have updated our preprint with the interim data from our Brazil study 1/n 
https://twitter.com/PulmoBioMed/status/1567094485275889666
https://twitter.com/DocMoschos/status/1530565917599481857
We had tried to detect COVID-19 in exhaled tidal breath. That's resting breathing to you and me. It didn't work (n=42). We concluded that at least PBM-HALE does what it says on the tin; no environmental contamination, as we sampled in COVID-19 wards with no ventilation. 2/n
However, others were reporting virus in breath samples- most notably @Don_Milton & @drkristenkc - that rose with increasing vocalisation. There is logic to that, as we know this increases aerosol generation. So we went off to Brazil and partnered with Mauro M Texeira at UFMG 3/n
Mauro runs clinical studies in a suburban primary care centre that serves favelas. This is the view from the site where we carried out the study 4/n 





This is the actual testing site. Two modified containers, one for participant interviews and recruitment, one for sample collection. Note the natural ventilation (pic 2, taken from door of RHS container) in the room. 5/n 



The only one container with air conditioning is the third container (not shown) where pharmaceuticals are kept for various clinical trials. The local power grid cannot take one more A/C unit. I suppose the next level of point of need testing would be in the jungle 6/n.
Like our previous study, we recruited patients positive by lateral flow test (aka rapid antigen test), who were within their first 5 days of symptoms. First they gave a tidal breath 30 min sample. Then they sang "happy birthday" in Portuguese into PBM-HALE for 15 min. 7/n
Unlike @magiorkinis's lab, the Brazilian Dx lab extracted the entire breath sample ~3.6 mL (~120 uL/min), not just 0.2mL or 1mL, to maximise sensitivity, into 30 uL, and loaded 2 uL into the RT-PCR reaction. They also used the US CDC multiplex assay for N1, N2, and RNase P. 8/n
Because there is no RNase P in exhaled tidal breath from the deep lung (there is in saliva), they tested also for 18S rRNA. They used 2 uL of the 30 uL extract, i.e. 6.67% of the sample- or 1 minute's worth of breath sample equivalent. 9/n
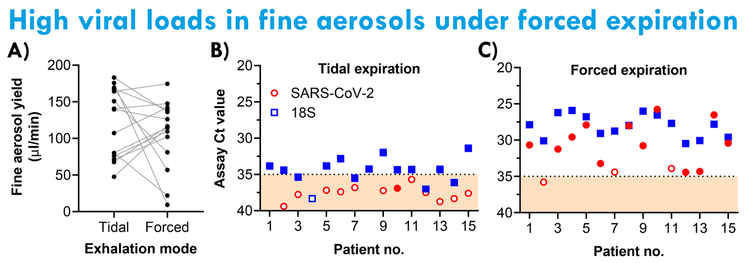
As you can see here, there is hardly any virus (none in 3/15 patients) when the patients exhale tidally. Empty data points signify less than 3 of 3 technical replicates being positive for N1 or N2 (i.e. Poisson distribution, non-quantifiable but detectable levels of virus) 10/n 

By forced expiration though (i.e. singing) we see Ct's up to 25.8 for SARS-CoV-2, which correlate (p=0.0213) with the 18S values in the sample. In other words, sing into PBM-HALE for 1 min, and we can tell you if you are shedding COVID-19 virus genomes. 11/n
We did not include culture in this study; new samples (n=30) will attempt this, but for some any Ct<32 is considered infectious. Food for thought regarding N95 face masks e.g. @trishgreenhalgh because these are fine aerosols from the deep lung, not just total exhaled breath. 12/n
The clue is in the sampling rate with tidal vs forced expiration. No significant difference in fine aerosol volume captured- because as we've shown PBM-HALE condenses when exhalation has stopped (i.e. during inhalation; eg in pic of 5 sec breath cycle). 13/n 

All controls in the Dx lab for extraction, plate positives and negatives, etc. behaved as expected. The beige band Ct 35-40 in the viral load fig is the limit of detection to limit of quantification band for the assay btw. 14/n
In my humble opinion, this is the first direct evidence that fine aerosols from the deep lung, as they exit the mouth, captured without upper airway and large droplet contamination, can contain infectious levels of SARS-CoV-2. I say this cautiously because: 15/n
many other studies that @jljcolorado @linseymarr @kprather88 @CathNoakes are familiar with have shown airborne virus, but most, if not every single one, involve pumps, droplet size evolution conditions, etc. Ours explicitly does not allow this to happen. 16/n
And before you mention 0.2 um filters- when wetted, molecules (such as genomes) will go through these filters and nebulise on the other side to contaminate the filtrate. They stop microorganisms, but not their components. 17/n
Happy to be corrected in public if wrong btw- as I've publicly done so for not checking the (faulty) temperature probe measuring -100oC for dry ice in our studies. We've also updated the pre-print for better legibility in places 18/n medrxiv.org/content/10.110…
If you spot any other errors, or have any other methodological or otherwise criticisms to offer, constructively, we welcome them. For me, open science pivots on full pre-print based data sharing and open discussion of what has been done right and what has been done wrong. 19/n
One criticism we received on submission of the previous version of the MS to a top 3 clinical respiratory journal was "the study was not registered". Since this is not an interventional study, our understanding is that no registration is required- we've asked the registers. 20/n
We have presented these data at the @EuroRespSoc #ERS2022 poster #4515 - though the Brazil results have not made the abstract. A copy of the poster will be placed online at @PulmoBioMed's website after the conference. The company will be announcing more important news soon. 21/n
• • •
Missing some Tweet in this thread? You can try to
force a refresh



