Presented today as late-breaking data at #HFSA2022 and posted online @CircAHA, new data from PROVE-HF regarding impact of #sacubitril/valsartan on #mitralregurgitation in #HFrEF.
Thanks to @DukeHFDoc for presenting in my absence.
What did we find? A 🧵...
Thanks to @DukeHFDoc for presenting in my absence.
What did we find? A 🧵...

It is well-known that MR severity is an important determinant of symptoms and prognosis in those with HFrEF.
Thanks to work from @LindenfeldJoann and @GreggWStone in the COAPT trial, it is also known that repair of MR may improve outcome in HFrEF.
Thanks to work from @LindenfeldJoann and @GreggWStone in the COAPT trial, it is also known that repair of MR may improve outcome in HFrEF.
Based on the COAPT and MITRA-FR results, current recommendations are to "optimize" #GDMT prior to decisions on repair of MR. Why?
Thanks to the reverse remodeling effects of #GDMT, MR severity may be reduced, avoiding need for MV repair.
What is known about sac/val and MR?
Thanks to the reverse remodeling effects of #GDMT, MR severity may be reduced, avoiding need for MV repair.
What is known about sac/val and MR?
In the PRIME trial, Kang and colleagues noted that sac/val improved MR more than valsartan in 118 study participants over a 12 month period.
They noted that "ARNI might be considered...optimal medical therapy of patients with heart HF and functional MR."
ahajournals.org/doi/full/10.11…
They noted that "ARNI might be considered...optimal medical therapy of patients with heart HF and functional MR."
ahajournals.org/doi/full/10.11…
In PROVE-HF we demonstrated significant reverse cardiac remodeling associated with sac/val therapy during a 12 m treatment period, however the impact on MR remained uncertain.
We therefore sought to examine association between rx with sac/val and changes in MR severity.
We therefore sought to examine association between rx with sac/val and changes in MR severity.

Following enrollment, sac/val was initiated and titrated to maximally-tolerated doses.
An echo was performed at baseline, 6 m, and 12 m and read in a core lab in a temporally-blinded fashion.
MR severity was graded consistent with ASE guidelines from 0-4+.
An echo was performed at baseline, 6 m, and 12 m and read in a core lab in a temporally-blinded fashion.
MR severity was graded consistent with ASE guidelines from 0-4+.

After excluded those missing interpretable MR data or those with prior MV procedures, the baseline data are shown attached.
This was a typical HFrEF population, mean age of 65 years, Class II predominant. About 50% had non-ischemic HFrEF.
76% were taking ACE/ARB at baseline.
This was a typical HFrEF population, mean age of 65 years, Class II predominant. About 50% had non-ischemic HFrEF.
76% were taking ACE/ARB at baseline.

The baseline echo data are attached. The median LVEF was 28%, and study participants had significant LA and LV remodeling, along with prevalent diastolic dysfunction.
At baseline 14.9% had 3-4+ MR ("eligible for MV clipping").
At baseline 14.9% had 3-4+ MR ("eligible for MV clipping").

The Sankey diagram depicts association between sac/val treatment and change in MR over a 12 m period. Note the shift toward lesser severe MR.
From baseline to 6 m, prevalence of 3-4+ MR decreased by 45%.
This improvement remained consistent at 12 m (44.7%).
From baseline to 6 m, prevalence of 3-4+ MR decreased by 45%.
This improvement remained consistent at 12 m (44.7%).

We then examined those with 3-4+ MR at baseline to see if one could predict who would "respond" with improved MR versus those who would not.
Why?
Some have suggested that those with MR due to organic valve disease (vs remodeling) might be identifiable early on.
Why?
Some have suggested that those with MR due to organic valve disease (vs remodeling) might be identifiable early on.
The bottom line is that whether examining either clinical variables or baseline echo variables, it was impossible to identify those with proportionate (due to LV remodeling) and disproportionate (due to valve dx) MR. 

Those decreasing MR from 3-4+ had ⬇️NT-proBNP concentrations by 12 months and they had greater improvement in LV remodeling. Lastly, the KCCQ-23 of responders was more significantly improved.
So they had better prognosis, improved LV function and felt better. Win/Win/Win.
So they had better prognosis, improved LV function and felt better. Win/Win/Win.

PROVE HF was a single arm, observational study, so improvement in MR might have been due to other factors.
Nonetheless, the results of this study are consistent with smaller studies and provide insights into change in MR following initiation of Sac/Val in usual care.
Nonetheless, the results of this study are consistent with smaller studies and provide insights into change in MR following initiation of Sac/Val in usual care.

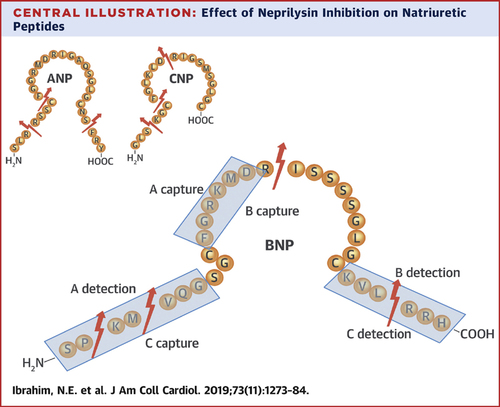
We conclude that among study participants with HFrEF, treatmement with sac/val was associated with a substantial reduction in 3-4+ MR.
This MR reduction was associated with greater reduction in NT-proBNP, improved health status and considerable reverse cardiac remodeling.
This MR reduction was associated with greater reduction in NT-proBNP, improved health status and considerable reverse cardiac remodeling.
Furthermore, baseline clinical and echocardiographic characteristics of those with 3-4+ MR who had a reduction to ≤2+ MR by 12 months were similar to those who did not.
Thus, predicting presence of MR due to LV dz versus intrinsic valve dz without GDMT optimization is difficult
Thus, predicting presence of MR due to LV dz versus intrinsic valve dz without GDMT optimization is difficult

Make no mistake about it, clipping the MV in someone with symptomatic HFrEF optimized on GDMT but with 3-4+ MR is an important consideration. This procedure has doubled in frequency since COAPT.
These results extend the definition of "optimized" GDMT prior to MV procedures.
These results extend the definition of "optimized" GDMT prior to MV procedures.

Prior to proceeding with a MV procedure, our data suggest that "optimized" GDMT should include a treatment course of sacubitril/valsartan.
#GDMTworks
#GDMTworks
It is important to recognize the exceptionally hard work of Dr. Alaa Omar and @Jcontreras75 from @MountSinaiHeart, whose Herculean efforts helped make this analysis possible.
These results are now available online at Circulation: ahajournals.org/doi/10.1161/CI…
These results are now available online at Circulation: ahajournals.org/doi/10.1161/CI…

@SeanMurphyMBBCh @JavedButler1 @DukeHFDoc @RxPDX @scottdsolomon @MGHHeartHealth @hvanspall @gcfmd @jteerlinkmd @MarkDrazner @coconnormd @mfiuzat
• • •
Missing some Tweet in this thread? You can try to
force a refresh