
1/🧵 Congratulations to @IIHDrBirmingham @MarkHeadache @DrMollan for their publication. Thanks @aswinchari for flagging this up as a #MorningPaper. #IIH #CSF @neuro_at_ic @e1v1m1 @markhwilson @AhmedToma13 @PaedNeurosurg @Samuel_Jeffery
link.springer.com/article/10.100…
link.springer.com/article/10.100…
2/ This 9-year prospective observational study included 490 #IIH patients in @uhbtrust with 98% being female (F:M was 53:1) with mean BMI 38, as defined by papilloedema (Frisen grade >0) in at least one eye. 67.1% required multiple hospital visits. 87% were treated medically.
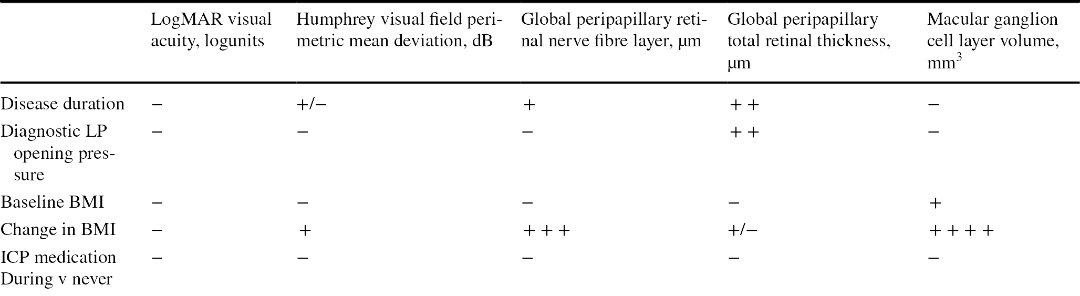
3/ Medical treatment most commonly used included acetazolamide (27%) and topiramate (9%). #IIH relapse occured in only 3.7%. Ocular outcome mirrored reduction in ganglion cell layer (GCL) vol, perimetric mean deviation (PMD) and retinal nerve fibre layet (RNFL) on OCT. 

4/ No correlation was identified between presence of papilloedema (or the reduction in the various OCT measurements) on initial presentation vs long-term visual outcome. Of all medical treatment, ⬇️BMI had the strongest link with improvement in #IIH parameters and symptoms. 
5/ Although medical treatment improved the visual parameters, no effect was seen on the headache assessment (i.e. frequency and severity).
On a separate note, those require surgery tend to have worse outcome (worse starting point?).
On a separate note, those require surgery tend to have worse outcome (worse starting point?).

6/ Overall this was a great study and a lot of hear work has gone into it. BMI control and earlier intervention seemed to prevail in this study.
The only thing I couldn't find was whether venous manometry / sinus stents had any different outcomes? @neil_rane @NeuroradLal
The only thing I couldn't find was whether venous manometry / sinus stents had any different outcomes? @neil_rane @NeuroradLal
• • •
Missing some Tweet in this thread? You can try to
force a refresh








