
October is #DysautonomiaAwarenessMonth. Today we are looking at some of the known causes of autonomic dysfunction, and how it is investigated. [THREAD] 

The cause(s) of #autonomicdysfunction in #EDS and #HSD remains unclear. However, some possible causes include:
🧍🏾♀️Increased blood pooling (e.g., in the legs when standing or around the gut after eating)
🩸Low circulating blood volume
🧍🏾♀️Increased blood pooling (e.g., in the legs when standing or around the gut after eating)
🩸Low circulating blood volume
💊 Medications with side effects that trigger or make problems worse, auto-immunity (immune responses to the person’s own body)
😷 Too much #histamine in the body (related to #allergy)
⚫️ Rarely, brainstem or spinal cord restriction
😷 Too much #histamine in the body (related to #allergy)
⚫️ Rarely, brainstem or spinal cord restriction
🩺 For a doctor, initially defining a patient’s history is important:
⚫️ Symptoms
⚫️ Triggers
⚫️ Modifying factors
⚫️ Impact on daily life
⚫️ Possible causes
⚫️ Family history
⚫️ Symptoms
⚫️ Triggers
⚫️ Modifying factors
⚫️ Impact on daily life
⚫️ Possible causes
⚫️ Family history
Many of the common cardiovascular autonomic symptoms relate to changes in posture. They occur when changing from a lying or sitting to a standing position, or with maintaining upright posture, and are improved but not always completely relieved by sitting or lying down. 
The history may reveal things that trigger or exacerbate these symptoms — heat, prolonged standing, alcohol, dehydration, having a cold, etc. A detailed examination is always warranted.
Other common causes of low blood pressure or fast heart rate should be considered, like medications, dehydration, and deconditioning.
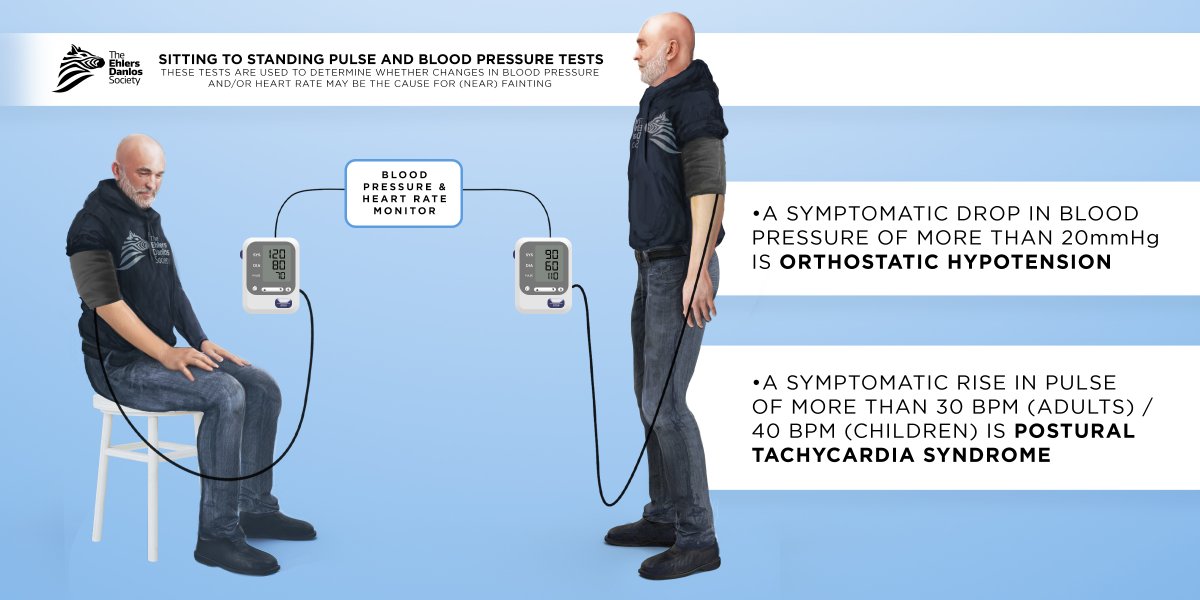
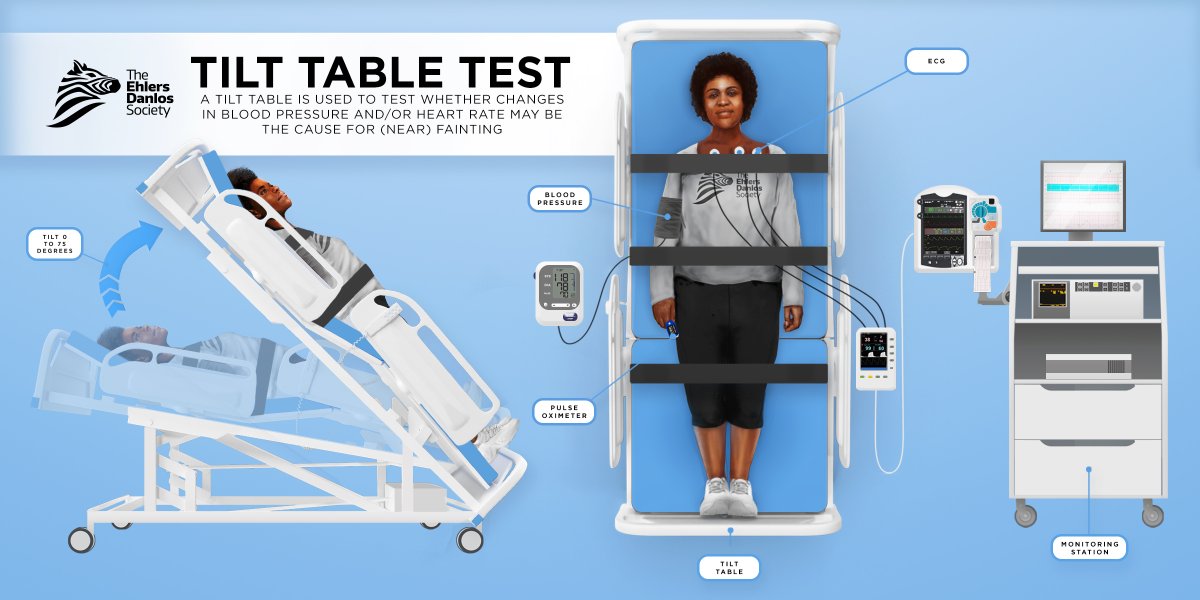
Formal evaluation of cardiovascular autonomic dysfunction is often made with a tilt table test usually done by an autonomic neurologist or electrophysiologist, however, a standard approach is a sitting-to-standing pulse and blood pressure test in the clinic. #Dysautonomia #POTS 
• • •
Missing some Tweet in this thread? You can try to
force a refresh




