
Getting ready for Clinical Controversies in treatment of S. aureus bacteremia. #IDWeek2022 

Increasing recognition that 'persistent' bacteremia should probably be earlier rather than later. Each day longer, associated with increased metastatic complications and mortality.
What is best treatment? ASP or cefazolin? Issues of increased toxicity vs cefazolin inoculum effect.
>>> we need to test in a clinical trial
If still BC+ at 5 days?
No routine role for combination antibiotics - no benefit with rifampin, daptomycin, aminoglycosides in trials
>>> we need to test in a clinical trial
If still BC+ at 5 days?
No routine role for combination antibiotics - no benefit with rifampin, daptomycin, aminoglycosides in trials
Patient case now still BC+ at 11 days after adding rifampin and linezolid
Switched to ertapenem + cefazolin and BC cleared in 24 hr. @DrToddLee @victornizet
>>> @snap_trial would like to test this combination
See Ulloa CID 2020 for 11 cases successfully salvaged
Switched to ertapenem + cefazolin and BC cleared in 24 hr. @DrToddLee @victornizet
>>> @snap_trial would like to test this combination
See Ulloa CID 2020 for 11 cases successfully salvaged
See Gilbertie OFID 2022 - initially 3-16 days bacteremic, cleared within 24 hr.
Mechanism - ertapenem inhibits PBP1; cefazolin inhibits PBP2 (similar thought to ceftriaxone + ampicillin for E faecium)
Mechanism - ertapenem inhibits PBP1; cefazolin inhibits PBP2 (similar thought to ceftriaxone + ampicillin for E faecium)
For isolates with CzIE, no such inoculum effect with ertapenem
Synergy for some isolates in vitro
Rat model of endocarditis - synergy also (even more)
Synergy for some isolates in vitro
Rat model of endocarditis - synergy also (even more)
Synergistic killing of MSSA biofilms
Immunomodulatory effects - increased susceptibility to neutrophil killing
@DrToddLee - maybe we should just do this in @snap_trial with / without grant
Immunomodulatory effects - increased susceptibility to neutrophil killing
@DrToddLee - maybe we should just do this in @snap_trial with / without grant
Next Warren Rose @Warren_E_Rose on whether daptomycin + ceftaroline should become standard of care?
Q&A: What about after the bacteremia then clears? Usually continue for 2 weeks and then step back to monotherapy
MRSA bacteremia is bad. Can we improve upon standard of care?
Makes excellent point that there are some factors that can't be changed - e.g., age, that impact on outcomes
Makes excellent point that there are some factors that can't be changed - e.g., age, that impact on outcomes
Noted limited SOC head to head studies (daptomycin vs vancomycin, remembering that Fowler registrational trial included aminoglycosides)
Combination therapies have not shown benefit
Combination therapies have not shown benefit
How about daptomycin + ceftaroline?
Sakoulas Clin Ther 2014. Case series of 20 patients for salvage therapy. These patients did well.
McCreary OFID 2020 Multicenter cohort of DAP+CPT vs SOC @ErinMcCreary. Giving early, cleared earlier. Lower mortality.
Sakoulas Clin Ther 2014. Case series of 20 patients for salvage therapy. These patients did well.
McCreary OFID 2020 Multicenter cohort of DAP+CPT vs SOC @ErinMcCreary. Giving early, cleared earlier. Lower mortality.
Additional cohort studies
One RCT. Geriak AAC 2019. Stopped early. No mortality in DAP+CPT group. A number of criticisms and limitations.
Volk CID 2020 - serum from Geriak study. Il-1B higher in DAP+CPT group.
One RCT. Geriak AAC 2019. Stopped early. No mortality in DAP+CPT group. A number of criticisms and limitations.
Volk CID 2020 - serum from Geriak study. Il-1B higher in DAP+CPT group.

Nichols OFID 2021 - de-escalation after 3-10 days DAP+CPT. De-escalation safe.
Rose CID 2021 - systematic review of proportion of patients with endocarditis / endovascular. Higher in retrospective studies (up to 30%) vs trials.
So applies to a significant number of patients
Rose CID 2021 - systematic review of proportion of patients with endocarditis / endovascular. Higher in retrospective studies (up to 30%) vs trials.
So applies to a significant number of patients
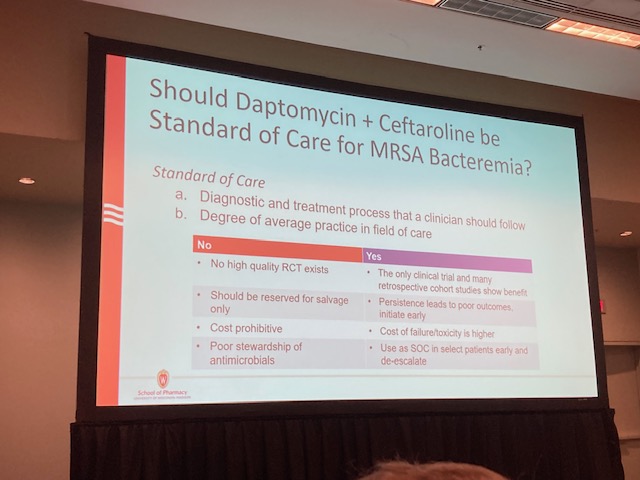
Future trial landscape?
Adaptive trials
Early DAP+CPT vs SOC
De-escalation from combination to monotherapy
Adaptive trials
Early DAP+CPT vs SOC
De-escalation from combination to monotherapy

Q&A
Should we test monotherapy first? Could all the effect be due to ceftaroline alone. Rose suggests the synergy is important.
Could persistent bacteremia more reflect the host and underlying disease? modifying with antibiotics may not make a difference
Should we test monotherapy first? Could all the effect be due to ceftaroline alone. Rose suggests the synergy is important.
Could persistent bacteremia more reflect the host and underlying disease? modifying with antibiotics may not make a difference
Great talk @Warren_E_Rose !
Next Brian Werth @bdubrx on non standard therapies (lipoglycopeptides, orals)
Oral switch - not controversial for uncomplicated SAB; but less clear for complicated SAB - most data is retrospective and heterogenous. No MRSA in POET. Most studies switch to 2 drugs.
Oral switch - not controversial for uncomplicated SAB; but less clear for complicated SAB - most data is retrospective and heterogenous. No MRSA in POET. Most studies switch to 2 drugs.
Long acting lipoglycopeptides (LPG)
Cross resistance to vanc & dapto
Dalba - 30 min infusion
Many advantages to single dose / weekly dose
Prescription data - increasing use of dalba, including for invasive infections
Cross resistance to vanc & dapto
Dalba - 30 min infusion
Many advantages to single dose / weekly dose
Prescription data - increasing use of dalba, including for invasive infections
Studies heterogenous in quality and data availability
Dalbavancin probably stays above MIC for up to 12 weeks! Even AUC/MIC 111 at 8 weeks.
This can be good, but may lead to overtreatment / dysbiosis / more selection for resistance
Dalbavancin probably stays above MIC for up to 12 weeks! Even AUC/MIC 111 at 8 weeks.
This can be good, but may lead to overtreatment / dysbiosis / more selection for resistance

When studied in vitro - see development of resistance to vanc, then dapto, then dalba.
Described in 4 clinical case series / reports.
Selection may be reduced by combining with nafcillin
Described in 4 clinical case series / reports.
Selection may be reduced by combining with nafcillin
New topic: daptomycin + TMP/SMX
An under-appreciated combination
Steed AAC 2012 and Werth AAC 2014 - clearly synergistic - similar to that with DAP + CPT
But very few case reports of use of the combination
An under-appreciated combination
Steed AAC 2012 and Werth AAC 2014 - clearly synergistic - similar to that with DAP + CPT
But very few case reports of use of the combination
Appears that synergy occurs with DAP susc and DAP resistant; but need TMP/SMX susceptibility
Need for RCTs - mention of DOTS
Need for RCTs - mention of DOTS

• • •
Missing some Tweet in this thread? You can try to
force a refresh





