An overly-long and still non-comprehensive reading list for understanding #NIRS #muscleoxygenation in sport science! 🧵
1/15
Start with this concise opinion piece from Perrey on the emerging promise and future direction of NIRS research & application
pubmed.ncbi.nlm.nih.gov/35321522/
1/15
Start with this concise opinion piece from Perrey on the emerging promise and future direction of NIRS research & application
pubmed.ncbi.nlm.nih.gov/35321522/

2/15
Perrey & Ferrari's review on NIRS in the context of sport science gives background and is a great jumping off point for NIRS studies in your particular sport of interest
pubmed.ncbi.nlm.nih.gov/29177977/
Perrey & Ferrari's review on NIRS in the context of sport science gives background and is a great jumping off point for NIRS studies in your particular sport of interest
pubmed.ncbi.nlm.nih.gov/29177977/
3/15
Barstow has a comprehensive overview of technically and biologically important aspects of NIRS, with recommendations for standardised methodology and nomenclature. This is a must read IMO for starting to understand the nuances of NIRS interpretation
pubmed.ncbi.nlm.nih.gov/30844336/
Barstow has a comprehensive overview of technically and biologically important aspects of NIRS, with recommendations for standardised methodology and nomenclature. This is a must read IMO for starting to understand the nuances of NIRS interpretation
pubmed.ncbi.nlm.nih.gov/30844336/

4/15
@JanBoone2906 et al at Ghent University have published definitive experiments describing NIRS response profiles during incremental ramp testing. Start here to visualise how NIRS responds in an intensity-dependent manner
pubmed.ncbi.nlm.nih.gov/27613650/
@JanBoone2906 et al at Ghent University have published definitive experiments describing NIRS response profiles during incremental ramp testing. Start here to visualise how NIRS responds in an intensity-dependent manner
pubmed.ncbi.nlm.nih.gov/27613650/

5/15
@MuriasLab et al at U of Calgary have also exhaustively investigated NIRS responses during exercise, characterising the deoxygenation breakpoint / HHb-plateau along with other threshold demarcations
pubmed.ncbi.nlm.nih.gov/25606817/
@MuriasLab et al at U of Calgary have also exhaustively investigated NIRS responses during exercise, characterising the deoxygenation breakpoint / HHb-plateau along with other threshold demarcations
pubmed.ncbi.nlm.nih.gov/25606817/

6/15
There is a wonderfully productive ongoing debate on the association between NIRS and other physiological breakpoints
pubmed.ncbi.nlm.nih.gov/29975303/
pubmed.ncbi.nlm.nih.gov/30134366/
There is a wonderfully productive ongoing debate on the association between NIRS and other physiological breakpoints
pubmed.ncbi.nlm.nih.gov/29975303/
pubmed.ncbi.nlm.nih.gov/30134366/
7/15
This debate has helped reveal operational limitations of how we use and think about 'thresholds'. To me, a critical aspect is the uncertainty inherent to any breakpoint detection method. Elegantly demonstrated by @KevinCaen @JanBoone2906 et al
pubmed.ncbi.nlm.nih.gov/35435465/
This debate has helped reveal operational limitations of how we use and think about 'thresholds'. To me, a critical aspect is the uncertainty inherent to any breakpoint detection method. Elegantly demonstrated by @KevinCaen @JanBoone2906 et al
pubmed.ncbi.nlm.nih.gov/35435465/

8/15
Another exciting application of NIRS is for non-invasive measurement of mitochondrial function, introduced by Ryan, @InfraredRx, @harrybrossiter et al. This method is now widely used across clinical and sport applications
pubmed.ncbi.nlm.nih.gov/28684592/
pubmed.ncbi.nlm.nih.gov/22582211/
Another exciting application of NIRS is for non-invasive measurement of mitochondrial function, introduced by Ryan, @InfraredRx, @harrybrossiter et al. This method is now widely used across clinical and sport applications
pubmed.ncbi.nlm.nih.gov/28684592/
pubmed.ncbi.nlm.nih.gov/22582211/
9/15
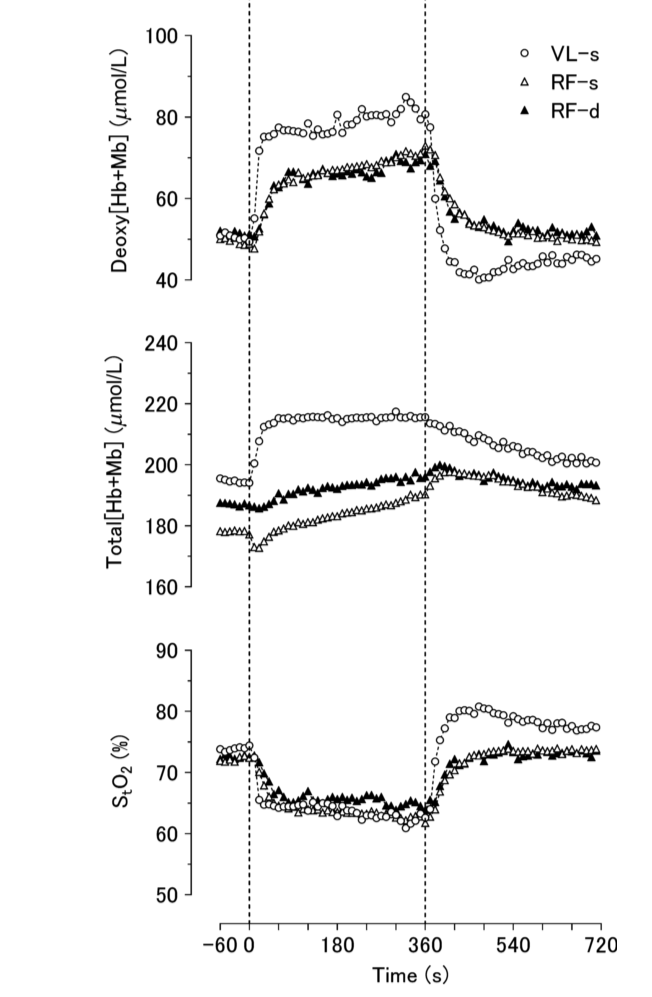
It's important to consider what *isn't* illuminated by NIRS. NIRS is hyper-local. There are critical spatial and (bio)mechanical effects to consider, such as deep vs superficial muscle heterogeneities
pubmed.ncbi.nlm.nih.gov/26404619/
pubmed.ncbi.nlm.nih.gov/28912130/
It's important to consider what *isn't* illuminated by NIRS. NIRS is hyper-local. There are critical spatial and (bio)mechanical effects to consider, such as deep vs superficial muscle heterogeneities
pubmed.ncbi.nlm.nih.gov/26404619/
pubmed.ncbi.nlm.nih.gov/28912130/
10/15
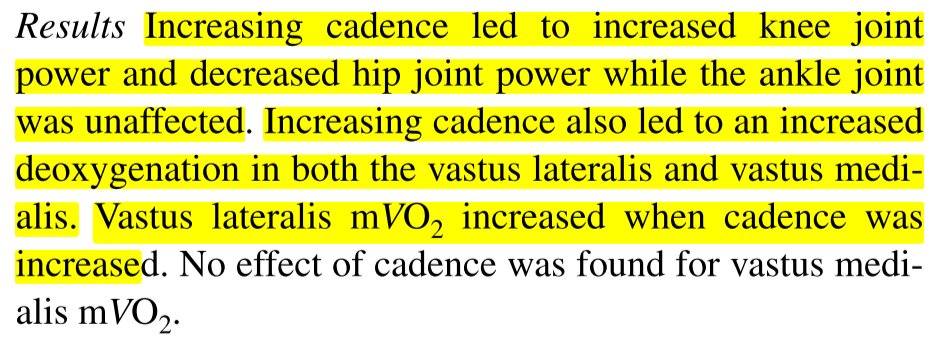
Vastus lateralis is the primary locomotor muscle studied in cycling. Rectus femoris in running. There are important modality- and quadricep head-specific recruitment & deoxygenation patterns
pubmed.ncbi.nlm.nih.gov/28970805/
pubmed.ncbi.nlm.nih.gov/29722622/
Vastus lateralis is the primary locomotor muscle studied in cycling. Rectus femoris in running. There are important modality- and quadricep head-specific recruitment & deoxygenation patterns
pubmed.ncbi.nlm.nih.gov/28970805/
pubmed.ncbi.nlm.nih.gov/29722622/

11/15
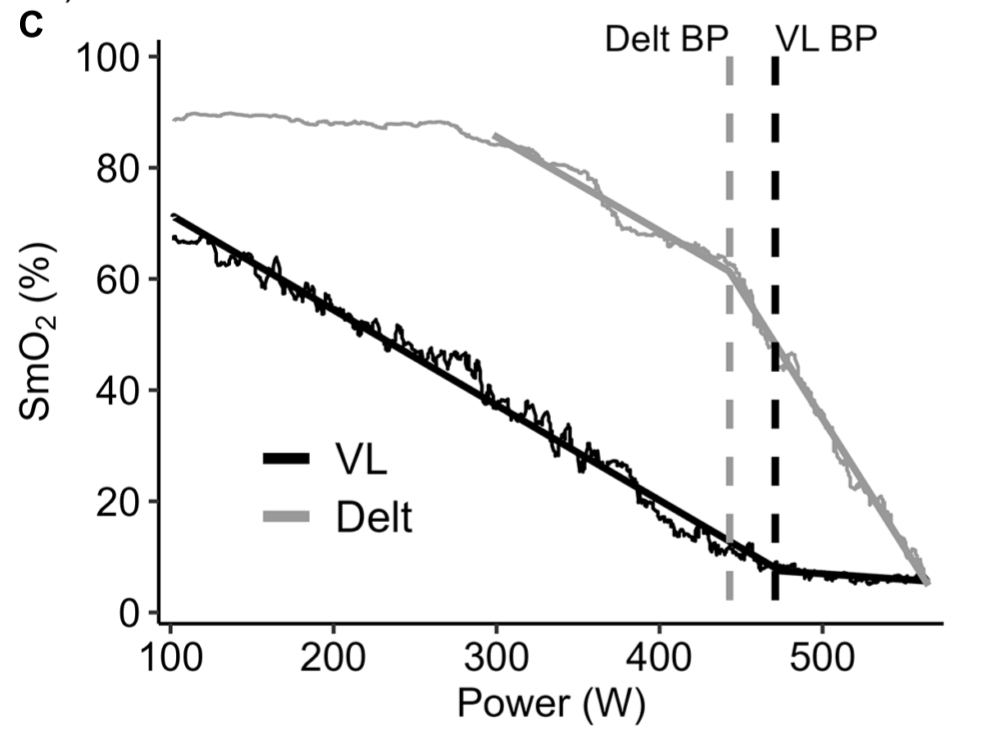
Consider NIRS responses of non-locomotor muscles during exercise such as bicep or deltoid, and what this might reveal in terms of systemic metabolic priorities
pubmed.ncbi.nlm.nih.gov/20204819/
pubmed.ncbi.nlm.nih.gov/35431982/
👆my colleague's paper
Consider NIRS responses of non-locomotor muscles during exercise such as bicep or deltoid, and what this might reveal in terms of systemic metabolic priorities
pubmed.ncbi.nlm.nih.gov/20204819/
pubmed.ncbi.nlm.nih.gov/35431982/
👆my colleague's paper
12/15
Adipose tissue thickness has large effects on NIRS signals. Especially consider differences in male & female subcutaneous fat distribution on quadriceps when interpreting locomotor NIRS signals
pubmed.ncbi.nlm.nih.gov/28151429/
pubmed.ncbi.nlm.nih.gov/28935822/
also
Adipose tissue thickness has large effects on NIRS signals. Especially consider differences in male & female subcutaneous fat distribution on quadriceps when interpreting locomotor NIRS signals
pubmed.ncbi.nlm.nih.gov/28151429/
pubmed.ncbi.nlm.nih.gov/28935822/
also
https://twitter.com/jem_arnold/status/1527371370673635329
13/15
Consider how NIRS measurements at the microvasculature (capillaries) are *expected* to differ from classical experiments that measure at larger conduit vessels (e.g. femoral or brachial aa. & vv.)
pubmed.ncbi.nlm.nih.gov/32940560/
Consider how NIRS measurements at the microvasculature (capillaries) are *expected* to differ from classical experiments that measure at larger conduit vessels (e.g. femoral or brachial aa. & vv.)
pubmed.ncbi.nlm.nih.gov/32940560/

14/15
We have to consider *mechanical effects* like isometric vs rhythmic (e.g. cadence) contractions, which change recruitment patterns and spatial distribution of tissue & fluid volumes into and out of the illuminated area
pubmed.ncbi.nlm.nih.gov/27126859/
pubmed.ncbi.nlm.nih.gov/15557016/
We have to consider *mechanical effects* like isometric vs rhythmic (e.g. cadence) contractions, which change recruitment patterns and spatial distribution of tissue & fluid volumes into and out of the illuminated area
pubmed.ncbi.nlm.nih.gov/27126859/
pubmed.ncbi.nlm.nih.gov/15557016/
15/15
There are so many more applications & nuances to NIRS
Start with the reviews at the top of this thread and come back later for the more nuanced experiments toward the bottom
Dig through the citation trains of these papers to discover what else you might be interested in!
There are so many more applications & nuances to NIRS
Start with the reviews at the top of this thread and come back later for the more nuanced experiments toward the bottom
Dig through the citation trains of these papers to discover what else you might be interested in!
16/15
Or listen / watch me try a few times recently to articulate a story about oxygenation response profiles during incremental exercise testing, trying to keep all of these nuances straight 🥴
scientifictriathlon.com/tts358/
Or listen / watch me try a few times recently to articulate a story about oxygenation response profiles during incremental exercise testing, trying to keep all of these nuances straight 🥴
scientifictriathlon.com/tts358/
Another very recent application from Pilotto, @AdamiAlessandra, @harrybrossiter, @PorcelliSimone et al is the evaluation of O2 diffusion capacity
This is quite exciting to understand muscle O2 delivery & uptake kinetics after higher intensity exercise
pubmed.ncbi.nlm.nih.gov/35930524/
This is quite exciting to understand muscle O2 delivery & uptake kinetics after higher intensity exercise
pubmed.ncbi.nlm.nih.gov/35930524/
• • •
Missing some Tweet in this thread? You can try to
force a refresh


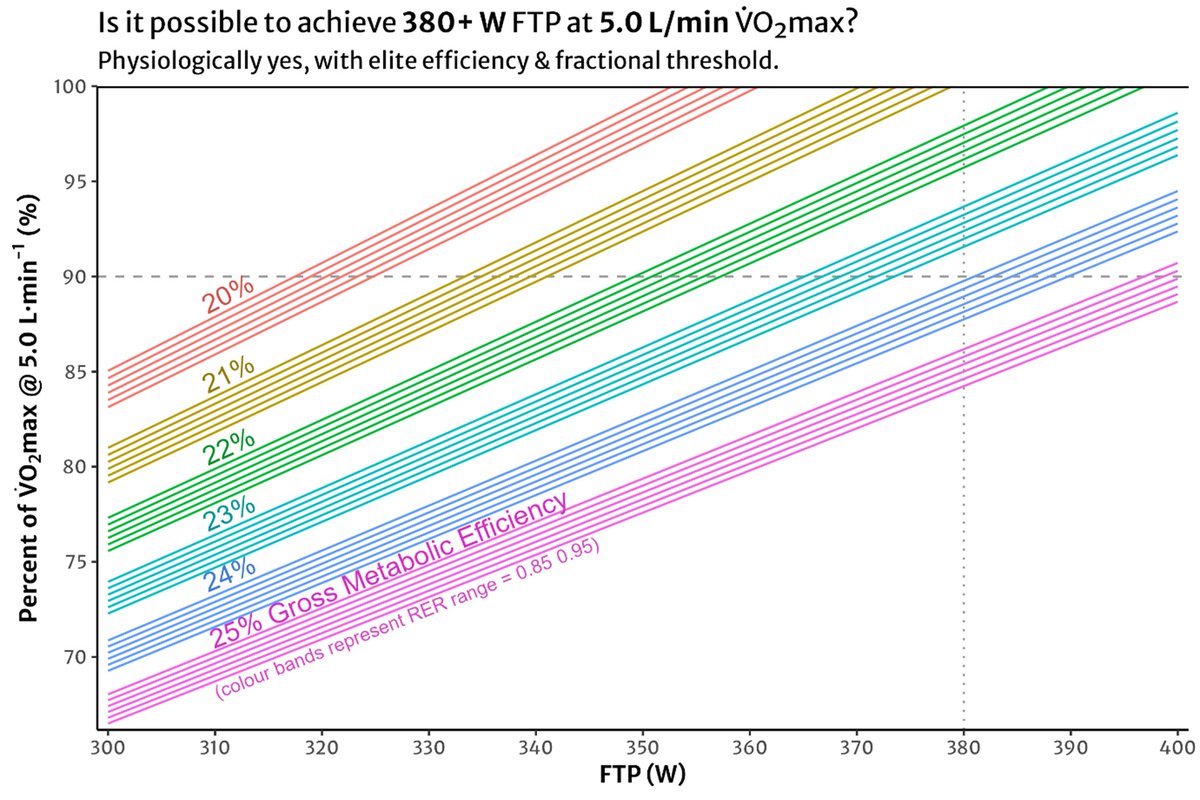
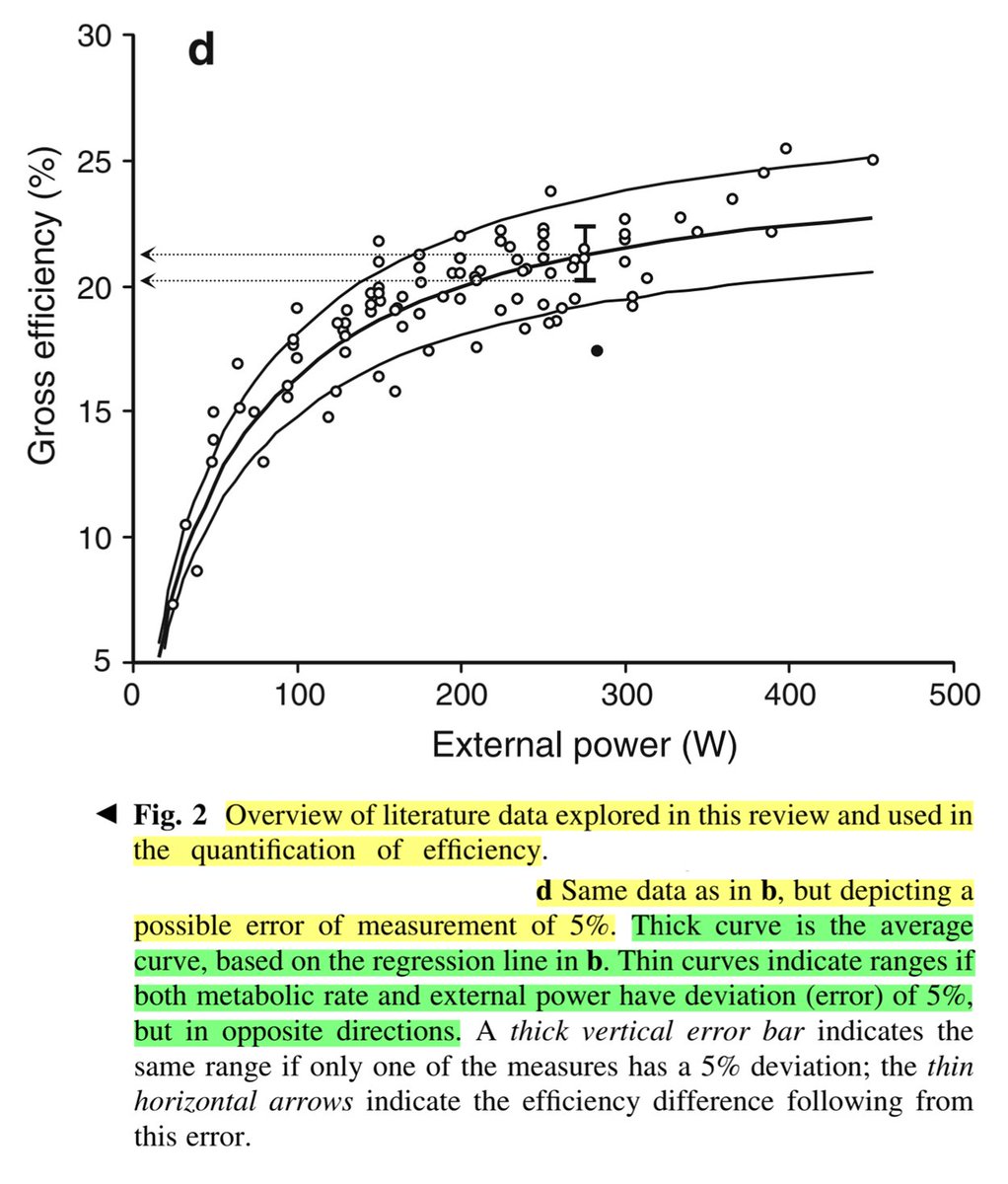
![Figure plotting individually observed gross efficiency (GE) values for cyclists across power output from 50 to 450 W, taken from published cross-sectional data in Ettema & Lorås, 2009. Efficiency in Cycling. A Review. https://www.researchgate.net/publication/24027428_Efficiency_in_cycling_A_review. A logarithmic model predicts GE as a function of PO, with 90% prediction intervals equivalent to ± 2.5% around the marginal estimate. e.g. at 250 W estimated GE = 21%, 90% PI = [18.5, 23.5].](https://pbs.twimg.com/media/G-LJl5ka0AIuANR.jpg)