1/ Let's flip through the Physician Fee Schedule Final Rule just out, w shared savings focus
Here's a little trick to get past all the pesky comments (that people spent 1000's of hours developing and submitting), and right to the meat of the matter:
CTRL-F "we are finalizing"
Here's a little trick to get past all the pesky comments (that people spent 1000's of hours developing and submitting), and right to the meat of the matter:
CTRL-F "we are finalizing"
2/ First up: we want to increase participation!
strong evidence for providing upfront capital, especially to rural, underserved, low income ACOs (see AIM)
Good idea to expand it 👍
Lots of comments about eligibility criteria, repayment, etc etc.
"finalized as proposed"



strong evidence for providing upfront capital, especially to rural, underserved, low income ACOs (see AIM)
Good idea to expand it 👍
Lots of comments about eligibility criteria, repayment, etc etc.
"finalized as proposed"




3/ We want to increase participation!
Let's allow folks to stay in one sided risk for longer, especially lower income (no hospital) ACOs
Makes sense 👍
Lots of comments about who, how, when, etc etc
"finalized as proposed without modification"


Let's allow folks to stay in one sided risk for longer, especially lower income (no hospital) ACOs
Makes sense 👍
Lots of comments about who, how, when, etc etc
"finalized as proposed without modification"



4/ ) Scale Shared Savings Based on Quality Performance-moving away from all-or-nothing
"Cliffs" don't make for great policy, so OK
Also, scaling back losses if high quality makes sense
Unfortunately, lots of comments that weren't technically in scope of this section
"F_ A_ P_"

"Cliffs" don't make for great policy, so OK
Also, scaling back losses if high quality makes sense
Unfortunately, lots of comments that weren't technically in scope of this section
"F_ A_ P_"


5/ Extension of eCQM/MIPS CQM Incentive (to allow ACOs an add'l year to gauge their performance on the eCQM/MIPS CQMs before full reporting of the measures are required beginning in PY 2025)
sadly, we need the time ✔️ FAP!
lots of comments (all-payer!) that were..out of scope
sadly, we need the time ✔️ FAP!
lots of comments (all-payer!) that were..out of scope

6/ Health Equity Adjustment (upwardly adjust quality
performance scores for ACOs that serve a high proportion of underserved individuals)
makes sense 👍
some comments said incentives should be greater, or more timely, or applied more broadly.
"we will not modify our proposal"
performance scores for ACOs that serve a high proportion of underserved individuals)
makes sense 👍
some comments said incentives should be greater, or more timely, or applied more broadly.
"we will not modify our proposal"

7/ BENCHMARKING
Lots of good stuff. Lots of comments
Big Q: who do new rules would apply to? Existing ACOs would like to operate under the new (and generally improved) rules- But CMS proposed to only apply them when new agreement
and .."we decline the commenters' suggestions"
Lots of good stuff. Lots of comments
Big Q: who do new rules would apply to? Existing ACOs would like to operate under the new (and generally improved) rules- But CMS proposed to only apply them when new agreement
and .."we decline the commenters' suggestions"

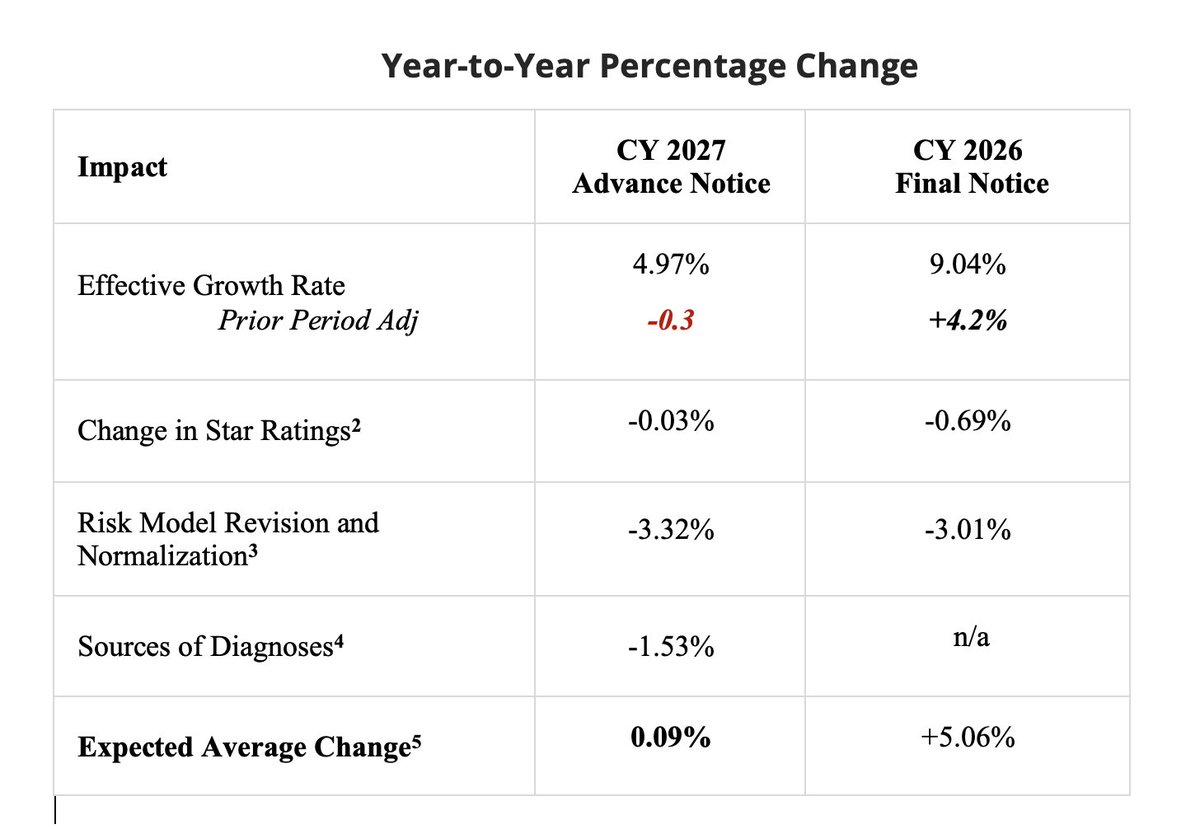
8/ Incorporating a Prospective, External Factor in Growth Rates Used to Update the Historical Benchmark
this deserves more than one tweet, cause it's a big departure.
Instead of benchmark updates being set by observing actual trends, let's begin to set it administratively
👇
this deserves more than one tweet, cause it's a big departure.
Instead of benchmark updates being set by observing actual trends, let's begin to set it administratively
👇

9/ This is not a bad idea.
In fact, one might say it becomes inevitable as CMS approaches their goal of getting close to 100% of beneficiaries in Accountable Care (who serves as comparison?)
Also, its brainchild of wicked smart people @Michael_Chernew @JMichaelMcW @alicejychen
In fact, one might say it becomes inevitable as CMS approaches their goal of getting close to 100% of beneficiaries in Accountable Care (who serves as comparison?)
Also, its brainchild of wicked smart people @Michael_Chernew @JMichaelMcW @alicejychen

10/ @CMSinnovates appropriately did an RFI- asking for broad input into the idea of administrative benchmarking- it will be fascinating to read what they learn.
But it's a bit weird for @CMSGov to simultaneously propose that it's to take effect right away.
What could go wrong?
But it's a bit weird for @CMSGov to simultaneously propose that it's to take effect right away.
What could go wrong?
11/ OK- let me use this example to give you a sense of the thought and effort that goes into regulatory comments.
The #PFS got 23 THOUSAND comments.
some of them are simple.
some of them are sad
And some are really detailed and sophisticated and smart.
🇺🇸


The #PFS got 23 THOUSAND comments.
some of them are simple.
some of them are sad
And some are really detailed and sophisticated and smart.
🇺🇸



12/ We submitted comment letter # 21,649: regulations.gov/comment/CMS-20… signed by @Travis_Broome and @dc_cavanaugh - they are among the very best in the business.
What did we say about admin benchmarking?
First off, great idea!
(always start positive, reader)
What did we say about admin benchmarking?
First off, great idea!
(always start positive, reader)

13/ But there are 2 big problems with CMS picking an inflation factor for the next five years to update ACO budgets
1) You could guess wrong. (pandemic? inflation?)
Pick too high, the govt is paying too much.
Pick too low, docs won't get savings, will drop out of the program.
1) You could guess wrong. (pandemic? inflation?)
Pick too high, the govt is paying too much.
Pick too low, docs won't get savings, will drop out of the program.

14/ the 2nd problem is that if you set a NATIONAL inflation rate, you could create regional winners and losers.
If cost inflation is "sticky" at the regional level, you could get bad selection bias with voluntary participation, and also low levels of adoption in some areas
If cost inflation is "sticky" at the regional level, you could get bad selection bias with voluntary participation, and also low levels of adoption in some areas

15/ FINALLY- a policy question that should be answerable with data.
Is the variation between national and regional cost trends random, subject to reversion to the mean, or sticky?
We ran the data, friend.
(OK, @BarnesBritainy ran the data, friend)
ITS NOT RANDOM. ITS STICKY
Is the variation between national and regional cost trends random, subject to reversion to the mean, or sticky?
We ran the data, friend.
(OK, @BarnesBritainy ran the data, friend)
ITS NOT RANDOM. ITS STICKY

16/ But how hard would it be to pick (or avoid) your region even if true? Maybe the high trend- and low-trend areas are all mixed together?
Nope.
If you were in California (esp LA) between 2015 and 2020 you were fighting a stiff headwind.
In Florida, sweet tailwind.
Nope.
If you were in California (esp LA) between 2015 and 2020 you were fighting a stiff headwind.
In Florida, sweet tailwind.

17/ You know who else thought that we shouldn't put half of our eggs in the national trend basket?
The American Academy of Family Physicians @aafp
Expert groups like @PEPC_DC @HCTTF @TrinityHealthHQ



The American Academy of Family Physicians @aafp
Expert groups like @PEPC_DC @HCTTF @TrinityHealthHQ




18/ The National Association of Accountable Care Organizations, the closest thing we have to the voice of value-based organizations in the country did their own analysis.
They didn't like it either.

They didn't like it either.


19/ All these organizations said some version of:
slow down, there's no burning need to introduce national administrative benchmarks so quickly, so prominently
If you decide to go ahead, please put some more guardrails in, to ensure that the damage is limited.
What happened?
slow down, there's no burning need to introduce national administrative benchmarks so quickly, so prominently
If you decide to go ahead, please put some more guardrails in, to ensure that the damage is limited.
What happened?

20/ "We decline commenters’ suggestions"
"We disagree with the commenters’ suggestion"
"we decline at this time to adopt commenters’ suggestions"
"We decline to delay implementation"
After consideration of the public comments, we are finalizing without modification our proposal
"We disagree with the commenters’ suggestion"
"we decline at this time to adopt commenters’ suggestions"
"We decline to delay implementation"
After consideration of the public comments, we are finalizing without modification our proposal
21/ I was a federal policymaker @HHSGov
I've been an avid fan and follower of the regulatory process for a long time over many cycles.
I honestly can't recall a final reg that is no unchanged from the proposed,
that exhibits so little curiosity to the input of stakeholders.
I've been an avid fan and follower of the regulatory process for a long time over many cycles.
I honestly can't recall a final reg that is no unchanged from the proposed,
that exhibits so little curiosity to the input of stakeholders.
22/ This is not a bad reg.
Many of the policies are good and smart.
Policymakers can disagree with any of our proposals, but the idea that none of the 22,000 commenters had anything worth listening to is incredible.
Many of the policies are good and smart.
Policymakers can disagree with any of our proposals, but the idea that none of the 22,000 commenters had anything worth listening to is incredible.
• • •
Missing some Tweet in this thread? You can try to
force a refresh