Palliative care: Opioids 🧵
Alfentanil and Fentanyl belong to the Phenylpiperidine family and have a much higher affinity for Mu opioid receptors than Morphine and Oxycodone which belong to the Phenanthrene class.
They are more potent but this difference has other implications
Alfentanil and Fentanyl belong to the Phenylpiperidine family and have a much higher affinity for Mu opioid receptors than Morphine and Oxycodone which belong to the Phenanthrene class.
They are more potent but this difference has other implications
You decide to rotate a person taking 150mg of oral morphine/day to an equivalent transdermal Fentanyl patch. Their pain is stable and they are fed up taking so many pills. You do the maths and decide on a 50microgram/hour patch.
You start the Fentanyl patch and stop the patients morphine.
Day 1 all is well
Day 2 patient feeling a bit achey all over and has a headache
Day 3 patient has diarrhoea, abdominal cramps, restlessness and feels dreadful. They are yawning and have goosebumps
Day 1 all is well
Day 2 patient feeling a bit achey all over and has a headache
Day 3 patient has diarrhoea, abdominal cramps, restlessness and feels dreadful. They are yawning and have goosebumps
They are experiencing opioid withdrawal……. But hold on…They are receiving the equivalent dose of opioid to what they had before and Fentanyl is a more potent Mu receptor agonist!
What is going on?
What is going on?
Morphine acts on the Mu receptor and Fentanyl has that covered.
Morphine also acts to varying degrees on the Delta and Kappa opioid receptors which are not activated as well by Fentanyl. These receptors are not happy and withdrawal is occurring.
Morphine also acts to varying degrees on the Delta and Kappa opioid receptors which are not activated as well by Fentanyl. These receptors are not happy and withdrawal is occurring.
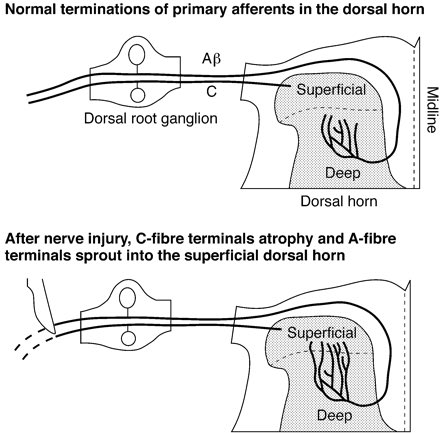
Opioid receptors are concentrated in the CNS but are also found in the peripheral nerves and end organs such as the bowels.
Fentanyl is highly liphophilic so it rapidly dissipates into the CNS leaving those more peripheral Mu receptors a little underwhelmed.
Fentanyl is highly liphophilic so it rapidly dissipates into the CNS leaving those more peripheral Mu receptors a little underwhelmed.
When you rotate from a Phenanthrene to a Phenylpiperidine too quickly you can precipitate this unpleasant seemingly paradoxical opioid withdrawal.
Abdominal cramps and loose stools may be main symptoms
Abdominal cramps and loose stools may be main symptoms
2 ways to reduce the risk
-Carry out the rotation in smaller steps over a longer period.
-Have the original morphine or oxycodone available as an immediate release preparation to be used for pain/withdrawal
Speak with your palliative care colleagues or pain team for advice
-Carry out the rotation in smaller steps over a longer period.
-Have the original morphine or oxycodone available as an immediate release preparation to be used for pain/withdrawal
Speak with your palliative care colleagues or pain team for advice
This withdrawal reaction is far less likely to happen when rotating the opposite way back to morphine or oxycodone.
Weird stuff eh… really important though as opioid withdrawal is awful and can be mistaken for other/worsening illness leading to unnecessary distress
Weird stuff eh… really important though as opioid withdrawal is awful and can be mistaken for other/worsening illness leading to unnecessary distress
Opioid conversion tables and calculations are helpful but are only part of the much more complex skill that is Opioid Rotation.
Not all opioids are equal
Not all opioids are equal
As always this is how I understand this areas and the thread is designed to open up discussion and learning (especially me 😉)
• • •
Missing some Tweet in this thread? You can try to
force a refresh