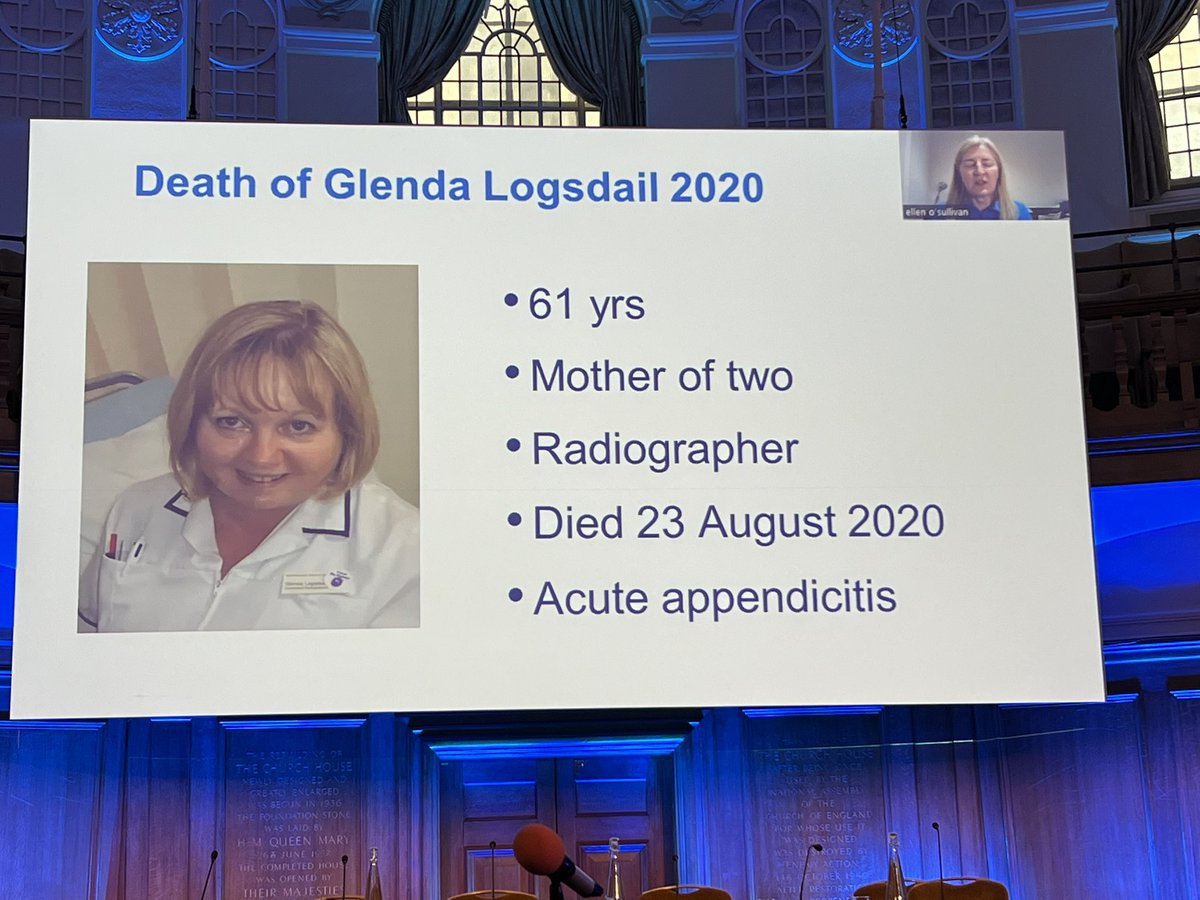
@ProfEllenO pre-recorded lecture (hope she’s okay?) on avoiding oesophageal intubation at #OAA3dc2022. Talk will focus on preventing unrecognized oesophageal intubation & @Anaes_Journal article from @UniversalAirway (PUMA group) - link below #OAA3dc2022
…-publications.onlinelibrary.wiley.com/doi/10.1111/an…



…-publications.onlinelibrary.wiley.com/doi/10.1111/an…




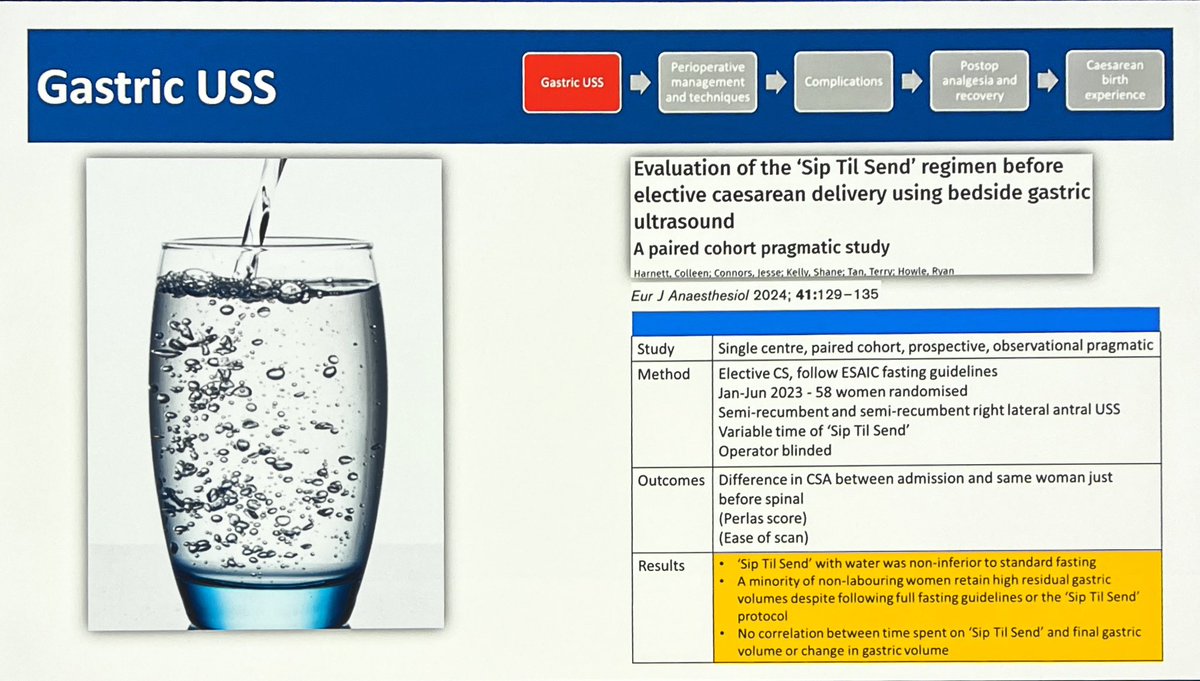
#OBAnes not immune to oesophageal intubation, and at higher risk (historically at very least) of difficult airway. Current findings, although looking at a very niche subset of patients, bear that out. #OAA3dc2022 




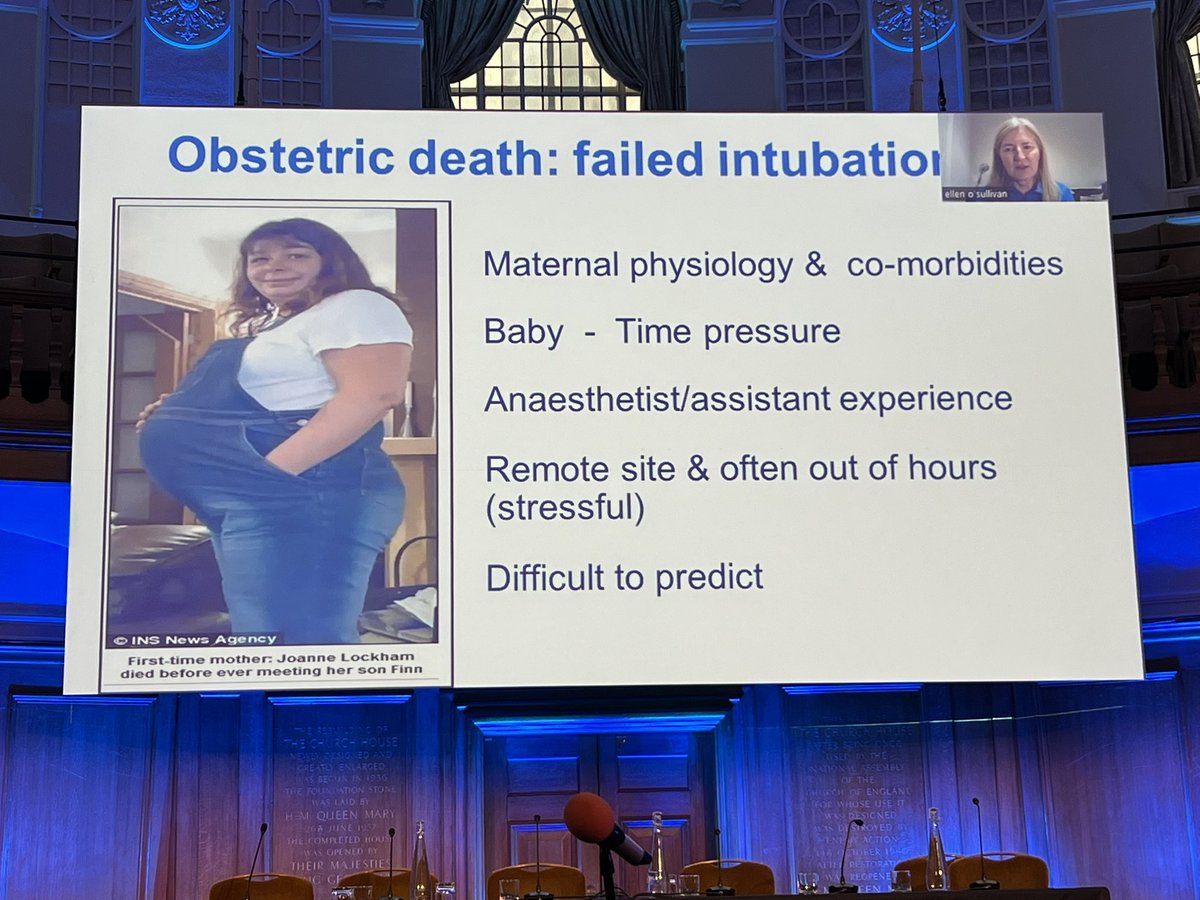


Regulation 28 sent to @RCoANews - anæsthetist unaware of “no trace = wrong place”. PUMA group @UniversalAirway guidelines in @Anaes_Journal, added aim to address human factors. ALWAYS monitors exhaled CO2 and SpO2 during airway management #OAA3dc2022 







Defining sustained exhaled CO2 (aspire to waveform capnography everywhere) - ALL criteria must be met. Operator and assistant should verbalized and confirm sustained CO2 and adequate SpO2. #OAA3dc2022 







Standardize and improve distinctiveness of variables on monitor. @UniversalAirway provide an algorithm for avoiding oesophageal intubation #OAA3dc2022 





Steps 1-4 have to be met, if not REMOVE ETT and ventilate. If ALL steps good - leave ETT in #OAA3dc2022 







More on step 3: has oesophageal intubation been excluded - minimum 2 checks direct visualization AND fibre optic, US or oesophageal detector (this may NOT be universally available, but aspirational and steps should be taken to provide this step) #OAA3dc2022 



BEWARE glottic impersonation (even VL can fail). @drlauraduggan @CJA_Journal. This is more likely during emergency cases - stress induced impaired decision making: #humanfactors (see @Airwayman1 lecture) How to AVOID? #OAA3dc2022 







Avoid by deliberate observation of ETT placement - identify anatomical structures! NB reminder - more likely in emergency situations! #humanfactors
#OAA3dc2022


#OAA3dc2022



Guideline emphasizes role of assistant (if have one) observing view during VL (if have one) and confirming sustained CO2 and adequate SpO2 (this any nurse can definitely do). Wherever possible, use VL (aspirational) - remember first attempt = best attempt. VERBALISE! #OAA3dc2022 







VL vs DL in @cochranecollab by @VirtueOfNothing @doctimcook et al. Hyperangulated VL —> less esophageal intubation. Key takeaways: VL (when familiar gear) likely provides safer risk profile vs DL. #OAA3dc2022 





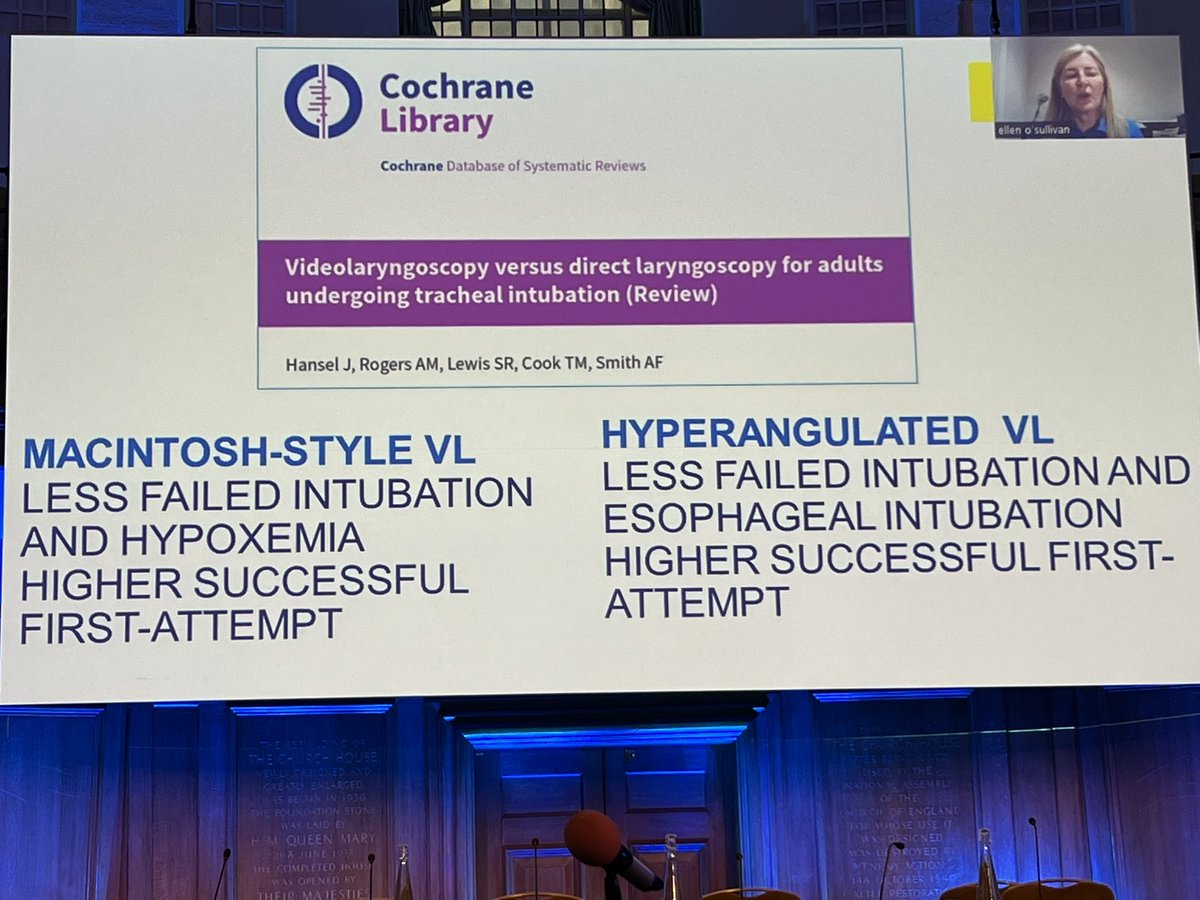

In UK: VL (not standardized) available in 91% of OR’s; only 50% ICU and OB units.<33% widespread use or enthusiasm.@noolslucas and @oldandbaffled recommend availability and use of VL in #OBAnes (@BJAJournals). VL has #humanfactors advantages. VERBALIZE! #OAA3dc2022 







Traditional methods of checking, including auscultation & CXR, discouraged. Auscultation was good in 100% of unexpected oesophageal intubations. Absence of signs = confirm oesophageal intubation NOT EXCLUDE IT #OAA3dc2022 






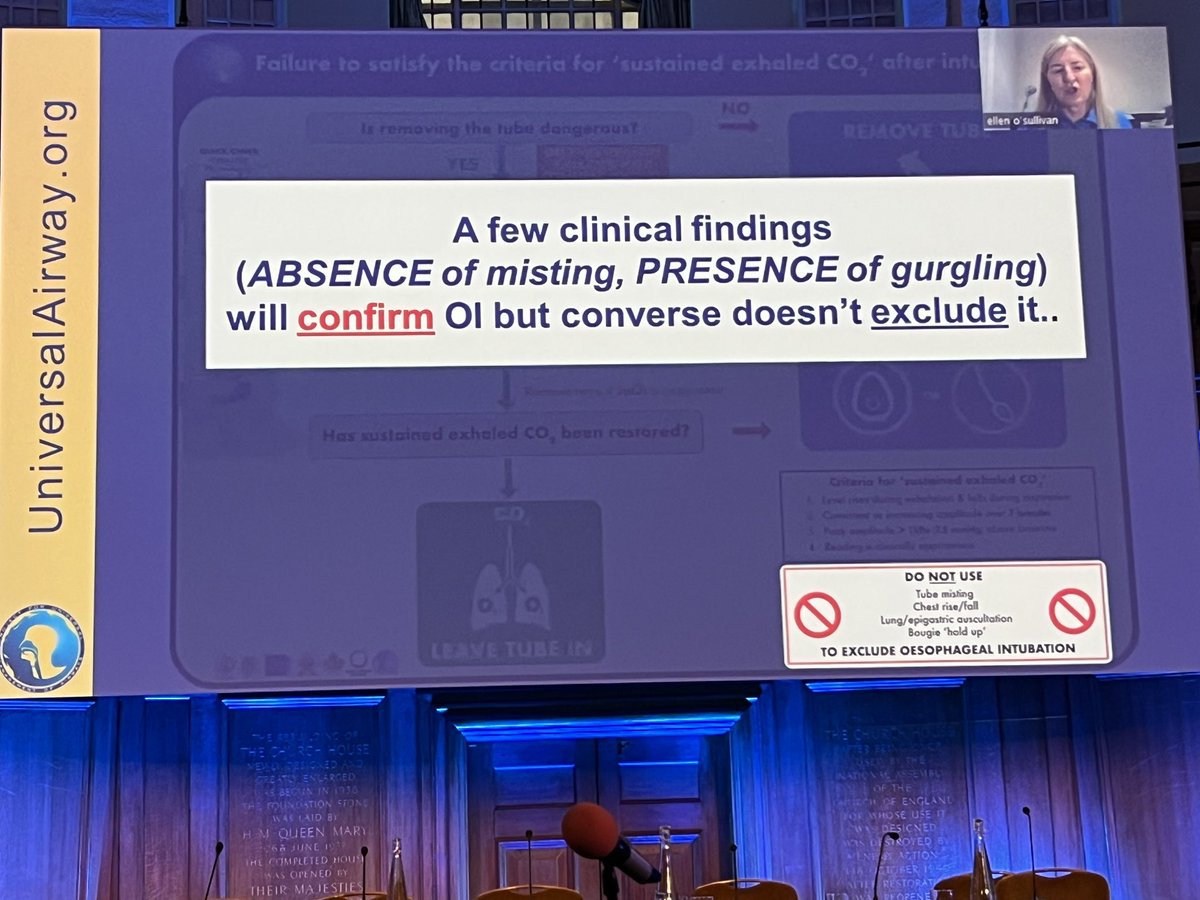
Quick check: equipment - confirm functionality of canograph, ? Replace equipment proximal to ETT; airway - exclude a leak (is cuff up?), assess latency of ETT; patient - exclude bronchospasm, check pulse (unlikely to cause absent CO2) #OAA3dc2022 







NB patient check is unlikely cause of no sustained CO2. Ensure adequate inspiratory pressure & expiration time (with evidence of air movement). Check pulse and start compressions PRN. #OAA3dc2022 





If moving air and have a pulse, patient is implausible cause of absence of sustained CO2. An attenuated trace is not flat/ absent. #OAA3dc2022 



A summary from @ProfEllenO: unrecognized oesophageal intubation is AVOIDABLE, always FATAL if not detected rapidly, waveform capnographu is best tool. @UniversalAirway guidelines offer best steps to prevent - please read @Anaes_Journal article. #OAA3dc2022 







@UniversalAirway PUMA group timeline has lots more! #OAA3dc2022
https://twitter.com/UniversalAirway/status/1593056491019591680
@threadreaderapp unroll please #OAA3dc2022
• • •
Missing some Tweet in this thread? You can try to
force a refresh