1/
Fri. 4PM. You just got consult #8.
Then, a call: "We have a new consult. This patient's been here for 2 weeks. We’re not sure what’s going on & wanted you on board.”
😱
You: "…so, what’s the question…?"
How do we improve this interaction?
This week: Receiving Consults
Fri. 4PM. You just got consult #8.
Then, a call: "We have a new consult. This patient's been here for 2 weeks. We’re not sure what’s going on & wanted you on board.”
😱
You: "…so, what’s the question…?"
How do we improve this interaction?
This week: Receiving Consults
2/
About 3 yrs ago on a thread about the cognitive aspects of consults I posted this poll:
Nearly 2/3 of >1100 respondents said “anticipated pushback” was the biggest anxiety-inducing factor when calling a consult.
This is a problem.
About 3 yrs ago on a thread about the cognitive aspects of consults I posted this poll:
https://twitter.com/VarunPhadke2/status/1233841954615681025
Nearly 2/3 of >1100 respondents said “anticipated pushback” was the biggest anxiety-inducing factor when calling a consult.
This is a problem.
3/
"Pushback" can be intentional or perceived. Either way it is not a desirable component of consultation (for EITHER side).
This week our focus is the consult request interaction, including its goals & downstream consequences, and strategies to make it more productive.
"Pushback" can be intentional or perceived. Either way it is not a desirable component of consultation (for EITHER side).
This week our focus is the consult request interaction, including its goals & downstream consequences, and strategies to make it more productive.
4/
There are “cognitive” 🧠 & “social” 🤝 aspects of the initial consult request.
We focus a lot on the former, but I’ll make a case that the latter is more important.
But let’s start w/ the cognitive piece - what info do consultants need to get from the initial interaction?
There are “cognitive” 🧠 & “social” 🤝 aspects of the initial consult request.
We focus a lot on the former, but I’ll make a case that the latter is more important.
But let’s start w/ the cognitive piece - what info do consultants need to get from the initial interaction?
5/
Of course, the “consult QUESTION”…right?
Yes, the quality of the “consult question” is often identified as THE most important factor in the *perceived* quality/impact of a consult.
It’s also been linked to better downstream teaching interactions!
pubmed.ncbi.nlm.nih.gov/26077219/
Of course, the “consult QUESTION”…right?
Yes, the quality of the “consult question” is often identified as THE most important factor in the *perceived* quality/impact of a consult.
It’s also been linked to better downstream teaching interactions!
pubmed.ncbi.nlm.nih.gov/26077219/
6/
Given this prevailing wisdom, there are many frameworks to help improve the consult request & ALL of them emphasize having a “good” question.
They also all target the team REQUESTING the consult.
But what about the team RECEIVING the consult?
Given this prevailing wisdom, there are many frameworks to help improve the consult request & ALL of them emphasize having a “good” question.
They also all target the team REQUESTING the consult.
But what about the team RECEIVING the consult?

7/
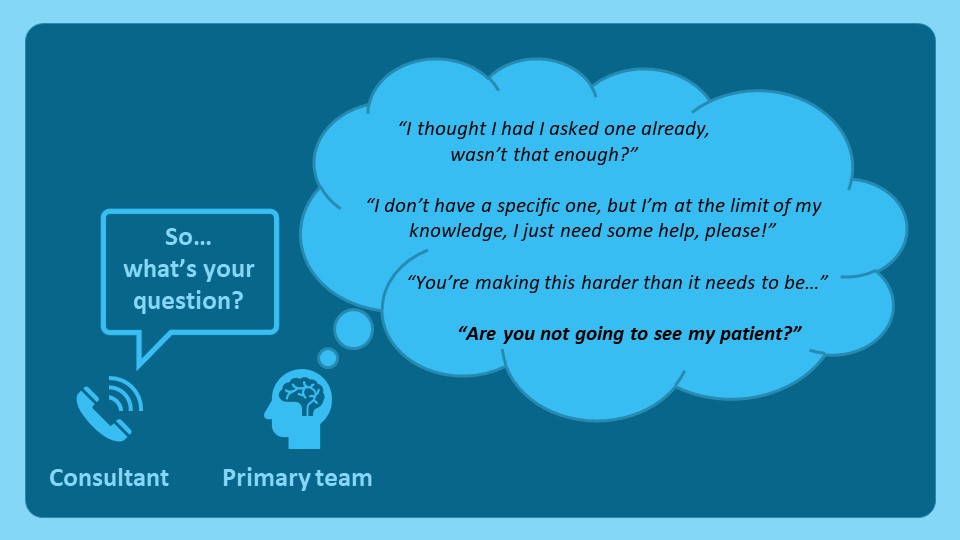
For consultants, our contribution to this interaction often goes: “so…what’s your QUESTION?”
Try asking this WITHOUT it coming across as annoyed. (H/T to @jen_babik)
Indeed, despite our best intentions, the primary team may perceive this question VERY differently.
For consultants, our contribution to this interaction often goes: “so…what’s your QUESTION?”
Try asking this WITHOUT it coming across as annoyed. (H/T to @jen_babik)
Indeed, despite our best intentions, the primary team may perceive this question VERY differently.
8/
Instead of fixating on a specific consult “question” upfront – which may prematurely narrow the scope of our input – a lower stakes & more achievable goal is simply to establish the consult “type”.
Here’s a framework adapted from how I discuss this with our fellows.
Instead of fixating on a specific consult “question” upfront – which may prematurely narrow the scope of our input – a lower stakes & more achievable goal is simply to establish the consult “type”.
Here’s a framework adapted from how I discuss this with our fellows.

9/
Now, I hear the naysayers already.
How will they learn to ask “good questions”?
How will I know what I’m being asked to do?
But maybe I really DON’T need to do a full consult?
All fair points.
But, is the consult request phone call really the optimal time to address them?
Now, I hear the naysayers already.
How will they learn to ask “good questions”?
How will I know what I’m being asked to do?
But maybe I really DON’T need to do a full consult?
All fair points.
But, is the consult request phone call really the optimal time to address them?
10/
The consult question IS an important framing device. But, harping on it can convey hesitance & be counterproductive.
What can we say to keep things more open-ended?
🌟 How can we help?
🌟 What’s worrying you?
And we can always clarify the "ask" AFTER seeing the patient!
The consult question IS an important framing device. But, harping on it can convey hesitance & be counterproductive.
What can we say to keep things more open-ended?
🌟 How can we help?
🌟 What’s worrying you?
And we can always clarify the "ask" AFTER seeing the patient!
11/
Let’s pivot to the “social” aspects of the consult request interaction.
The CONTEXT of the consult process (time/workload pressures) underlies most of what we call “pushback”.
@gradydoctor captured this perfectly in this thread
Let’s pivot to the “social” aspects of the consult request interaction.
The CONTEXT of the consult process (time/workload pressures) underlies most of what we call “pushback”.
@gradydoctor captured this perfectly in this thread
https://twitter.com/gradydoctor/status/1206800311823806465
12/
These contextual factors can translate into explicit or implicit disagreement about the need (“appropriateness”), urgency, sophistication, or “interestingness” of the consult request. This is “pushback”.
How do we mitigate this?
The interpersonal dynamic is key.
These contextual factors can translate into explicit or implicit disagreement about the need (“appropriateness”), urgency, sophistication, or “interestingness” of the consult request. This is “pushback”.
How do we mitigate this?
The interpersonal dynamic is key.
13/
In semi-structured interviews w/ physicians in EM/IM/surgery, Chan et al (2014) identified conflict-mitigating & exacerbating factors in the referral-consultation dynamic (see table).
Which factors rose to the top?
✅ Familiarity
✅ Empathy
✅ Humility
✅ Professionalism
In semi-structured interviews w/ physicians in EM/IM/surgery, Chan et al (2014) identified conflict-mitigating & exacerbating factors in the referral-consultation dynamic (see table).
Which factors rose to the top?
✅ Familiarity
✅ Empathy
✅ Humility
✅ Professionalism

14/
We know these from experience.
Consultants don’t push back when they know the caller, empathize w/ their dilemma, & perceive equal engagement in the problem, no matter what it is.
The challenge is time.
How do we cultivate all this in a brief phone call?
We know these from experience.
Consultants don’t push back when they know the caller, empathize w/ their dilemma, & perceive equal engagement in the problem, no matter what it is.
The challenge is time.
How do we cultivate all this in a brief phone call?
15/
Some strategies:
1⃣ Frame the callback by accepting the consult – negotiate about WHEN you'll see the patient, not IF
2⃣ Convey empathy – acknowledge the clinical dilemma, no matter what it is
3⃣ Express humility/curiosity – the consult is often not what you think it is
Some strategies:
1⃣ Frame the callback by accepting the consult – negotiate about WHEN you'll see the patient, not IF
2⃣ Convey empathy – acknowledge the clinical dilemma, no matter what it is
3⃣ Express humility/curiosity – the consult is often not what you think it is

16/
This seems easy. BUT:
Have I had less than ideal initial consult interactions? For sure.
Have I given “pushback”? Sad to say, but yes.
Have I let “context” best me? Many times.
Do I think receiving consults effectively is a skill I can intentionally develop/improve? YES!
This seems easy. BUT:
Have I had less than ideal initial consult interactions? For sure.
Have I given “pushback”? Sad to say, but yes.
Have I let “context” best me? Many times.
Do I think receiving consults effectively is a skill I can intentionally develop/improve? YES!
17/
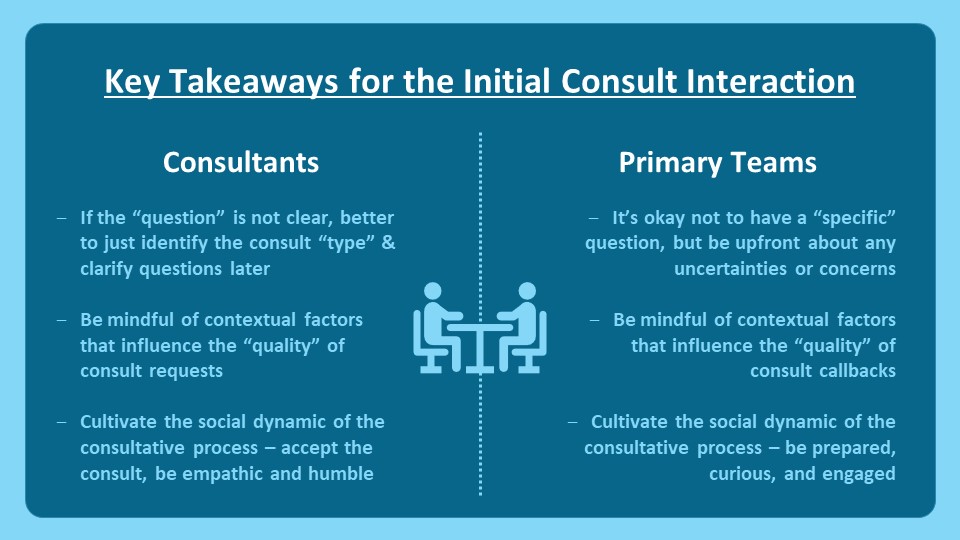
To recap:
The initial consult interaction has important cognitive & social elements, & its success depends on inputs from both sides.
In this thread I’ve outlined strategies to help consultants/specialty trainees be a bit more “meta” about this routine aspect of our work.
To recap:
The initial consult interaction has important cognitive & social elements, & its success depends on inputs from both sides.
In this thread I’ve outlined strategies to help consultants/specialty trainees be a bit more “meta” about this routine aspect of our work.
18/
Next week @JenniferSpicer4 will continue this series on “Teaching Consultant Skills,” with “Effective Data Gathering.”
Remember to check out #SubspecialtyTeaching @MedEdTwagTeam to keep up with all our threads in one place!
See you next week!
Next week @JenniferSpicer4 will continue this series on “Teaching Consultant Skills,” with “Effective Data Gathering.”
Remember to check out #SubspecialtyTeaching @MedEdTwagTeam to keep up with all our threads in one place!
See you next week!

• • •
Missing some Tweet in this thread? You can try to
force a refresh