1/ *Re-consult 📞*
You: What did the last consult note say?
Them: I don't know how to interpret it...
*reading the ✍️ yourself*
#Sepsis
- send tick serologies
- start broad-spectrum antibiotics
- we will follow up OSH data
You: 🤦 I feel you... We'll see the patient again.
You: What did the last consult note say?
Them: I don't know how to interpret it...
*reading the ✍️ yourself*
#Sepsis
- send tick serologies
- start broad-spectrum antibiotics
- we will follow up OSH data
You: 🤦 I feel you... We'll see the patient again.

2/ You wonder...
💭 What tick serologies were we referring to?
💭 What antibiotics were we wanting to start?
💭 And which OSH has prior records?
And you're not the only one wondering...
How can we ✍️ more effective notes?
💭 What tick serologies were we referring to?
💭 What antibiotics were we wanting to start?
💭 And which OSH has prior records?
And you're not the only one wondering...
How can we ✍️ more effective notes?
3/ Clinical notes are used for many purposes, as previously highlighted by @YihanYangMD
https://twitter.com/YihanYangMD/status/1551959943036538880
4/ As specialists, our notes are an important way for us to communicate with the primary team & other consultants to:
📌 Summarize relevant data
📌 Explain our thought process
📌 Communicate our recommendations
📌 Summarize relevant data
📌 Explain our thought process
📌 Communicate our recommendations
5/ Therefore, on consult teams, we need to teach our learners (and ourselves) how to ✍️ effective notes.
So what makes an effective consult note?
So what makes an effective consult note?
6/ Whereas primary team notes are a "journal entry" of the patient's hospitalization, consult notes should be more focused by:
📌 Defining the consult "ask"
📌 Curating data relevant to the "ask"
📌 Clearly answering the consult "ask"
📌 Defining the consult "ask"
📌 Curating data relevant to the "ask"
📌 Clearly answering the consult "ask"

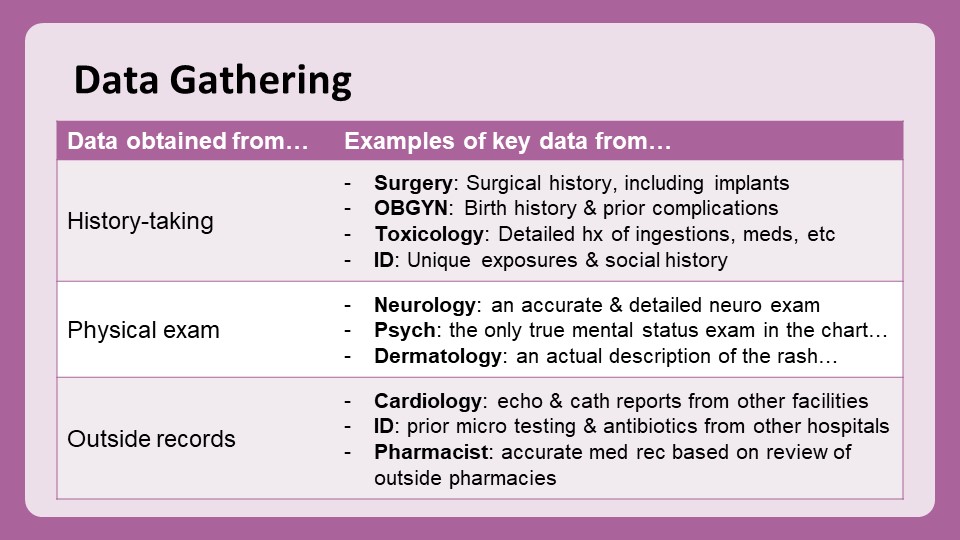
7/ 1⃣ Data GATHERING:
Specialists have expertise in gathering data relevant to their field, including:
✅ Specific historical information
✅ Specialized physical exam findings
✅ Outside records (hospitals, health department, etc)
And we go to their notes to find these things!
Specialists have expertise in gathering data relevant to their field, including:
✅ Specific historical information
✅ Specialized physical exam findings
✅ Outside records (hospitals, health department, etc)
And we go to their notes to find these things!
8/ 2⃣ Data INTERPRETATION:
But sometimes it's not new data we seek but rather a curation +/- interpretation of existing data, including:
✅ Lab tests
✅ Imaging
✅ Other reports (ex: EKGs, EGD/colonoscopy, etc.)
It's helpful when the relevant info is gathered in a single note!
But sometimes it's not new data we seek but rather a curation +/- interpretation of existing data, including:
✅ Lab tests
✅ Imaging
✅ Other reports (ex: EKGs, EGD/colonoscopy, etc.)
It's helpful when the relevant info is gathered in a single note!

9/ 3⃣ Data SYNTHESIS:
Although data listed in consultants' notes is often helpful, the MOST important part of the note is the assessment & recommendation.
So how should we structure them?
Although data listed in consultants' notes is often helpful, the MOST important part of the note is the assessment & recommendation.
So how should we structure them?
10/ Here are 2 key articles on the topic:
*⃣ pubmed.ncbi.nlm.nih.gov/19898909/
*⃣ pubmed.ncbi.nlm.nih.gov/17296883/
*⃣ pubmed.ncbi.nlm.nih.gov/19898909/
*⃣ pubmed.ncbi.nlm.nih.gov/17296883/

11/ These studies surveyed primary teams re: consult preferences.
There were some differences between surgical & non-surgical teams, but most agreed that notes should:
✅ Be concise
✅ Describe decision-making rationale
✅ Indicate importance & urgency of recs
There were some differences between surgical & non-surgical teams, but most agreed that notes should:
✅ Be concise
✅ Describe decision-making rationale
✅ Indicate importance & urgency of recs
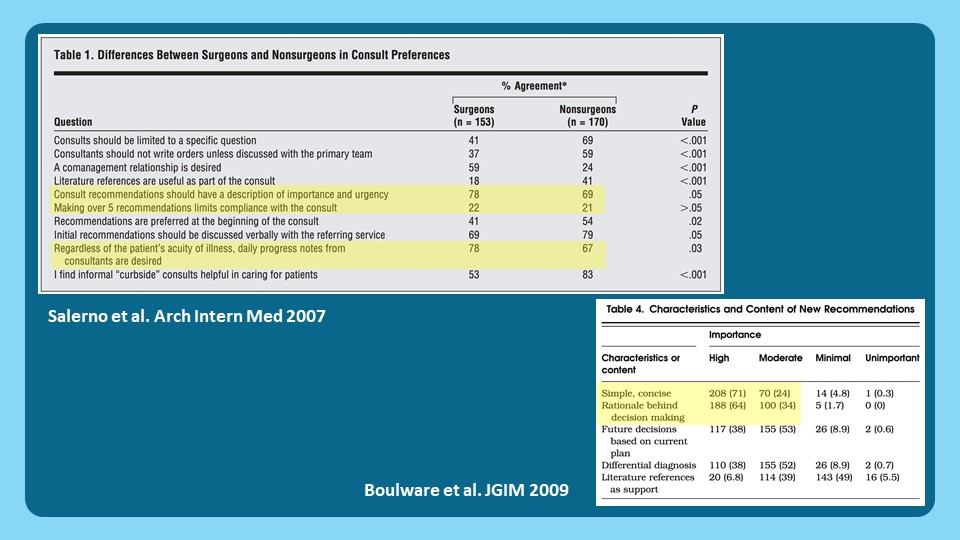
12/ Importantly, most did NOT care about:
📌 Limiting # of recommendations
📌 Including references
📌 Limiting # of recommendations
📌 Including references
13/ Based on this data, we should probably teach 3 important aspects of the data synthesis (i.e., "assessment & recommendations"):
1⃣ Synthesis - description of patient's problem with ddx
2⃣ Recommendations - clear, concise, specific
3⃣ Structure - well-organized, easy-to-read
1⃣ Synthesis - description of patient's problem with ddx
2⃣ Recommendations - clear, concise, specific
3⃣ Structure - well-organized, easy-to-read

14/ So how can we teach our learners, esp those new to a consult team, how to write effective notes?
I've summarized some strategies in the table below.
Two keys to doing this effectively:
🗝️ Providing explicit guidance
🗝️ Practicing what we 🗣️
I've summarized some strategies in the table below.
Two keys to doing this effectively:
🗝️ Providing explicit guidance
🗝️ Practicing what we 🗣️

15/ Next week @VarunPhadke2 will continue this series on "Teaching Consultant Skills" with ”Dealing with Conflict” ...
...including in our notes!
Remember to check out #SubspecialtyTeaching @MedEdTwagTeam to find all our threads in one place!
...including in our notes!
Remember to check out #SubspecialtyTeaching @MedEdTwagTeam to find all our threads in one place!

• • •
Missing some Tweet in this thread? You can try to
force a refresh