1/
9am. Consults.
Them: “We want you on board because ____ is 'refusing' to do this procedure but ____ says it's needed. You're the tiebreaker.”
You: [sigh] “OK.”
⌛️
Patient: “Ah! ____ said YOU'RE the one holding up my discharge!”
You: 🙄
Feeling triggered yet?
This week:
9am. Consults.
Them: “We want you on board because ____ is 'refusing' to do this procedure but ____ says it's needed. You're the tiebreaker.”
You: [sigh] “OK.”
⌛️
Patient: “Ah! ____ said YOU'RE the one holding up my discharge!”
You: 🙄
Feeling triggered yet?
This week:

2/
Conflict is inevitable when working within a system.
What do I mean when I say “conflict”? 🤔 For the purposes of this 🧵 let me paraphrase a huge body of literature w/ the following definition:
Conflict is “disagreement” that causes (or has the potential to cause) “harm”.
Conflict is inevitable when working within a system.
What do I mean when I say “conflict”? 🤔 For the purposes of this 🧵 let me paraphrase a huge body of literature w/ the following definition:
Conflict is “disagreement” that causes (or has the potential to cause) “harm”.
3/
Let's unpack this a bit more w/ a focus on conflict in consultative care.
"Disagreement" is a broad term.
It can stem from...
↪️ real OR perceived differences in opinion
↪️ about diagnosis OR management
↪️ between the primary team & the consultant OR between consultants
Let's unpack this a bit more w/ a focus on conflict in consultative care.
"Disagreement" is a broad term.
It can stem from...
↪️ real OR perceived differences in opinion
↪️ about diagnosis OR management
↪️ between the primary team & the consultant OR between consultants
4/
“Harm" is also a broad term.
It might mean...
🙅 damage to the inter-professional relationship
😩 internalized stress, aka burnout
👎 patient dissatisfaction
⛔️ medical error
“Harm" is also a broad term.
It might mean...
🙅 damage to the inter-professional relationship
😩 internalized stress, aka burnout
👎 patient dissatisfaction
⛔️ medical error
5/
Being able to recognize conflict is an essential skill for consultants because of our unique "invited" role in patient care. It influences how we communicate with patients, primary teams, & other consultants.
What are some signs of "conflict"?
Here’s a non-exhaustive list:
Being able to recognize conflict is an essential skill for consultants because of our unique "invited" role in patient care. It influences how we communicate with patients, primary teams, & other consultants.
What are some signs of "conflict"?
Here’s a non-exhaustive list:

6/
Even though we all experience conflict, few of us receive training in "conflict resolution."
One well-known framework (see figure) organizes strategies for conflict resolution based on how much value you place on your goals vs. those of the other party/the relationship.
Even though we all experience conflict, few of us receive training in "conflict resolution."
One well-known framework (see figure) organizes strategies for conflict resolution based on how much value you place on your goals vs. those of the other party/the relationship.

7/
While this scheme DESCRIBES the approaches that might unfold in an established conflict, our goal as teachers is to model/cultivate specific techniques to AVOID and MITIGATE conflict.
To do so, we need to have a framework for WHY conflict happens.
While this scheme DESCRIBES the approaches that might unfold in an established conflict, our goal as teachers is to model/cultivate specific techniques to AVOID and MITIGATE conflict.
To do so, we need to have a framework for WHY conflict happens.
8/
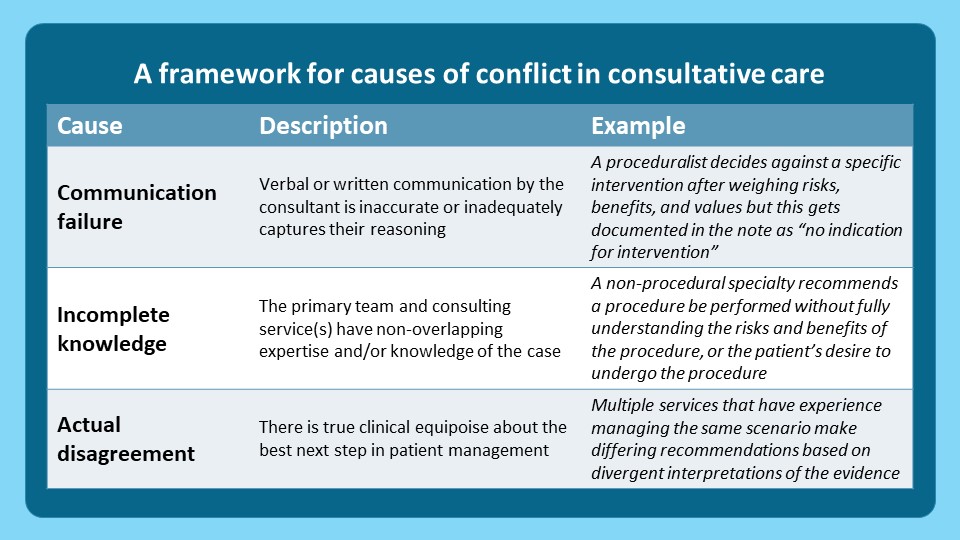
Here's how I organize the reasons why conflict arises in consultative care:
1⃣ Communication failure (written or verbal)
2⃣ Incomplete knowledge (+/- lack of humility)
3⃣ Actual disagreement (arising from true equipoise in diagnosis or management)
Here's how I organize the reasons why conflict arises in consultative care:
1⃣ Communication failure (written or verbal)
2⃣ Incomplete knowledge (+/- lack of humility)
3⃣ Actual disagreement (arising from true equipoise in diagnosis or management)
9/
Three key points about this framework:
🌟 The causes are in this order based on frequency (my opinion)
🌟 Strategies to avoid/mitigate conflict must be tailored to the specific cause
🌟 Conflict can occur WITHOUT actual disagreement!
Let's tackle these one-by-one.
Three key points about this framework:
🌟 The causes are in this order based on frequency (my opinion)
🌟 Strategies to avoid/mitigate conflict must be tailored to the specific cause
🌟 Conflict can occur WITHOUT actual disagreement!
Let's tackle these one-by-one.
10/
1⃣ Communication failure
This may be THE most common cause of conflict in consultation.
Communication failures can occur in written notes or verbal interactions.
Importantly, communication failures can lead to conflict even when NO disagreement exists!
1⃣ Communication failure
This may be THE most common cause of conflict in consultation.
Communication failures can occur in written notes or verbal interactions.
Importantly, communication failures can lead to conflict even when NO disagreement exists!

11/
These problems are often the most burnout-inducing causes of conflict.
Undoing bad games of "telephone", abrasive verbal or written recs, or unclear patient interactions is exhausting.
And all this can happen without ANY actual disagreement between the parties involved 😲
These problems are often the most burnout-inducing causes of conflict.
Undoing bad games of "telephone", abrasive verbal or written recs, or unclear patient interactions is exhausting.
And all this can happen without ANY actual disagreement between the parties involved 😲
12/
So, how do we mitigate/avoid these issues?
First, communication failures must be addressed in REAL-TIME.
Second, coaching strategies must emphasize SPECIFIC skills, like:
-describing reasoning in notes
-delivering 'unpalatable' recs
-discussing uncertainty w/ patients
So, how do we mitigate/avoid these issues?
First, communication failures must be addressed in REAL-TIME.
Second, coaching strategies must emphasize SPECIFIC skills, like:
-describing reasoning in notes
-delivering 'unpalatable' recs
-discussing uncertainty w/ patients

13/
2⃣ Incomplete knowledge
Even when communication is clear, consultants may not appreciate the unique knowledge/perspective that others have about a case/decision.
If this translates into recs that don’t align with the thoughts/values/goals of others, it can cause conflict.
2⃣ Incomplete knowledge
Even when communication is clear, consultants may not appreciate the unique knowledge/perspective that others have about a case/decision.
If this translates into recs that don’t align with the thoughts/values/goals of others, it can cause conflict.
14/
What might a consultant not fully grasp when "parachuting" into a case?
*⃣ Aspects of the "situation" that are more accessible to those w/ different content expertise or w/ a longitudinal patient relationship
*⃣ Aspects of the "options" that are the subject of disagreement
What might a consultant not fully grasp when "parachuting" into a case?
*⃣ Aspects of the "situation" that are more accessible to those w/ different content expertise or w/ a longitudinal patient relationship
*⃣ Aspects of the "options" that are the subject of disagreement

15/
How do we manage this?
Specialty learners must be COACHED on how to dialogue w/ others in a way that explores other perspectives meaningfully while also asserting their own unique expertise.
@WrayCharles et al. shared one fantastic framework in their "The Art of the Deal."
How do we manage this?
Specialty learners must be COACHED on how to dialogue w/ others in a way that explores other perspectives meaningfully while also asserting their own unique expertise.
@WrayCharles et al. shared one fantastic framework in their "The Art of the Deal."

16/
3⃣ Actual disagreement
Sometimes even w/ clear communication AND shared understanding of the situation, consultants disagree. Many clinical dilemmas have >1 acceptable solution, others have none.
But, this disagreement need not ⏩ conflict.
How can we avoid/mitigate it?
3⃣ Actual disagreement
Sometimes even w/ clear communication AND shared understanding of the situation, consultants disagree. Many clinical dilemmas have >1 acceptable solution, others have none.
But, this disagreement need not ⏩ conflict.
How can we avoid/mitigate it?
17/
Like other domains where high-stakes decisions that are vulnerable to bias must be made, CONSENSUS is 🗝️.
In these cases, clinical teachers should model:
✔️ Multi-disciplinary conversations
✔️ Sharing of perceived/real doubts
✔️ Patient-inclusive discussions of uncertainty
Like other domains where high-stakes decisions that are vulnerable to bias must be made, CONSENSUS is 🗝️.
In these cases, clinical teachers should model:
✔️ Multi-disciplinary conversations
✔️ Sharing of perceived/real doubts
✔️ Patient-inclusive discussions of uncertainty

18/
Okay, let’s recap.
In this 🧵 we learned:
🌟 Conflict in consultation manifests in many ways
🌟 Causes of conflict include communication failures, incomplete knowledge, or actual clinical equipoise
🌟 Strategies to build conflict resolution skills should address each cause
Okay, let’s recap.
In this 🧵 we learned:
🌟 Conflict in consultation manifests in many ways
🌟 Causes of conflict include communication failures, incomplete knowledge, or actual clinical equipoise
🌟 Strategies to build conflict resolution skills should address each cause
19/
Next week @JenniferSpicer4 will continue this series and kick off our segment on “Teaching the Consult Team” w/ “Teaching Multi-Level Learners.”
Remember to check out #SubspecialtyTeaching @MedEdTwagTeam to keep up with all our threads in one place!
See you next week!
Next week @JenniferSpicer4 will continue this series and kick off our segment on “Teaching the Consult Team” w/ “Teaching Multi-Level Learners.”
Remember to check out #SubspecialtyTeaching @MedEdTwagTeam to keep up with all our threads in one place!
See you next week!

• • •
Missing some Tweet in this thread? You can try to
force a refresh