1/4
#GI #GIbleed #urea
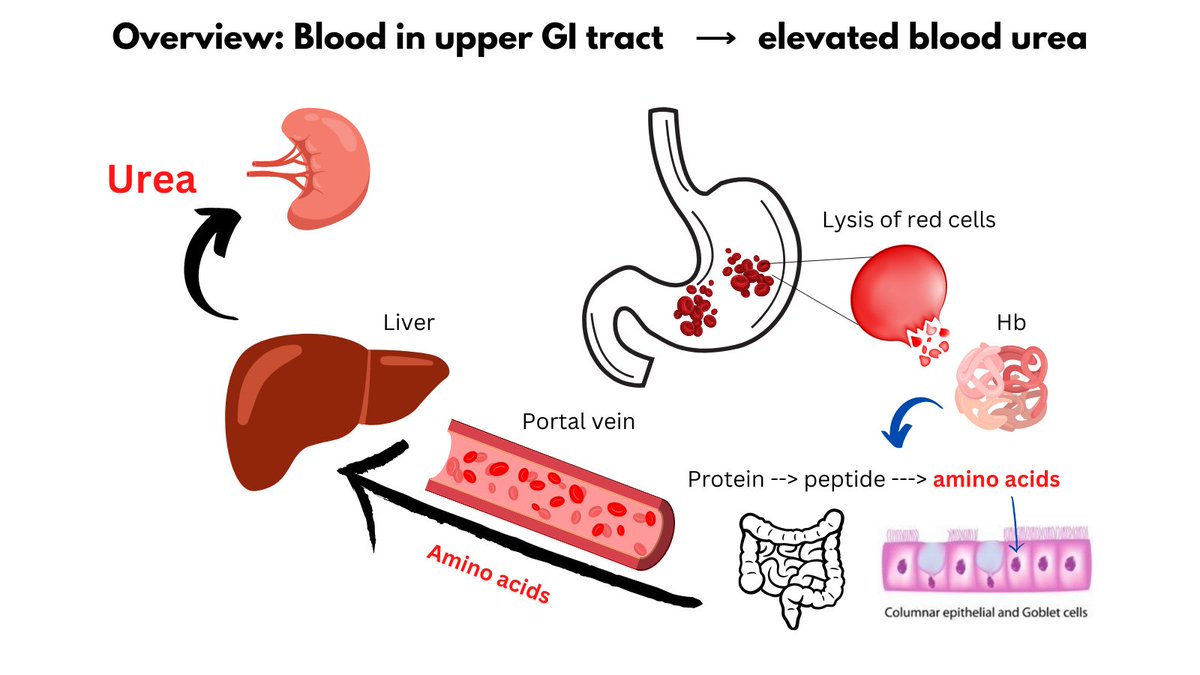
Elevated BUN: creatinine ratio favors UPPER over lower GI bleed.
Why?
1) Hb in stomach --> amino acids (aa).
2) aa absorbed by small intestine.
3) aa transported and taken up by liver.
4) In the liver, aa undergo deamination, leading to release of NH3.
#GI #GIbleed #urea
Elevated BUN: creatinine ratio favors UPPER over lower GI bleed.
Why?
1) Hb in stomach --> amino acids (aa).
2) aa absorbed by small intestine.
3) aa transported and taken up by liver.
4) In the liver, aa undergo deamination, leading to release of NH3.
2/4
5) NH3 (aka ammonia) is converted to urea by the urea cycle, leading to elevated blood urea levels.
6) Meantime, creatinine is not influenced by the protein/aa bolus.
7) Thus, BUN/creatinine ratio is increased.
5) NH3 (aka ammonia) is converted to urea by the urea cycle, leading to elevated blood urea levels.
6) Meantime, creatinine is not influenced by the protein/aa bolus.
7) Thus, BUN/creatinine ratio is increased.
3/4
So why does blood cause this bump in urea and increase in BUN/creatinine ratio, whereas a steak dinner does not?
Because blood has poor BIOLOGICAL VALIUE (the protein is poorly utilized by the body).
The LOWER the biological value of a protein, the HIGHER the urea.
So why does blood cause this bump in urea and increase in BUN/creatinine ratio, whereas a steak dinner does not?
Because blood has poor BIOLOGICAL VALIUE (the protein is poorly utilized by the body).
The LOWER the biological value of a protein, the HIGHER the urea.
• • •
Missing some Tweet in this thread? You can try to
force a refresh