1/
2pm. Usual day on ID consults.
Learner: “So the patient had [complex multi-stage procedure w/ prosthetic material] yesterday. Turns out they were bacteremic.”
You: "and...?"
Learner: "They want antibiotic recs...I'm not sure how to approach that..."
You: 🤷
This week:
2pm. Usual day on ID consults.
Learner: “So the patient had [complex multi-stage procedure w/ prosthetic material] yesterday. Turns out they were bacteremic.”
You: "and...?"
Learner: "They want antibiotic recs...I'm not sure how to approach that..."
You: 🤷
This week:

2/
Consultants are often called upon for input on management.
Typically, this means helping with a clinical decision (which test? which treatment?).
Management reasoning refers to the cognitive processes by which clinicians make those decisions.
pubmed.ncbi.nlm.nih.gov/29800012/
Consultants are often called upon for input on management.
Typically, this means helping with a clinical decision (which test? which treatment?).
Management reasoning refers to the cognitive processes by which clinicians make those decisions.
pubmed.ncbi.nlm.nih.gov/29800012/
3/
Teaching & assessing clinical decision-making skills is HARD.
Without a framework for the cognitive processes involved, it can be challenging to isolate the specific skills a learner needs to work on.
This leads to unhelpful feedback like "lacks confidence" (which = 🤷).
Teaching & assessing clinical decision-making skills is HARD.
Without a framework for the cognitive processes involved, it can be challenging to isolate the specific skills a learner needs to work on.
This leads to unhelpful feedback like "lacks confidence" (which = 🤷).
4/
Fortunately, there's been an explosion of helpful publications & other resources over the past few years w/ specific tips on teaching management reasoning.
I’ve highlighted a few here.
I have drawn on these & many others to craft this thread, & added some of my own pearls.
Fortunately, there's been an explosion of helpful publications & other resources over the past few years w/ specific tips on teaching management reasoning.
I’ve highlighted a few here.
I have drawn on these & many others to craft this thread, & added some of my own pearls.

5/
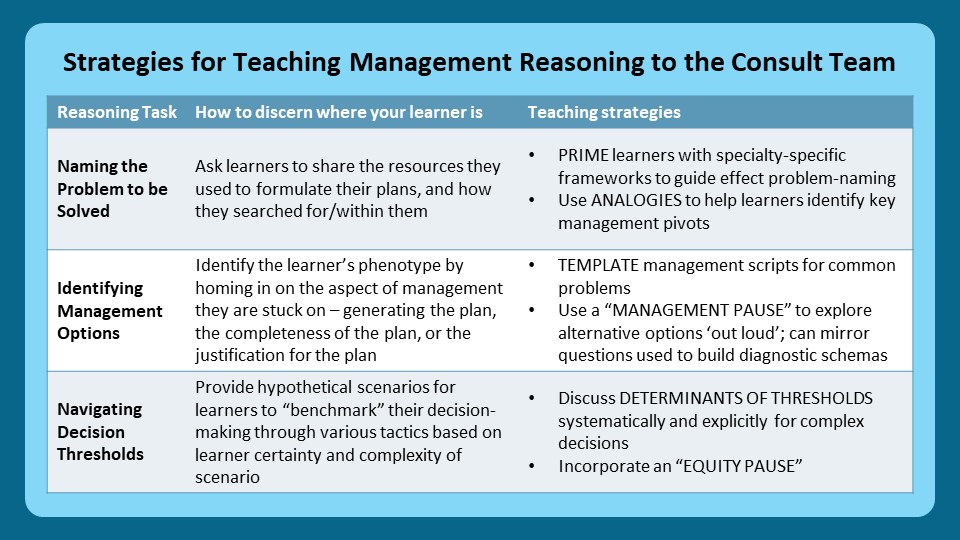
For this 🧵 I'll be discussing just three skills that I’ve extracted from this framework of management reasoning (one that is still being refined):
1⃣ Naming a problem to be solved
2⃣ Identifying management options
3⃣ Navigating decision thresholds
pubmed.ncbi.nlm.nih.gov/35830267/
For this 🧵 I'll be discussing just three skills that I’ve extracted from this framework of management reasoning (one that is still being refined):
1⃣ Naming a problem to be solved
2⃣ Identifying management options
3⃣ Navigating decision thresholds
pubmed.ncbi.nlm.nih.gov/35830267/
6/
For each skill, I hope to address some practical issues faced by clinical teachers, with a focus on consult services.
📌 Are there unique considerations for specialists?
📌 What can I do to figure out where my learner is?
📌 How do I teach this skill?
Let’s get started!
For each skill, I hope to address some practical issues faced by clinical teachers, with a focus on consult services.
📌 Are there unique considerations for specialists?
📌 What can I do to figure out where my learner is?
📌 How do I teach this skill?
Let’s get started!
7/
1⃣ "Naming a problem to be solved"
Learners on consult teams struggle w/ this for two reasons:
a. They are unfamiliar w/ the problems/syndromes that ought to trigger action
b. The problem/syndrome is one for which no established action plan exists (reason for consult!) 😱
1⃣ "Naming a problem to be solved"
Learners on consult teams struggle w/ this for two reasons:
a. They are unfamiliar w/ the problems/syndromes that ought to trigger action
b. The problem/syndrome is one for which no established action plan exists (reason for consult!) 😱

8/
These issues have different solutions.
Less experienced learners should be primed w/ relevant resources *as soon as the consult ask becomes clear* (not after their assessment!).
This helps them formulate an actionable diagnostic label for the case.
These issues have different solutions.
Less experienced learners should be primed w/ relevant resources *as soon as the consult ask becomes clear* (not after their assessment!).
This helps them formulate an actionable diagnostic label for the case.
https://twitter.com/JenniferSpicer4/status/1592571825074343937?s=20&t=7Id8zPEr4_x44nTRtMhWdQ
9/
What about when learners name problems for which no established ("google-able”) solution exists?
This happens a lot on consults because so many decisions are left to “expert opinion".
Here we can help learners ‘reason’ their way to appropriate management using analogies.
What about when learners name problems for which no established ("google-able”) solution exists?
This happens a lot on consults because so many decisions are left to “expert opinion".
Here we can help learners ‘reason’ their way to appropriate management using analogies.

10/
2⃣ “Identifying management options”
Once a "problem" has been established, clinicians need to be able to generate a menu of potential management options.
This pre-compiled list of actions activated by a working diagnosis is a management script.
pubmed.ncbi.nlm.nih.gov/32349018/
2⃣ “Identifying management options”
Once a "problem" has been established, clinicians need to be able to generate a menu of potential management options.
This pre-compiled list of actions activated by a working diagnosis is a management script.
pubmed.ncbi.nlm.nih.gov/32349018/
11/
Learners may struggle here in many ways:
a. Not being able to articulate a script ("what SHOULD you do...")
b. Not having a fully developed script ("what ELSE should you do...")
c. Not having multiple scripts to compare/contrast & select from ("what else COULD you do...")
Learners may struggle here in many ways:
a. Not being able to articulate a script ("what SHOULD you do...")
b. Not having a fully developed script ("what ELSE should you do...")
c. Not having multiple scripts to compare/contrast & select from ("what else COULD you do...")

12/
@EmilyAbdoler @andrewparsonsMD @thilanMD & @JRencic have shared some strategies for tackling these issues.
For example:
📐 Templating - to ensure completeness of management scripts
⏸️ The 'management pause' - to explore alternatives "out loud"
pubmed.ncbi.nlm.nih.gov/36420532/
@EmilyAbdoler @andrewparsonsMD @thilanMD & @JRencic have shared some strategies for tackling these issues.
For example:
📐 Templating - to ensure completeness of management scripts
⏸️ The 'management pause' - to explore alternatives "out loud"
pubmed.ncbi.nlm.nih.gov/36420532/
13/
Now go back to tweet #11 in this 🧵. Does it remind you of anything? Yes, it’s a schema!
This was entirely deliberate.
I’ve found it can be helpful to teach management scripts on-the-fly using the same strategies I use to build diagnostic schemas on-the-fly!
Check it out!
Now go back to tweet #11 in this 🧵. Does it remind you of anything? Yes, it’s a schema!
This was entirely deliberate.
I’ve found it can be helpful to teach management scripts on-the-fly using the same strategies I use to build diagnostic schemas on-the-fly!
Check it out!

14/
3⃣ “Navigating decision thresholds"
This is my favorite part of management reasoning to teach about.
And it's particularly important on consult services where many management decisions are shaped by the varying thresholds of the consultant, primary team, patient, & system.
3⃣ “Navigating decision thresholds"
This is my favorite part of management reasoning to teach about.
And it's particularly important on consult services where many management decisions are shaped by the varying thresholds of the consultant, primary team, patient, & system.
15/
A decision threshold is the point at which a clinician perceives they have enough info to take an action (ex perform a test, start Rx).
How high/low their threshold is for taking that action depends on many factors, which may be internal/external to the action or clinician.
A decision threshold is the point at which a clinician perceives they have enough info to take an action (ex perform a test, start Rx).
How high/low their threshold is for taking that action depends on many factors, which may be internal/external to the action or clinician.
16/
How can we elicit the [usually implicit] thresholds that are guiding a learner's decision-making?
Three strategies I use routinely:
*⃣ Progressive problem-solving (h/t to @Gurpreet2015)
*⃣ The "spectrum of anxiety"
*⃣ "Shoot down my crazy idea"
How can we elicit the [usually implicit] thresholds that are guiding a learner's decision-making?
Three strategies I use routinely:
*⃣ Progressive problem-solving (h/t to @Gurpreet2015)
*⃣ The "spectrum of anxiety"
*⃣ "Shoot down my crazy idea"

17/
The unifying concept underlying all three of these approaches is to provide learners w/ hypothetical scenarios which they can use to "benchmark" their decision-making.
Ideally such “reps” occur organically through clinical exposure.
But they don’t. So we need to improvise.
The unifying concept underlying all three of these approaches is to provide learners w/ hypothetical scenarios which they can use to "benchmark" their decision-making.
Ideally such “reps” occur organically through clinical exposure.
But they don’t. So we need to improvise.
18/
How can we make learners more aware of the factors that influence decision-making?
By thinking through those factors systematically (see Table).
@EmilyAbdoler @andrewparsonsMD & @thilanMD also described an "equity reflection" to help mitigate bias.
pubmed.ncbi.nlm.nih.gov/36420532/
How can we make learners more aware of the factors that influence decision-making?
By thinking through those factors systematically (see Table).
@EmilyAbdoler @andrewparsonsMD & @thilanMD also described an "equity reflection" to help mitigate bias.
pubmed.ncbi.nlm.nih.gov/36420532/

19/
Let's recap:
In this 🧵 we:
📌 Dissected three elements of the management reasoning process w/ a focus on consultants
📌 Described tactics to “surface” the cognitive processes underlying learners’ decision-making
📌 Identified teaching strategies to build those skills
Let's recap:
In this 🧵 we:
📌 Dissected three elements of the management reasoning process w/ a focus on consultants
📌 Described tactics to “surface” the cognitive processes underlying learners’ decision-making
📌 Identified teaching strategies to build those skills
20/
Next week @JenniferSpicer4 will pick up a new series on “Teaching the Primary Team” focusing on “The Why”.
Remember to check out #SubspecialtyTeaching @MedEdTwagTeam & follow @YihanYangMD @GStetsonMD @ChrisDJacksonMD to keep up with all our threads!
See you next week!
Next week @JenniferSpicer4 will pick up a new series on “Teaching the Primary Team” focusing on “The Why”.
Remember to check out #SubspecialtyTeaching @MedEdTwagTeam & follow @YihanYangMD @GStetsonMD @ChrisDJacksonMD to keep up with all our threads!
See you next week!

• • •
Missing some Tweet in this thread? You can try to
force a refresh