New mask thread. Addresses
- Why so much controversy?
- Airborne transmission
- RCTs of masks - strengths/weaknesses, community, healthcare settings
- Meta-analyses - gold standard or lazy lumping?
- Non-RCT evidence - why is it needed, what does it show?
- AOB
1.
- Why so much controversy?
- Airborne transmission
- RCTs of masks - strengths/weaknesses, community, healthcare settings
- Meta-analyses - gold standard or lazy lumping?
- Non-RCT evidence - why is it needed, what does it show?
- AOB
1.
2.Before I start, here’s the OLD mask thread from July 21, which ran to >100 tweets. Some of that is now rather dated but a lot still holds. I’ll paste the best old tweets into this new thread.
https://twitter.com/trishgreenhalgh/status/1414294003479089154?s=20
3.WHY IS MASKING SO CONTROVERSIAL?
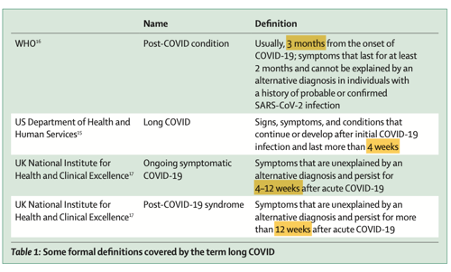
First, ‘masks’ and ‘masking’ are very broad terms. They cover different technologies (cloth, medical, respirator), wearers (public, patient, healthcare worker), settings (low v high risk) and requirements (mandated v free choice).


First, ‘masks’ and ‘masking’ are very broad terms. They cover different technologies (cloth, medical, respirator), wearers (public, patient, healthcare worker), settings (low v high risk) and requirements (mandated v free choice).



4. WHY CONTROVERSIAL?
Because of this multiplicity, statements like “masks [don't] work” may be referring to very different interventions in different populations for different activities at different times, not to mention different diseases. The literature, in short, is a mess.
Because of this multiplicity, statements like “masks [don't] work” may be referring to very different interventions in different populations for different activities at different times, not to mention different diseases. The literature, in short, is a mess.
5.WHY CONTROVERSIAL?
Second, masking is a cultural practice as well as a public health intervention. It has symbolic meaning. Pirates and burglars wear masks. To some, masking means you’re a ‘pansy’, ‘sheep’ etc. Masking offends libertarians.
bmj.com/content/370/bm…
Second, masking is a cultural practice as well as a public health intervention. It has symbolic meaning. Pirates and burglars wear masks. To some, masking means you’re a ‘pansy’, ‘sheep’ etc. Masking offends libertarians.
bmj.com/content/370/bm…
6. WHY CONTROVERSIAL?
There’s strong social pressure to mask to contribute to the greater good (“my mask protects you”). People may feel pushed into doing something which a) feels awkward, b) symbolises an allegiance they don’t identify with and c) they feel is ineffective.
There’s strong social pressure to mask to contribute to the greater good (“my mask protects you”). People may feel pushed into doing something which a) feels awkward, b) symbolises an allegiance they don’t identify with and c) they feel is ineffective.

7.WHY CONTROVERSIAL?
Third, masking (whatever its benefits) has downsides. It’s (depending on the design) uncomfortable. It can interfere with communication (especially if hard of hearing). If you work long shifts, it gets hot & sweaty behind the mask.
bmj.com/content/370/bm…
Third, masking (whatever its benefits) has downsides. It’s (depending on the design) uncomfortable. It can interfere with communication (especially if hard of hearing). If you work long shifts, it gets hot & sweaty behind the mask.
bmj.com/content/370/bm…
8.WHY CONTROVERSIAL?
In short, masking is something many of us feel strongly about. It’s not even possible to separate “the science” of masks from “the politics”, since science does not sit in some protected bubble away from the rest of society. Read on!
In short, masking is something many of us feel strongly about. It’s not even possible to separate “the science” of masks from “the politics”, since science does not sit in some protected bubble away from the rest of society. Read on!
9. AIRBORNE TRANSMISSION
Understanding why & to what extent masks work requires knowledge of how the SARS-CoV-2 virus is transmitted. With colleagues, I published a summary of evidence that it spreads *predominantly* through the air. Thread + paper here
Understanding why & to what extent masks work requires knowledge of how the SARS-CoV-2 virus is transmitted. With colleagues, I published a summary of evidence that it spreads *predominantly* through the air. Thread + paper here
https://twitter.com/trishgreenhalgh/status/1389204113032876032?s=20
10. AIRBORNE TRANSMISSION
I responded to critics of that paper here
I responded to critics of that paper here
https://twitter.com/trishgreenhalgh/status/1385878084063219713?s=20&t=_Gj92tVyztw7cQb6S1pJiA(plus see more in thread below).
11.AIRBORNE TRANSMISSION
For those who want depth and detail, here’s Chia Wang and team’s stunning review of the evidence for airborne transmission in Science (one of the very top scientific journals).
science.org/doi/abs/10.112…
For those who want depth and detail, here’s Chia Wang and team’s stunning review of the evidence for airborne transmission in Science (one of the very top scientific journals).
science.org/doi/abs/10.112…
12.AIRBORNE TRANSMISSION
In sum, it's *settled science* that SARS-CoV-2 is transmitted via the air. Settled, that is, in all branches of science *except* key groups of doctors, including some in powerful positions at the World Health Organisation. I return to that paradox below.
In sum, it's *settled science* that SARS-CoV-2 is transmitted via the air. Settled, that is, in all branches of science *except* key groups of doctors, including some in powerful positions at the World Health Organisation. I return to that paradox below.
13. AIRBORNE TRANSMISSION
Medical/surgical (~same thing) masks are designed to stop spatter (e.g. your dentist dribbling into your mouth). Most aren’t made to a specific quality standard. Respirators are designed to filter out airborne particles. They ARE made to a standard.
Medical/surgical (~same thing) masks are designed to stop spatter (e.g. your dentist dribbling into your mouth). Most aren’t made to a specific quality standard. Respirators are designed to filter out airborne particles. They ARE made to a standard.
14.AIRBORNE TRANSMISSION
If SARS-CoV-2 were spread mainly by droplets, we’d need to focus on handwashing and med/surg masks which stop wet drops. If mainly via air, we need to focus on air quality and use the kind of face coverings that stop airborne particles (ie. respirators)
If SARS-CoV-2 were spread mainly by droplets, we’d need to focus on handwashing and med/surg masks which stop wet drops. If mainly via air, we need to focus on air quality and use the kind of face coverings that stop airborne particles (ie. respirators)
15.AIRBORNE TRANSMISSION
All masks stop some airborne particles (even if the holes are bigger than the particles, fibres are criss-crossed and electrostatic forces kick in). But N95 (FFP2) respirators stop >95% of particles of SARS-CoV-2 size, and N99s (FFP3s) stop >99%.
All masks stop some airborne particles (even if the holes are bigger than the particles, fibres are criss-crossed and electrostatic forces kick in). But N95 (FFP2) respirators stop >95% of particles of SARS-CoV-2 size, and N99s (FFP3s) stop >99%.
16. AIRBORNE TRANSMISSION
A year ago, we wrote this article recommending that everyone upgrades their mask from either medical/surgical to respirator.
theconversation.com/time-to-upgrad…
A year ago, we wrote this article recommending that everyone upgrades their mask from either medical/surgical to respirator.
theconversation.com/time-to-upgrad…
17.AIRBORNE TRANSMISSION
Whilst respirators protect best, ANY mask is better than none. Efficiency at reducing transmission of an artificial respiratory aerosol:
N95 respirator 99%
Medical mask 59%
Bandana (single) 47% (double) 60%
Face shield 2%
tandfonline.com/doi/full/10.10……
Whilst respirators protect best, ANY mask is better than none. Efficiency at reducing transmission of an artificial respiratory aerosol:
N95 respirator 99%
Medical mask 59%
Bandana (single) 47% (double) 60%
Face shield 2%
tandfonline.com/doi/full/10.10……
18. AIRBORNE TRANSMISSION
The above, a laboratory study of artificial aerosols, should not be taken as direct evidence that these masks would be this effective/ineffective in preventing real-world SARS-CoV-2 transmission. But they *add to the mix of evidence*. More on that later
The above, a laboratory study of artificial aerosols, should not be taken as direct evidence that these masks would be this effective/ineffective in preventing real-world SARS-CoV-2 transmission. But they *add to the mix of evidence*. More on that later
19.AIRBORNE TRANSMISSION
Face shields are only 2% effective cos they’re designed to stop spatter NOT filter air. Medical masks don’t fit snugly, so instead of breathing filtered air, you breathe what leaks in round the sides. This is why a doubled-over bandana works pretty well!
Face shields are only 2% effective cos they’re designed to stop spatter NOT filter air. Medical masks don’t fit snugly, so instead of breathing filtered air, you breathe what leaks in round the sides. This is why a doubled-over bandana works pretty well!
20. AIRBORNE TRANSMISSION
While I believe that cloth & medical masks have an important place (better than nothing), some scholars (Lisa Brosseau is one) feel that the benefits of respirators are so much greater, we should junk all lesser kinds of masking.
cidrap.umn.edu/covid-19/comme…
While I believe that cloth & medical masks have an important place (better than nothing), some scholars (Lisa Brosseau is one) feel that the benefits of respirators are so much greater, we should junk all lesser kinds of masking.
cidrap.umn.edu/covid-19/comme…
21. AIRBORNE TRANSMISSION
Remember, respirators (and masks) only work if they fit you snugly. You don’t need a professional fitting any more than you need to have your underwear professionally fitted, but do check for gaps.
Remember, respirators (and masks) only work if they fit you snugly. You don’t need a professional fitting any more than you need to have your underwear professionally fitted, but do check for gaps.
22. RANDOMISED CONTROLLED TRIALS (RCTs) OF MASKS
RCTs of masks have continued to generate more heat than light. I’m going to reproduce what I said 2 years ago, which still holds (even more so now, since what has happened since could have been predicted from my earlier thread).
RCTs of masks have continued to generate more heat than light. I’m going to reproduce what I said 2 years ago, which still holds (even more so now, since what has happened since could have been predicted from my earlier thread).
23. RCTs
In the name of evidence-based medicine (EBM), the West got off on the wrong foot. We became obsessed with the holy grail of a definitive randomised controlled trial (RCT) that would quantify both the benefits and the harms of masks, just as you would for a drug.
In the name of evidence-based medicine (EBM), the West got off on the wrong foot. We became obsessed with the holy grail of a definitive randomised controlled trial (RCT) that would quantify both the benefits and the harms of masks, just as you would for a drug.
24. RCTs
If you were raised in the EBM tradition, where “rigorous RCTs” are mother’s milk, it’s not easy to get your head round why this was a bad way to approach the problem. Looks like Prof G has lost it, dropped her standards, joined the dark side etc. Bear with me.
If you were raised in the EBM tradition, where “rigorous RCTs” are mother’s milk, it’s not easy to get your head round why this was a bad way to approach the problem. Looks like Prof G has lost it, dropped her standards, joined the dark side etc. Bear with me.
25. RCTs
A RCT is a controlled experiment. Since people are randomly allocated to one or other group (‘arm’), any confounding variables are distributed evenly between the arms so they all cancel out (so long as the study is large enough and allocation is truly random).
A RCT is a controlled experiment. Since people are randomly allocated to one or other group (‘arm’), any confounding variables are distributed evenly between the arms so they all cancel out (so long as the study is large enough and allocation is truly random).
26. RCTs
Random allocation means that differences between the arms of a RCT are highly likely to be due to the intervention (in this case, masks) and not to confounders. But it doesn’t follow that a RCT is better, for any scientific question, than a non-RCT design. Why not?
Random allocation means that differences between the arms of a RCT are highly likely to be due to the intervention (in this case, masks) and not to confounders. But it doesn’t follow that a RCT is better, for any scientific question, than a non-RCT design. Why not?
27. RCTs
Many reasons. Drugs are (arguably) a simple intervention, but masks are a highly complex one. There are two key questions: do they protect the wearer from other people’s germs – and do they protect other people from the wearer’s germs (‘source control’)?
Many reasons. Drugs are (arguably) a simple intervention, but masks are a highly complex one. There are two key questions: do they protect the wearer from other people’s germs – and do they protect other people from the wearer’s germs (‘source control’)?
28. RCTs
The RCT design can’t (usually) cope with this. It’s easy to design a study where the main outcome is infection in wearers, but how would a RCT of source control work? Answer: do an enormous study to randomise entire towns to either masking or not masking!
The RCT design can’t (usually) cope with this. It’s easy to design a study where the main outcome is infection in wearers, but how would a RCT of source control work? Answer: do an enormous study to randomise entire towns to either masking or not masking!
29. RCTs
Impressively, @jabaluk and team did just this. They randomised 600 villages in rural Bangladesh (over 300,000 people) to getting free masks (‘interventions’) or not (‘controls’). For 2 months, they observed mask-wearing and counted covid-19 cases in all villages.
Impressively, @jabaluk and team did just this. They randomised 600 villages in rural Bangladesh (over 300,000 people) to getting free masks (‘interventions’) or not (‘controls’). For 2 months, they observed mask-wearing and counted covid-19 cases in all villages.
30. RCTs
The Abaluk RCT was published in Science (really top-notch academic journal). It showed that in the intervention villages, a) mask wearing was three times as high as in the control villages, and b) incidence of covid-19 was lower.
science.org/doi/10.1126/sc…
The Abaluk RCT was published in Science (really top-notch academic journal). It showed that in the intervention villages, a) mask wearing was three times as high as in the control villages, and b) incidence of covid-19 was lower.
science.org/doi/10.1126/sc…
31. RCTs
Despite the large size of the Bangladesh RCT, differences in covid-19 incidence were relatively modest and only just reached statistical significance when measured by blood test. Differences were greater where surgical rather than cloth masks were used.
Despite the large size of the Bangladesh RCT, differences in covid-19 incidence were relatively modest and only just reached statistical significance when measured by blood test. Differences were greater where surgical rather than cloth masks were used.
32. RCTs
Does this mean “masks don’t work” in the community? NO! Looks like even in free-living conditions (people can choose not to wear), they have a modest but important effect—reducing transmission by ~10%. Let me return to some of the arguments I put out two years ago.
Does this mean “masks don’t work” in the community? NO! Looks like even in free-living conditions (people can choose not to wear), they have a modest but important effect—reducing transmission by ~10%. Let me return to some of the arguments I put out two years ago.
33. EXPONENTIAL SPREAD
For policy decisions, we’re not just interested in whether masking reduces community incidence of covid-19 in a short intervention period (say, a month or 2). We’re interested in how masking impacts on the *exponential spread* of an accelerating pandemic.
For policy decisions, we’re not just interested in whether masking reduces community incidence of covid-19 in a short intervention period (say, a month or 2). We’re interested in how masking impacts on the *exponential spread* of an accelerating pandemic.
34. EXPONENTIAL SPREAD
Take the number 1, double it, then keep going. 1 becomes 2, then 4, etc. After 10 doubles, you get 512. After 10 more doubles, 262144. Now instead of doubling, multiply by 1.9 (a tiny reduction in growth rate). After 20 cycles, the total is only 104127.
Take the number 1, double it, then keep going. 1 becomes 2, then 4, etc. After 10 doubles, you get 512. After 10 more doubles, 262144. Now instead of doubling, multiply by 1.9 (a tiny reduction in growth rate). After 20 cycles, the total is only 104127.
35.EXPONENTIAL SPREAD
=> if masks reduce transmission by a TINY bit (too tiny to be statistically significant in a short RCT), population benefits are still HUGE. If instead of doubling every 9 days, covid rates increased by 1.9, after 180 days total cases would be down by 60%.
=> if masks reduce transmission by a TINY bit (too tiny to be statistically significant in a short RCT), population benefits are still HUGE. If instead of doubling every 9 days, covid rates increased by 1.9, after 180 days total cases would be down by 60%.
36. WHY RCTS OFTEN MISLEAD
These two issues—the near-impossibility of using RCTs to test hypotheses about source control and over-reliance on “statistically significant effects” within a short intervention period—is why a RCT of masks is *highly likely to mislead us*.
These two issues—the near-impossibility of using RCTs to test hypotheses about source control and over-reliance on “statistically significant effects” within a short intervention period—is why a RCT of masks is *highly likely to mislead us*.
37.RCTs
Let’s look at the other large community-based RCT of masks in covid-19. The *big Danish mask trial* became one of the most talked-about RCTs in the pandemic. Its main finding was negative (no significant impact of masks compared to no masks).
acpjournals.org/doi/10.7326/M2…
Let’s look at the other large community-based RCT of masks in covid-19. The *big Danish mask trial* became one of the most talked-about RCTs in the pandemic. Its main finding was negative (no significant impact of masks compared to no masks).
acpjournals.org/doi/10.7326/M2…
38. RCTs
But the DANMASK RCT was *fatally flawed* as
@dgurdasani1
and I argued here. I’ll summarise in the next tweet. spectator.co.uk/article/eight-……
But the DANMASK RCT was *fatally flawed* as
@dgurdasani1
and I argued here. I’ll summarise in the next tweet. spectator.co.uk/article/eight-……
39. RCTs
DANMASK RCT flaws: no CONSORT statement, no ethical approval, inappropriate setting (there was almost no Covid circulating at the time!), under-powered sample, wrong primary outcome, wrong intervention period, inaccurate test, misinterpretation of own findings.
DANMASK RCT flaws: no CONSORT statement, no ethical approval, inappropriate setting (there was almost no Covid circulating at the time!), under-powered sample, wrong primary outcome, wrong intervention period, inaccurate test, misinterpretation of own findings.
40. RCTs
There *never will be* RCT evidence to definitively answer the question “do masks work in community settings?” because RCTs can’t generate dynamic evidence to understand complex social interventions in diverse and changing contexts. Answer will always be “to some extent”
There *never will be* RCT evidence to definitively answer the question “do masks work in community settings?” because RCTs can’t generate dynamic evidence to understand complex social interventions in diverse and changing contexts. Answer will always be “to some extent”
41. RCTs OF MASKS IN HEALTHCARE WORKERS (HCWs)
The question of how to protect HCWs is politically contentious, since it involves the sensitive topic of occupationally-acquired disease and the risk (in rare but well-described cases) of a HCW dying from covid-19 caught at work.
The question of how to protect HCWs is politically contentious, since it involves the sensitive topic of occupationally-acquired disease and the risk (in rare but well-described cases) of a HCW dying from covid-19 caught at work.
42. RCTs in HCWs
Broadly speaking, HCW unions want high-grade protection for their members; employers want to spend as little as possible on personal protective equipment (PPE). So RCTs comparing medical masks (cheap) with respirators (more expensive) have special significance.
Broadly speaking, HCW unions want high-grade protection for their members; employers want to spend as little as possible on personal protective equipment (PPE). So RCTs comparing medical masks (cheap) with respirators (more expensive) have special significance.
43. RCTs in HCWs
There’s been only one published peer-reviewed RCT of masking in HCWs during covid-19. Loeb et al did a 5-country study which showed no statistically significant difference between medical masks and respirators:
pubmed.ncbi.nlm.nih.gov/36442064/
There’s been only one published peer-reviewed RCT of masking in HCWs during covid-19. Loeb et al did a 5-country study which showed no statistically significant difference between medical masks and respirators:
pubmed.ncbi.nlm.nih.gov/36442064/
44. RCTs in HCWs
The Loeb study has been heavily criticised. I have two major concerns. First, according to the original study protocol, HCWs were asked to wear the mask/respirator “when providing routine care to patients with COVID-19 or suspected COVID-19”.
The Loeb study has been heavily criticised. I have two major concerns. First, according to the original study protocol, HCWs were asked to wear the mask/respirator “when providing routine care to patients with COVID-19 or suspected COVID-19”.
45. RCTs in HCWs
Because SARS-CoV-2 is airborne (see tweets 9-20), removing masks when not in the close vicinity of known or suspected covid patients is illogical. See why we need to understand the mode of transmission to interpret the studies?
Because SARS-CoV-2 is airborne (see tweets 9-20), removing masks when not in the close vicinity of known or suspected covid patients is illogical. See why we need to understand the mode of transmission to interpret the studies?
46. RCTs in HCWs
Even though the words quoted in tweet 42 are taken directly from their participant information sheets, Loeb and colleagues say that participants were “expected” to wear their mask or respirator all the time when at work.
Even though the words quoted in tweet 42 are taken directly from their participant information sheets, Loeb and colleagues say that participants were “expected” to wear their mask or respirator all the time when at work.
47. RCTs in HCWs
There is confusion about which participants wore what and when in the Loeb RCT. This may not be entirely the authors’ fault, as the study was occurring in a changing policy context (universal masking of HCWs came and went in some sites as the trial progressed).
There is confusion about which participants wore what and when in the Loeb RCT. This may not be entirely the authors’ fault, as the study was occurring in a changing policy context (universal masking of HCWs came and went in some sites as the trial progressed).
48. RCTs in HCWs
My other concern with the Loeb RCT is that results are heavily skewed by data from Egypt, the largest national subsample. There was a big wave of Omicron in Egypt at the time, so HCWs in both arms could well have caught the virus outside work.
My other concern with the Loeb RCT is that results are heavily skewed by data from Egypt, the largest national subsample. There was a big wave of Omicron in Egypt at the time, so HCWs in both arms could well have caught the virus outside work.
49. RCTs in HCWs
Even if Egyptian HCWs wore their protection all the time at work, if they then went home and played with their infected kids, they’d be as likely to catch covid as anyone else. Egypt was the only country where *more* infections occurred in the respirator arm!
Even if Egyptian HCWs wore their protection all the time at work, if they then went home and played with their infected kids, they’d be as likely to catch covid as anyone else. Egypt was the only country where *more* infections occurred in the respirator arm!
50. RCTs in HCWs
Loeb et al are currently responding to these and other methodological criticisms. ONE explanation for their findings is that respirators are no more effective than medical masks. Another is that a benefit exists but this trial failed to demonstrate it.
Loeb et al are currently responding to these and other methodological criticisms. ONE explanation for their findings is that respirators are no more effective than medical masks. Another is that a benefit exists but this trial failed to demonstrate it.
51. COCHRANE REVIEW OF MASK RCTs
You may have seen the headlines in the last couple of weeks, that a ‘Cochrane review’ has demonstrated the lack of RCT evidence for efficacy of masks. Here’s the review so you know what I’m criticising. I don’t endorse it.
cochranelibrary.com/cdsr/doi/10.10…
You may have seen the headlines in the last couple of weeks, that a ‘Cochrane review’ has demonstrated the lack of RCT evidence for efficacy of masks. Here’s the review so you know what I’m criticising. I don’t endorse it.
cochranelibrary.com/cdsr/doi/10.10…
52. COCHRANE REVIEW
Despite widespread claims that this new meta-analysis (actually, an update of an old meta-analysis) has definitively demonstrated that “masks don’t work” in reducing covid-19 transmission, it doesn’t show anything of the sort. Let me explain.
Despite widespread claims that this new meta-analysis (actually, an update of an old meta-analysis) has definitively demonstrated that “masks don’t work” in reducing covid-19 transmission, it doesn’t show anything of the sort. Let me explain.
53. COCHRANE REVIEW
As @KelseyTuoc points out, of 78 studies in in this Cochrane review, only 6 (& only 2 on masks) were conducted during the covid-19 pandemic. All the rest were old RCTs in flu & other (less contagious) outbreaks in non-pandemic times.
vox.com/future-perfect…
As @KelseyTuoc points out, of 78 studies in in this Cochrane review, only 6 (& only 2 on masks) were conducted during the covid-19 pandemic. All the rest were old RCTs in flu & other (less contagious) outbreaks in non-pandemic times.
vox.com/future-perfect…
54. COCHRANE REVIEW
As well as combining covid studies with non-covid studies, Jefferson et al made another elementary lumping error. They combined RCTs in which HCWs had worn protection *some of the time* with RCTs in which they wore them *all the time*.
As well as combining covid studies with non-covid studies, Jefferson et al made another elementary lumping error. They combined RCTs in which HCWs had worn protection *some of the time* with RCTs in which they wore them *all the time*.
55. COCHRANE REVIEW
As we argue in this article, a meta-analysis that combines studies of different designs asking different questions will tend to produce un-nuanced and often negative findings. Mixing the paints in the paintbox gives you dull brown.
theconversation.com/yes-masks-redu…
As we argue in this article, a meta-analysis that combines studies of different designs asking different questions will tend to produce un-nuanced and often negative findings. Mixing the paints in the paintbox gives you dull brown.
theconversation.com/yes-masks-redu…
56. COCHRANE REVIEW
Here, @JenniferNuzzo (a fan of Cochrane revs) points out additional subtleties that cast doubt on the masks-don’t-work conclusion (which is not in any case what the review's authors concluded—at least, not in the review itself).
Here, @JenniferNuzzo (a fan of Cochrane revs) points out additional subtleties that cast doubt on the masks-don’t-work conclusion (which is not in any case what the review's authors concluded—at least, not in the review itself).
https://twitter.com/JenniferNuzzo/status/1621881097452666883?s=20
57. COCHRANE REVIEW
Here, Jason Abaluk @jabaluk of the impressive Bangladeshi mask RCT argues that the updated Jefferson review made the same mistakes they had made in previous versions.
Here, Jason Abaluk @jabaluk of the impressive Bangladeshi mask RCT argues that the updated Jefferson review made the same mistakes they had made in previous versions.
https://twitter.com/Jabaluck/status/1620485974819229697?s=20
58. COCHRANE REVIEW
Here, Satoshi Akima @ToshiAkima explains why Cochrane reviews should not be blithely swallowed as an assumed ‘gold standard’.
Here, Satoshi Akima @ToshiAkima explains why Cochrane reviews should not be blithely swallowed as an assumed ‘gold standard’.
https://twitter.com/ToshiAkima/status/1627184313593909248?s=20
59.COCHRANE REVIEW
Satoshi argues that whilst RCTs may provide *predictive* evidence (intervention A is more/less likely to produce outcome X than intervention B), they don’t provide *mechanistic* evidence (how does intervention A work?). I’ll come back to this.
Satoshi argues that whilst RCTs may provide *predictive* evidence (intervention A is more/less likely to produce outcome X than intervention B), they don’t provide *mechanistic* evidence (how does intervention A work?). I’ll come back to this.
60. COCHRANE REVIEW
Here, @danwalker9999, citing @BlakeMMurdoch, accuses the authors of the Jefferson Cochrane review of “amazing sloppiness” (failing to access and incorporate raw data from the Abaluk trial that was in the public domain).
Here, @danwalker9999, citing @BlakeMMurdoch, accuses the authors of the Jefferson Cochrane review of “amazing sloppiness” (failing to access and incorporate raw data from the Abaluk trial that was in the public domain).
https://twitter.com/danwalker9999/status/1629531188791746562?s=20
61. COCHRANE REVIEW
Have I persuaded you that Cochrane reviews aren’t a magic higher form of science that automatically knocks all other evidence out of the park? They look at a narrow slice of evidence and can be done well or badly. Where’s the quality control? Good question.
Have I persuaded you that Cochrane reviews aren’t a magic higher form of science that automatically knocks all other evidence out of the park? They look at a narrow slice of evidence and can be done well or badly. Where’s the quality control? Good question.
62.COCHRANE REVIEW
Some (though not all) Cochrane authors believe that the RCT is such a superior form of evidence that we don’t even have to look at any other kinds of evidence (unless our search for RCTs turns up none). Let me explain why this is a dangerously naïve assumption
Some (though not all) Cochrane authors believe that the RCT is such a superior form of evidence that we don’t even have to look at any other kinds of evidence (unless our search for RCTs turns up none). Let me explain why this is a dangerously naïve assumption
63. MECHANISTIC EVIDENCE
Bradford Hill (famous for doing the 1st ever RCT) emphasised that we can’t rely solely on probabilistic evidence from RCTs. We also need mechanistic evidence (see tweet 58). We explain in this paper on EBM+:
ebm.bmj.com/content/27/5/2…
Bradford Hill (famous for doing the 1st ever RCT) emphasised that we can’t rely solely on probabilistic evidence from RCTs. We also need mechanistic evidence (see tweet 58). We explain in this paper on EBM+:
ebm.bmj.com/content/27/5/2…
64. MECHANISTIC EVIDENCE
When Jefferson et al ignore ALL evidence except RCTs and also use synthesis methods that *make no sense* when you take the *mechanism of transmission* into account (i.e. lumping continuous masking RCTs with intermittent masking RCTs), I have a problem.
When Jefferson et al ignore ALL evidence except RCTs and also use synthesis methods that *make no sense* when you take the *mechanism of transmission* into account (i.e. lumping continuous masking RCTs with intermittent masking RCTs), I have a problem.
65. MECHANISTIC EVIDENCE
Mechanistic evidence (which Jefferson et al conspicuously ignore) means evidence – from basic science laboratory experiments and real-world case studies for example – that helps us understand how the virus spreads and how covering the face *could* work.
Mechanistic evidence (which Jefferson et al conspicuously ignore) means evidence – from basic science laboratory experiments and real-world case studies for example – that helps us understand how the virus spreads and how covering the face *could* work.
66.MECHANISTIC EVIDENCE
My original mask thread (see tweet 2) presented lots more mechanistic evidence that whilst *some* transmission of SARS-CoV-2 might conceivably happen by droplets, *most* transmission happens by airborne viruses which enter the lungs when we breathe in.
My original mask thread (see tweet 2) presented lots more mechanistic evidence that whilst *some* transmission of SARS-CoV-2 might conceivably happen by droplets, *most* transmission happens by airborne viruses which enter the lungs when we breathe in.
67. MECHANISTIC EVIDENCE
Airborne transmission happens *mainly* when you’re very close to someone who is exhaling the virus. But airborne viruses *float in the air* so they spread throughout an indoor space. Rules like “wear your mask/respirator within 2 metres” don’t make sense
Airborne transmission happens *mainly* when you’re very close to someone who is exhaling the virus. But airborne viruses *float in the air* so they spread throughout an indoor space. Rules like “wear your mask/respirator within 2 metres” don’t make sense
68. MECHANISTIC EVIDENCE
Airborne transmission of SARS-CoV-2 explains why protection that *blocks airborne particles* (i.e. respirators) is in theory better than protection that blocks droplets, and why we’d expect a well-designed RCT of respirators vs masks to favor the former.
Airborne transmission of SARS-CoV-2 explains why protection that *blocks airborne particles* (i.e. respirators) is in theory better than protection that blocks droplets, and why we’d expect a well-designed RCT of respirators vs masks to favor the former.
69. MECHANISTIC EVIDENCE
Just because mechanistic evidence suggests respirators will outperform medical masks doesn’t mean we should ignore RCTs that show no advantage. But it does mean we should *design those RCTs properly* so that an advantage, if it exists, would show up.
Just because mechanistic evidence suggests respirators will outperform medical masks doesn’t mean we should ignore RCTs that show no advantage. But it does mean we should *design those RCTs properly* so that an advantage, if it exists, would show up.
70. EXPLAINING THE CONTROVERSY
Because RCTs and meta-analyses were poorly designed (overlooking mechanism of transmission), many produced negative findings. Some researchers (+ press and public) have conflated *absence of evidence of effect* with *evidence of lack of effect*.
Because RCTs and meta-analyses were poorly designed (overlooking mechanism of transmission), many produced negative findings. Some researchers (+ press and public) have conflated *absence of evidence of effect* with *evidence of lack of effect*.
71.EXPLAINING THE CONTROVERSY
I’ve argued from philosophical perspective that flawed mental models assuming a ‘droplet’ mode of spread led scientists to greatly under-estimate the importance of masking. (NB I’m NOT saying it’s a bad idea to wash hands) (royalsocietypublishing.org/doi/10.1098/rs…
I’ve argued from philosophical perspective that flawed mental models assuming a ‘droplet’ mode of spread led scientists to greatly under-estimate the importance of masking. (NB I’m NOT saying it’s a bad idea to wash hands) (royalsocietypublishing.org/doi/10.1098/rs…
72. EXPLAINING THE CONTROVERSY
For an unforgivably long time, WHO and others denied that SARS-CoV-2 was airborne (see tweets 9-20). We wrote a paper on why this error happened (TL;DR: powerful doctors had entrenched mental models & reputations to lose). wellcomeopenresearch.org/articles/6-126
For an unforgivably long time, WHO and others denied that SARS-CoV-2 was airborne (see tweets 9-20). We wrote a paper on why this error happened (TL;DR: powerful doctors had entrenched mental models & reputations to lose). wellcomeopenresearch.org/articles/6-126
73. EXPLAINING THE CONTROVERSY
These flawed mental models led to flawed policy narratives, diverting us into an *obsessive concern with handwashing and squirty sanitisers* and thinking that medical masks (designed to block droplets) will do for HCWs.
bmj.com/content/378/bm…
These flawed mental models led to flawed policy narratives, diverting us into an *obsessive concern with handwashing and squirty sanitisers* and thinking that medical masks (designed to block droplets) will do for HCWs.
bmj.com/content/378/bm…
74.OBSERVATIONAL EVIDENCE
Let’s return to the question of community masking. Notwithstanding @JABALOK’s impressive RCT, it remains the case that this kind of study is difficult & expensive to do & hard to interpret. What other evidence is there? I get asked this question a lot.
Let’s return to the question of community masking. Notwithstanding @JABALOK’s impressive RCT, it remains the case that this kind of study is difficult & expensive to do & hard to interpret. What other evidence is there? I get asked this question a lot.
75. OBSERVATIONAL EVIDENCE
Countries that introduced mandated masking within 30 days of the first case (mostly Asian) had *dramatically* fewer Covid-19 cases than those that delayed beyond 100 days (mostly Western).
ajtmh.org/view/journals/……
Countries that introduced mandated masking within 30 days of the first case (mostly Asian) had *dramatically* fewer Covid-19 cases than those that delayed beyond 100 days (mostly Western).
ajtmh.org/view/journals/……
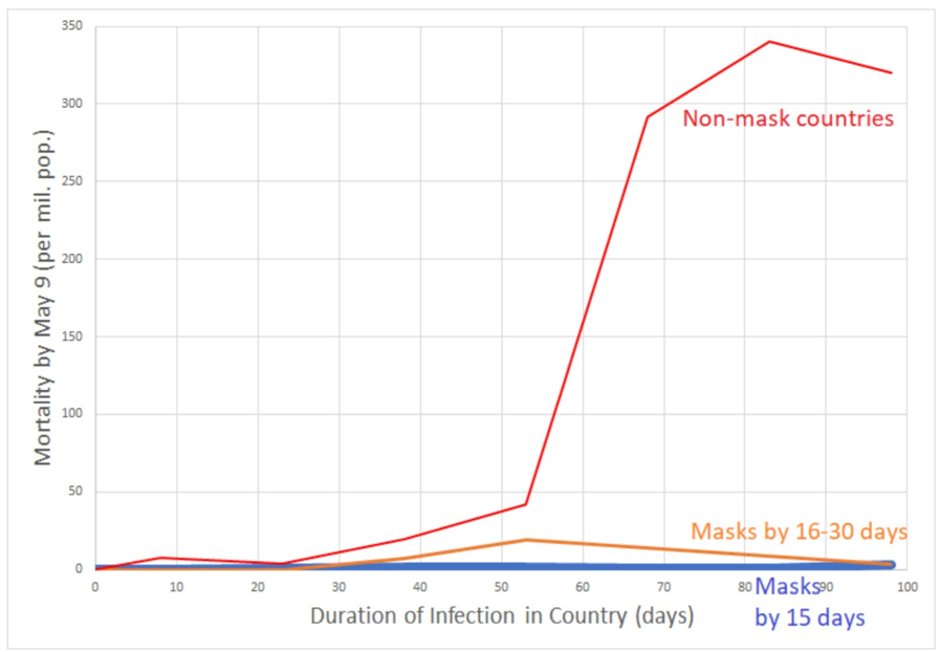
76. OBSERVATIONAL EVIDENCE
Was this association or causation? Early on, we didn’t know (though, importantly, nobody in these Asian countries seemed to come to harm from wearing a mask). Since that early study, there have been numerous studies of the impact of mask mandates.
Was this association or causation? Early on, we didn’t know (though, importantly, nobody in these Asian countries seemed to come to harm from wearing a mask). Since that early study, there have been numerous studies of the impact of mask mandates.
77. OBSERVATIONAL EVIDENCE
Various systematic reviews of mask mandates have been published. This from 2021 showed a statistically significant effect of mask mandates (same effect size as handwashing, with physical distancing having an even greater effect)
bmj.com/content/375/bm…
Various systematic reviews of mask mandates have been published. This from 2021 showed a statistically significant effect of mask mandates (same effect size as handwashing, with physical distancing having an even greater effect)
bmj.com/content/375/bm…
78. OBSERVATIONAL EVIDENCE
Yanni Li et al did a meta-analysis of case-control studies. Acknowledging the limitations of such designs, they found masks reduced SARS-CoV-2 infections by (on average) ~70% in healthcare workers and ~60% in lay people. ncbi.nlm.nih.gov/pmc/articles/P…… 35/
Yanni Li et al did a meta-analysis of case-control studies. Acknowledging the limitations of such designs, they found masks reduced SARS-CoV-2 infections by (on average) ~70% in healthcare workers and ~60% in lay people. ncbi.nlm.nih.gov/pmc/articles/P…… 35/
79. OBSERVATIONAL EVIDENCE
What’s a case-control study? Find people who caught Covid; match them with people who were similar but didn’t catch Covid; ask whether each was wearing a mask. Relatively weak design (bc unmeasured confounders), but not as weak as a badly-designed RCT
What’s a case-control study? Find people who caught Covid; match them with people who were similar but didn’t catch Covid; ask whether each was wearing a mask. Relatively weak design (bc unmeasured confounders), but not as weak as a badly-designed RCT
80. OBSERVATIONAL EVIDENCE
This review of observational studies of various public health measures in the pandemic found that 6 of 7 studies of mask mandates showed a statistically significant effect. Studies rated higher quality found greater effects.
sciencedirect.com/science/articl…
This review of observational studies of various public health measures in the pandemic found that 6 of 7 studies of mask mandates showed a statistically significant effect. Studies rated higher quality found greater effects.
sciencedirect.com/science/articl…
81.OBSERVATIONAL EVIDENCE
The Talic review (tweet 77) highlighted this study by Liu et al, who looked at (inter alia) introduction of mask mandates in different US states. After correcting for confounders, mask mandates reduced transmission by 29%.
link.springer.com/article/10.118…
The Talic review (tweet 77) highlighted this study by Liu et al, who looked at (inter alia) introduction of mask mandates in different US states. After correcting for confounders, mask mandates reduced transmission by 29%.
link.springer.com/article/10.118…
82. OBSERVATIONAL EVIDENCE
A more recent study of observational data across US states by Ahlers et al showed that (after complex statistical measures to correct for confounders) mask mandates were associated with significantly reduced transmission rate
bmjmedicine.bmj.com/content/1/1/e0…
A more recent study of observational data across US states by Ahlers et al showed that (after complex statistical measures to correct for confounders) mask mandates were associated with significantly reduced transmission rate
bmjmedicine.bmj.com/content/1/1/e0…
83. OBSERVATIONAL EVIDENCE
Two more studies of mask mandates across US states, again showing the localities with mask mandates had lower transmission whilst the mandates were in place, and lower hospitalisations from covid-19
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…
Two more studies of mask mandates across US states, again showing the localities with mask mandates had lower transmission whilst the mandates were in place, and lower hospitalisations from covid-19
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…
84.OBSERVATIONAL EVIDENCE
And here’s Miriam Van Dyke’s study of more granular data on mask mandates across the state of Kansas, USA, in 2020. Again, localities that implemented mask mandates had lower transmission after confounders were controlled for.
ncbi.nlm.nih.gov/pmc/articles/P…
And here’s Miriam Van Dyke’s study of more granular data on mask mandates across the state of Kansas, USA, in 2020. Again, localities that implemented mask mandates had lower transmission after confounders were controlled for.
ncbi.nlm.nih.gov/pmc/articles/P…
85. OBSERVATIONAL EVIDENCE
In another recent study, Daniel Cooper et al try to unpack whether the *association* between mask mandates and lower covid-19 cases across US states from 2020 is *causal*. They conclude that it is.
sciencedirect.com/science/articl…
In another recent study, Daniel Cooper et al try to unpack whether the *association* between mask mandates and lower covid-19 cases across US states from 2020 is *causal*. They conclude that it is.
sciencedirect.com/science/articl…
86. AOB
We wrote a summary review of masks and masking here (now somewhat out of date but includes a lot of useful papers). [need break - will resume thread after tea]
acpjournals.org/doi/abs/10.732…
We wrote a summary review of masks and masking here (now somewhat out of date but includes a lot of useful papers). [need break - will resume thread after tea]
acpjournals.org/doi/abs/10.732…
87. AOB
The rest of this thread links to additional key evidence on the mask/masking debate. This from @jljcolorado on why people wrongly assumed for so long that respiratory illnesses are droplet-spread.
The rest of this thread links to additional key evidence on the mask/masking debate. This from @jljcolorado on why people wrongly assumed for so long that respiratory illnesses are droplet-spread.
https://twitter.com/jljcolorado/status/1391111720526024708?s=20
88. AOB
A landmark paper from Adriaan Bax’s team showing that breathing, speaking and singing are key activities that transmit SARS-CoV-2 ncbi.nlm.nih.gov/pmc/articles/P…
A landmark paper from Adriaan Bax’s team showing that breathing, speaking and singing are key activities that transmit SARS-CoV-2 ncbi.nlm.nih.gov/pmc/articles/P…
89. AOB
The Bagheri et al modelling study: what if one person masks? What if both people mask?
The Bagheri et al modelling study: what if one person masks? What if both people mask?
https://twitter.com/HuffmanLabDU/status/1467430860676763651?s=20
90. AOB
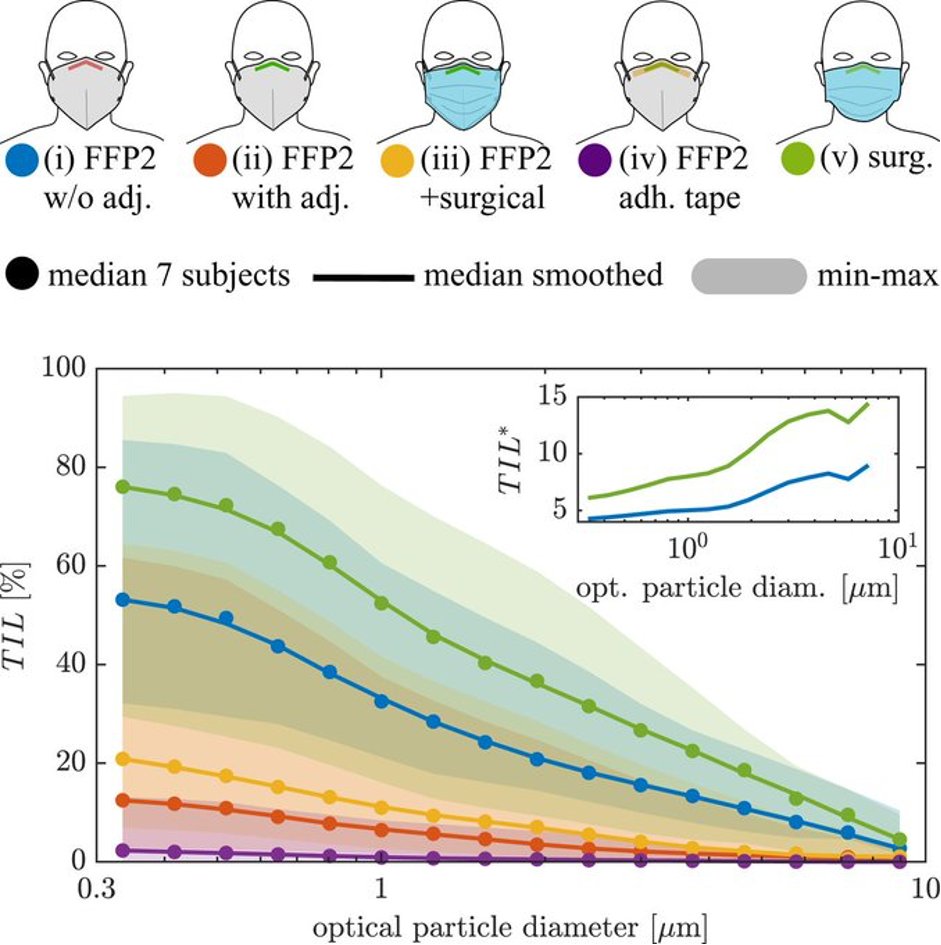
TIL = total inward leakage (vertical axis). Jargon for "air getting in round the sides of your badly-fitting mask". High TIL is bad. Aim for PURPLE: wear a FFP2 & use a bit of tape to close the gaps. GREEN is an untaped surgical mask - useless! pnas.org/doi/pdf/10.107…
TIL = total inward leakage (vertical axis). Jargon for "air getting in round the sides of your badly-fitting mask". High TIL is bad. Aim for PURPLE: wear a FFP2 & use a bit of tape to close the gaps. GREEN is an untaped surgical mask - useless! pnas.org/doi/pdf/10.107…
91. AOB
Here’s a nice theory-based review of the psychology of mask-wearing (or mask-refusing). Talks about 3 main constructs: autonomy, psychological relatedness, and competence.
mdpi.com/1660-4601/17/1…
Here’s a nice theory-based review of the psychology of mask-wearing (or mask-refusing). Talks about 3 main constructs: autonomy, psychological relatedness, and competence.
mdpi.com/1660-4601/17/1…
92. AOB
Thanks several people for pointing out I forgot to add the before-and-after Cambridge study showing HCW covid infections went right down after N95s introduced
cam.ac.uk/research/news/…
Thanks several people for pointing out I forgot to add the before-and-after Cambridge study showing HCW covid infections went right down after N95s introduced
cam.ac.uk/research/news/…
93. AOB
We don't have to wear masks everywhere, for ever. We should adjust our masking behaviour to reflect the prevailing risk of transmission.
theconversation.com/heres-where-an…
We don't have to wear masks everywhere, for ever. We should adjust our masking behaviour to reflect the prevailing risk of transmission.
theconversation.com/heres-where-an…
94. PS
Another thread, from Tomas Pueyo, pointing out serious flaws with the Jefferson Cochrane review which is being (wrongly) interpreted as proving that masks don't work.
Another thread, from Tomas Pueyo, pointing out serious flaws with the Jefferson Cochrane review which is being (wrongly) interpreted as proving that masks don't work.
https://twitter.com/tomaspueyo/status/1630000803141255169?s=20
95. PS
Another relevant thread from @dontwantadothis pointing out the differences between RCTs of behavioural interventions such as masking and the more conventional RCTs of drug v placebo.
Another relevant thread from @dontwantadothis pointing out the differences between RCTs of behavioural interventions such as masking and the more conventional RCTs of drug v placebo.
https://twitter.com/dontwantadothis/status/1630023818306543617?s=20
• • •
Missing some Tweet in this thread? You can try to
force a refresh