1/
You staff a new consult w/ your team. You share pearls & make a plan.
Then:
🩻 You review the CT w/ radiology.
🤝 You chat w/ another consult service.
🗣️ You deliver your recs at the workroom.
📲 You call night float w/ an update.
So many opportunities to teach!
This week:
You staff a new consult w/ your team. You share pearls & make a plan.
Then:
🩻 You review the CT w/ radiology.
🤝 You chat w/ another consult service.
🗣️ You deliver your recs at the workroom.
📲 You call night float w/ an update.
So many opportunities to teach!
This week:

2/
Last week @JenniferSpicer4 kicked off our segment on "Teaching the Primary Team" by focusing on "The Why."
This week, for "The Who", I want to think beyond just the primary team to identify the many different learners we encounter as consultants.
Last week @JenniferSpicer4 kicked off our segment on "Teaching the Primary Team" by focusing on "The Why."
https://twitter.com/JenniferSpicer4/status/1628082665025941512?s=20
This week, for "The Who", I want to think beyond just the primary team to identify the many different learners we encounter as consultants.
3/
Why?
Even though the primary team is the obvious audience for teaching - their "ask" is what invited us into the case to begin with! - we usually interface with many other teams in the process of rendering our opinion.
All of these teams have learners we can impact!
Why?
Even though the primary team is the obvious audience for teaching - their "ask" is what invited us into the case to begin with! - we usually interface with many other teams in the process of rendering our opinion.
All of these teams have learners we can impact!
4/
And, once we recognize the range of learners we are teaching - explicitly or implicitly - we must also acknowledge that the consult "ask" is just one domain of content about which we can/should teach.
This means we must tailor our teaching to both the learner & their team.
And, once we recognize the range of learners we are teaching - explicitly or implicitly - we must also acknowledge that the consult "ask" is just one domain of content about which we can/should teach.
This means we must tailor our teaching to both the learner & their team.
5/
For this 🧵, I'll discuss potential learners on the following teams:
📌 The primary team (who requested the consult)
📌 Other consulting teams seeing the same patient
📌 Teams providing diagnostic information for the case (e.g., radiology, pathology, microbiology, etc.)
For this 🧵, I'll discuss potential learners on the following teams:
📌 The primary team (who requested the consult)
📌 Other consulting teams seeing the same patient
📌 Teams providing diagnostic information for the case (e.g., radiology, pathology, microbiology, etc.)
6/
Let's start w/ the primary team.
A teacher-learner relationship is “built-in” to the consult interaction.
It can start off on the wrong foot when there are misunderstandings about “where” the learner is.
I previously shared strategies to avoid this:
Let's start w/ the primary team.
A teacher-learner relationship is “built-in” to the consult interaction.
It can start off on the wrong foot when there are misunderstandings about “where” the learner is.
I previously shared strategies to avoid this:
https://twitter.com/VarunPhadke2/status/1605245928549629960?s=20
7/
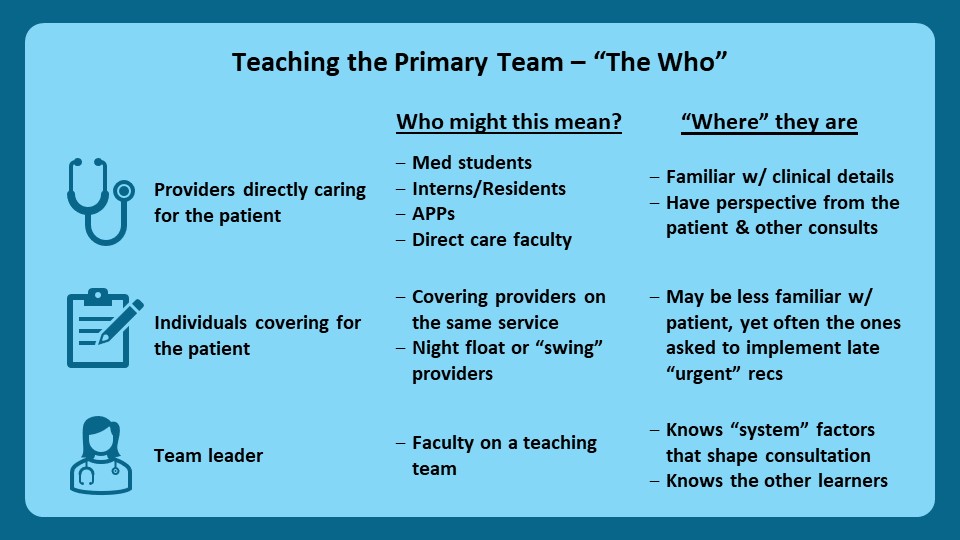
Intrinsic to that framework is the recognition that the “primary team” comprises a range of people to teach.
This includes:
🩺 Those directly caring for the patient
📋 Individuals covering for the patient
👩⚕️ The team leader
We must modify our teaching scripts accordingly!
Intrinsic to that framework is the recognition that the “primary team” comprises a range of people to teach.
This includes:
🩺 Those directly caring for the patient
📋 Individuals covering for the patient
👩⚕️ The team leader
We must modify our teaching scripts accordingly!
8/
Now let’s turn to other consulting teams.
It’s pretty routine for multiple specialists to be “on board” a complex case.
Despite this, the inter-consultant interaction often gets neglected.
And the primary team ends up as the intermediary.
Now let’s turn to other consulting teams.
It’s pretty routine for multiple specialists to be “on board” a complex case.
Despite this, the inter-consultant interaction often gets neglected.
And the primary team ends up as the intermediary.
9/
It doesn’t have to be this way!
As consultants we need to be intentional about this interaction to make it productive.
Learners on other consult teams who are trying to build their own scripts, schemas, and decision thresholds benefit from the wisdom of other specialists!
It doesn’t have to be this way!
As consultants we need to be intentional about this interaction to make it productive.
Learners on other consult teams who are trying to build their own scripts, schemas, and decision thresholds benefit from the wisdom of other specialists!

10/
Finally, let’s recognize learners on teams that contribute diagnostic data.
Because radiology, pathology, & microbiology results are so often the trigger for consults, a consultant’s workflow often includes interfacing directly w/ the people that generate those results.
Finally, let’s recognize learners on teams that contribute diagnostic data.
Because radiology, pathology, & microbiology results are so often the trigger for consults, a consultant’s workflow often includes interfacing directly w/ the people that generate those results.
11/
There are two key teaching opportunities here:
1⃣ Sharing of clinical nuance that might shape their interpretation (beyond the limited “reason for exam”)
2⃣ Diagnostic feedback to help reinforce/hone their clinical skills
@StefanTigges @StewartGNeill - any others?
There are two key teaching opportunities here:
1⃣ Sharing of clinical nuance that might shape their interpretation (beyond the limited “reason for exam”)
2⃣ Diagnostic feedback to help reinforce/hone their clinical skills
@StefanTigges @StewartGNeill - any others?
12/
Let's recap:
In this 🧵 we:
📌 Identified learners beyond the primary team that we also have the opportunity to teach
📌 Described the benefits of expanding our teaching efforts to include those learners
📌 Explored broad domains of teaching scripts for each of these teams
Let's recap:
In this 🧵 we:
📌 Identified learners beyond the primary team that we also have the opportunity to teach
📌 Described the benefits of expanding our teaching efforts to include those learners
📌 Explored broad domains of teaching scripts for each of these teams

13/
Next week @JenniferSpicer4 will continue this series on “Teaching the Primary Team” focusing on “The When.”
Remember to check out #SubspecialtyTeaching @MedEdTwagTeam & follow @YihanYangMD @GStetsonMD @ChrisDJacksonMD to keep up with all our threads!
See you next week!
Next week @JenniferSpicer4 will continue this series on “Teaching the Primary Team” focusing on “The When.”
Remember to check out #SubspecialtyTeaching @MedEdTwagTeam & follow @YihanYangMD @GStetsonMD @ChrisDJacksonMD to keep up with all our threads!
See you next week!

• • •
Missing some Tweet in this thread? You can try to
force a refresh