Never in the history of medicine has so much been done, by so many, so incompetently, with so little consequence as in the treatment of severe hyponatremia. #Tweetorial 1/10
You shouldn't correct hyponatremia too fast. The speed limit is 8 mmol/L per day. We are terrible at it. In George et al, 41% of 1,490 pts were corrected faster than 8 mEq/L. Look at the poor slobs at the left of the nomogram whose Na actually went down 🤪 2/10
Thankfully this incompetence is rarely punished. Of the 611 (41% of 1490) patients who over-corrected in the George trial, only 7 developed osmotic demyelination syndrome (ODS). Screw the sodium correction and you can get away with it 99% of the time. 3/10
I was invited to help a study looking at the incidence of ODS in hyponatremia using the GEMINI database which tracks internal medicine admissions in Toronto. It is amazing when someone you look up to DMs you asking to join them on an important study. Thanks @FralickMike 4/10
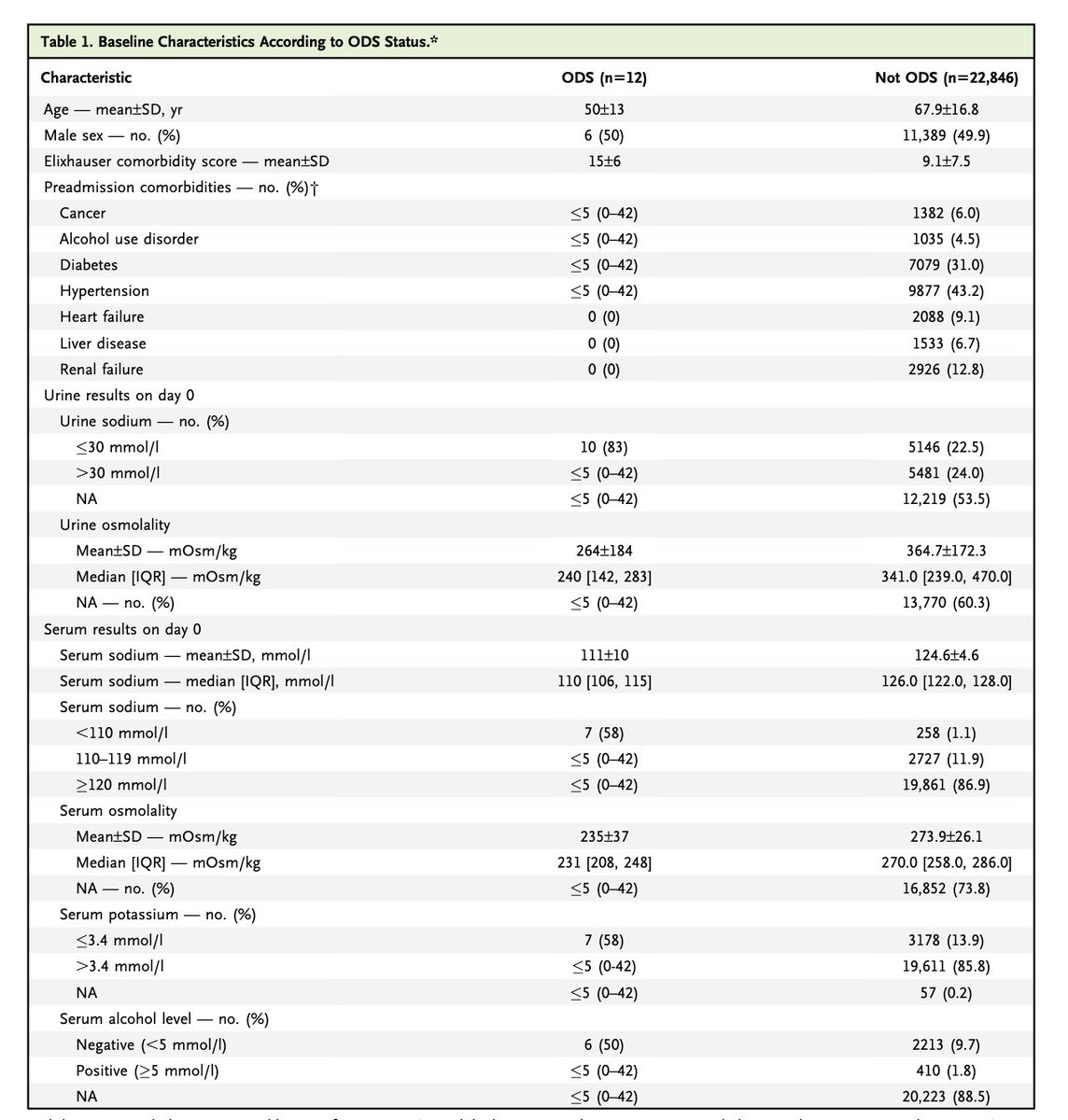
We tracked every case of hyponatremia (Na < 130) admitted to 5 academic hospitals in Toronto from 2010-2020.
22,858 cases. This is the biggest hyponatremia study ever. Even if you restrict the cohort to just sodiums < 120, it is nearly 2x George et al 5/10
22,858 cases. This is the biggest hyponatremia study ever. Even if you restrict the cohort to just sodiums < 120, it is nearly 2x George et al 5/10
The Canadians seem to do a better job of correcting the sodium, went too fast in only 18% of cases, 3632 patients. But hold on, a lot of these people had relatively mild hyponatremia. When you break it down by starting Na, Canadians look just as bad as the US at going slow 6/10
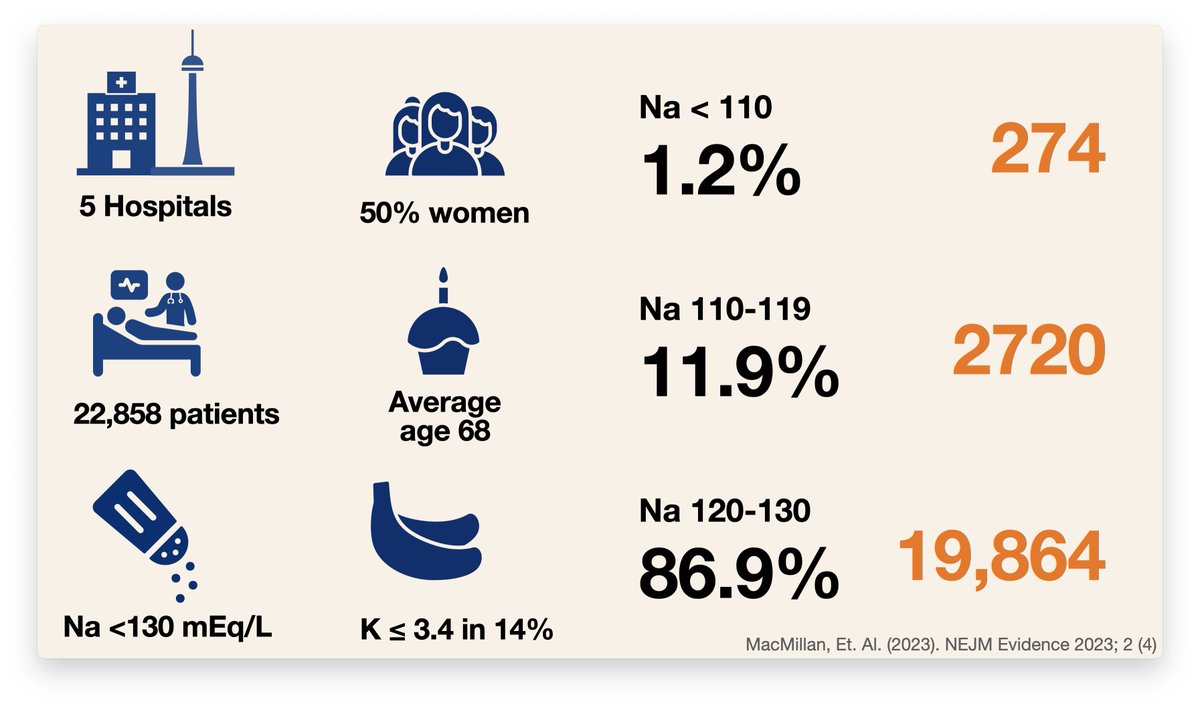
And what was the consequence of all that hyponatremia? All that rapid correction? 12 of osmotic demyelinating syndrome.
12 out of 22,858. 0.05%
If you divide by starting Na they found an incidence of:
0.3% with a Na < 120
0.015% with a Na > 120
**2.5% with a Na < 110**
7/10
12 out of 22,858. 0.05%
If you divide by starting Na they found an incidence of:
0.3% with a Na < 120
0.015% with a Na > 120
**2.5% with a Na < 110**
7/10
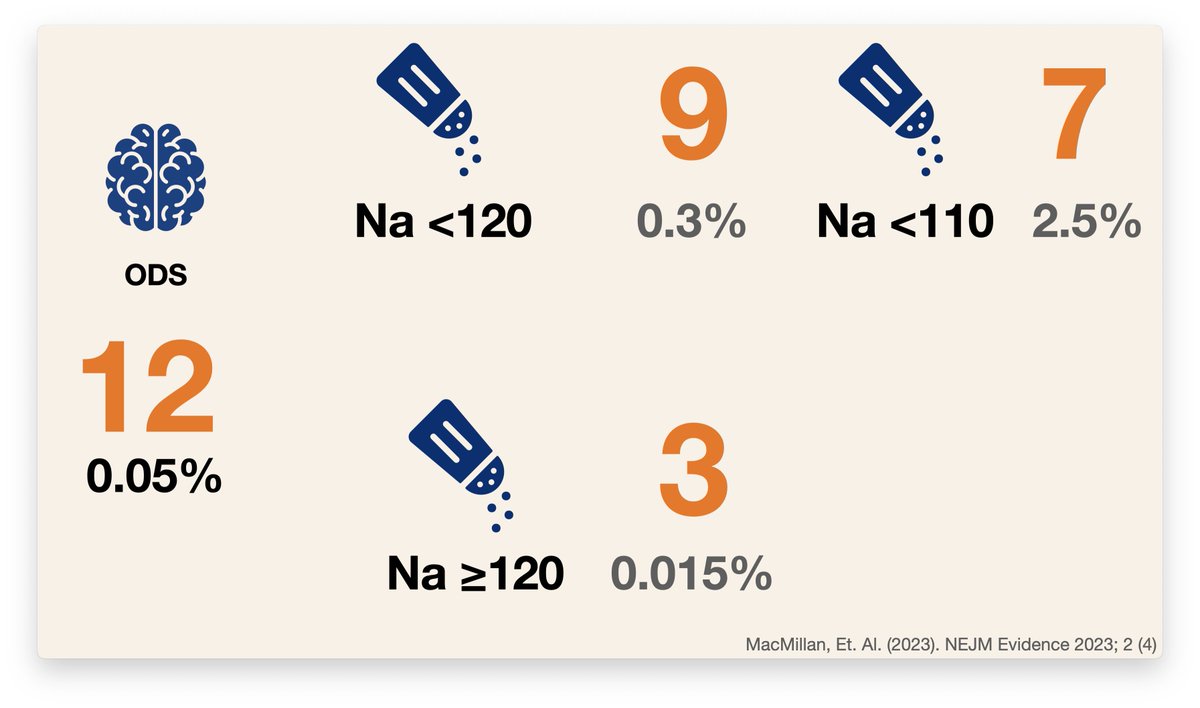
The part of the manuscript you are looking for is the rates of ODS by rapid versus slow correction. Sorry. We couldn't publish this due to the ethical guardrails placed on this trial. And the statisticians wouldn’t whisper it in my ear because they know me. Bummer. 8/10
So what can we take from this paper? ODS is rare; Canadians are just at bad correcting the sodium slowly as the guys in Pittsburgh; and the rate of ODS really rises as the initial sodium level goes does down, from a trivial 0.015% at levels > 120 to 2.5% with sodiums < 110. 9/10
Take a look at the paper and at the George paper.
evidence.nejm.org/doi/10.1056/EV…
pubmed.ncbi.nlm.nih.gov/29871886/
evidence.nejm.org/doi/10.1056/EV…
pubmed.ncbi.nlm.nih.gov/29871886/
• • •
Missing some Tweet in this thread? You can try to
force a refresh