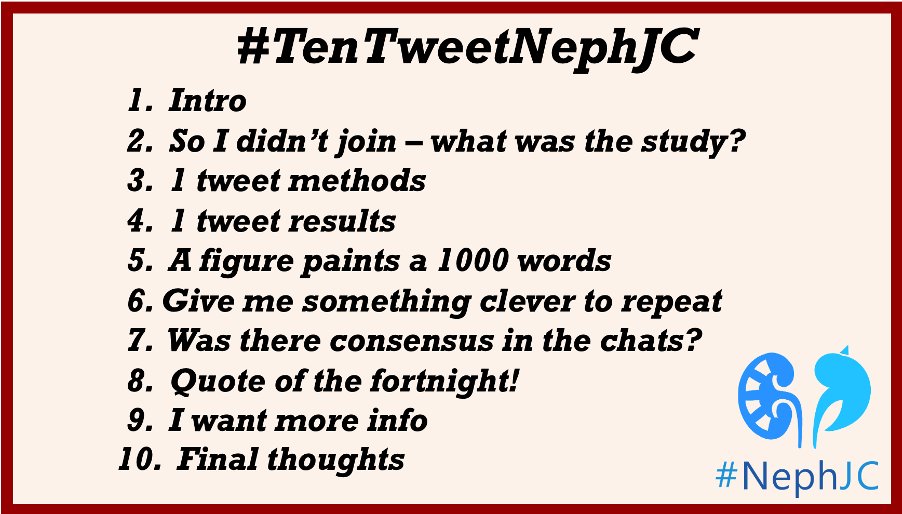
Welcome to #TenTweetNephJC for a short recap! Nephrologists warned of renalism neglecting cardiac ischemia in kidney pts. ISCHEMIA-CKD dashed hopes. Waiting for a deceased donor kidney transplant in the US is a grueling journey for +100K pts with advanced chronic kidney disease 

2/10
What did I miss?
🌤️Retrospective study: asymptomatic kidney transplant candidates tested for coronary heart disease (CHD) vs non-tested pubmed.ncbi.nlm.nih.gov/36595271/
Aim: to determine the effect of CHD testing on the risk of death or acute MI within 30 days after transplant
What did I miss?
🌤️Retrospective study: asymptomatic kidney transplant candidates tested for coronary heart disease (CHD) vs non-tested pubmed.ncbi.nlm.nih.gov/36595271/
Aim: to determine the effect of CHD testing on the risk of death or acute MI within 30 days after transplant
3/10
1 tweet methods
⏪ Retrospective cohort study, USRDS, 2000-2014
✅ 79334 Adults, 1st time kidney transplant
✅ CHD testing 12 months before transplant
🛠️ Instrumental analysis variable - less biased by confounding than standard methods @Husamjz

1 tweet methods
⏪ Retrospective cohort study, USRDS, 2000-2014
✅ 79334 Adults, 1st time kidney transplant
✅ CHD testing 12 months before transplant
🛠️ Instrumental analysis variable - less biased by confounding than standard methods @Husamjz


4/10
1 tweet results
❤️ Primary outcome reached in 5.3% (4604) patients - are this numbers correct?
💔Death in 2063 patients while acute MI in 2329 patients
1 tweet results
❤️ Primary outcome reached in 5.3% (4604) patients - are this numbers correct?
💔Death in 2063 patients while acute MI in 2329 patients

6/10
Give me something clever to say
We are quoting a cardiologist, but not every cardiologist, the son of a nephrologist @jelevenson

Give me something clever to say
We are quoting a cardiologist, but not every cardiologist, the son of a nephrologist @jelevenson
https://twitter.com/jelevenson/status/1635812684099641345

7/10
Chat consensus?
1️⃣ Revascularization (by extension testing) isn't benign. Denying transplants is definitely doing people harm
2️⃣ Isn't dialysis a form of stress testing?
3️⃣ CV events decline after transplant. We should think of transplant as revascularization by proxy
Chat consensus?
1️⃣ Revascularization (by extension testing) isn't benign. Denying transplants is definitely doing people harm
2️⃣ Isn't dialysis a form of stress testing?
3️⃣ CV events decline after transplant. We should think of transplant as revascularization by proxy
8/10
Quote of the fortnight!
Is @hswapnil the most quoted in #TenTweetNephJC? 🧠

Quote of the fortnight!
Is @hswapnil the most quoted in #TenTweetNephJC? 🧠
https://twitter.com/hswapnil/status/1635996627130302467?s=20

9/10
I want more info
✅Follow @gchertow, @BaiocchiMike & @StanfordNeph
✅ About journey to the waitlist in @Nephmasness blog
ajkdblog.org/2023/03/01/nep…
✅#NephJC summary: @DrCool_Beans @meyyappannephro
nephjc.com/news/pre-trans…
✅2 VAs by @renspasilan @Nihal_Hamary @MedPEEdsKidneys

I want more info
✅Follow @gchertow, @BaiocchiMike & @StanfordNeph
✅ About journey to the waitlist in @Nephmasness blog
ajkdblog.org/2023/03/01/nep…
✅#NephJC summary: @DrCool_Beans @meyyappannephro
nephjc.com/news/pre-trans…
✅2 VAs by @renspasilan @Nihal_Hamary @MedPEEdsKidneys


10/10
Final thoughts
✳️ Waitlist journey can be daunting as it is, our patients don’t need more impediments when aren't really necessary
➡️Up next, Rolling Stone's new hit Hydrochlorothiazide couldn't give any satisfaction in preventing kidney stones
pubmed.ncbi.nlm.nih.gov/36856614/
Final thoughts
✳️ Waitlist journey can be daunting as it is, our patients don’t need more impediments when aren't really necessary
➡️Up next, Rolling Stone's new hit Hydrochlorothiazide couldn't give any satisfaction in preventing kidney stones
pubmed.ncbi.nlm.nih.gov/36856614/

I admit sometimes I'm stumbling more than I'm learning. But thanks to truly fantastic support and guidance of #NephJC people, I am here today, 1 year after hosting my 1st #NephJC, happy to continue my journey along with #NephJC & @NSMCInternship Cristina Popa, @NephroSeeker 

• • •
Missing some Tweet in this thread? You can try to
force a refresh