Okay @amit_pawa vs @jeffgadsden debate just completed at #RAUK23 - fantastic Pro/Con debate. @garrettsbarry, as promised, here it is
@jeffgadsden takes the Pro argument, in what he feels shouldn’t really be a face off. Note: tearing off the nerve stimulator cord is a tad aggressive #RAUK23 





@jeffgadsden proposes the 4 pillars of his argument. 1. A means to avoid intraneural needle tip placement. Seems to shoot himself in the foot immediately by pointing out poor sensitivity #RAUK23 





Triple monitoring reduced false negatives. With US alone are we 100% sure we’re not too close every time - No. Not much literature to support, but consequences of error are massive. Worth having a belt and braces approach? Probably. #RAUK23 







And it’s easy to do - 6 seconds. What an awesome slowmo replay! #RAUK23 

2. A way to avoid skewering neighbouring nerves. RAPTIR block illustrates tiger territory - suprascapular nerve. #RAUK23 







A solution = stimulation. Note: hand placement to detect a twitch while advancing the needle #RAUK23 



Also during Adductor Canal Block that regionalists perform daily - nerve to Vastus Medialis not always visible on US #RAUK23 





Sure dissection with saline helps, but stimulation adds efficacy and safety (twitch means stop). Consequences are notable. #RAUK23 







3. Help identify nerve when US fails. Not sure how much of USA constitutes the “Biscuit Belt” but we all have obese patients where US does NOT visualize the nerves - stimulation keeps us safe? #RAUK23 



4. Help identify correct fascial plane. QLB needs to avoid injection into Psoas Major - otherwise you end up with lumbar plexus block (effective but can’t move leg). If psoas muscle twitches = bad! Know you’re there when QL stops twitching. #RAUK23 



Summary of how stimulation helps. Equates to seatbelt vs airbags debate (seatbelts so last season once airbags arrived) - but both = better! #RAUK23 







@jeffgadsden argues US and nerve stimulation should be a bromance… somewhat like @BlockIt_Hot_Pod #RAUK23 



@amit_pawa up for the CON side of the debate. Keeping the patient in sight as the real winner of the debate no matter which way it goes. #RAUK23 



Oh dear, a sign of weakness from @amit_pawa - altering the parameters of the debate? Will it hurt him? #RAUK23 



Appealing to emotions of the audience - excellent debate strategy from @amit_pawa (I’m sure @RegionalAnaesUK will miss him). But his talk will be serious with no-subliminal messages whatsoever #RAUK23 







Does nerve stimulation really separate these bromance partners of @BlockIt_Hot_Pod? @amit_pawa has cried foul on tape - says it was AI. #RAUK23 

@amit_pawa focusing the point of the debate - or more specifically where the needle’s point SHOULDN’T be. #RAUK23 







Despite advances in regional anesthesia, long term nerve injury remains unchanged. Do we need a belt and braces (or triple check) approach. Ooh early but has @amit_pawa delivered his mic-drop moment quoting @jeffgadsden from the literature? #RAUK23 





Illustrating the premise, but is it always reliable? Right @jeffgadsden spoke about 0.2mA, but most use higher values… #RAUK23 







A tale of two pigs (no third found @amit_pawa?): NO twitches with INTRANEURAL needles - not very sensitive. Ultrasound DOES detect intraneural injection #RAUK23 





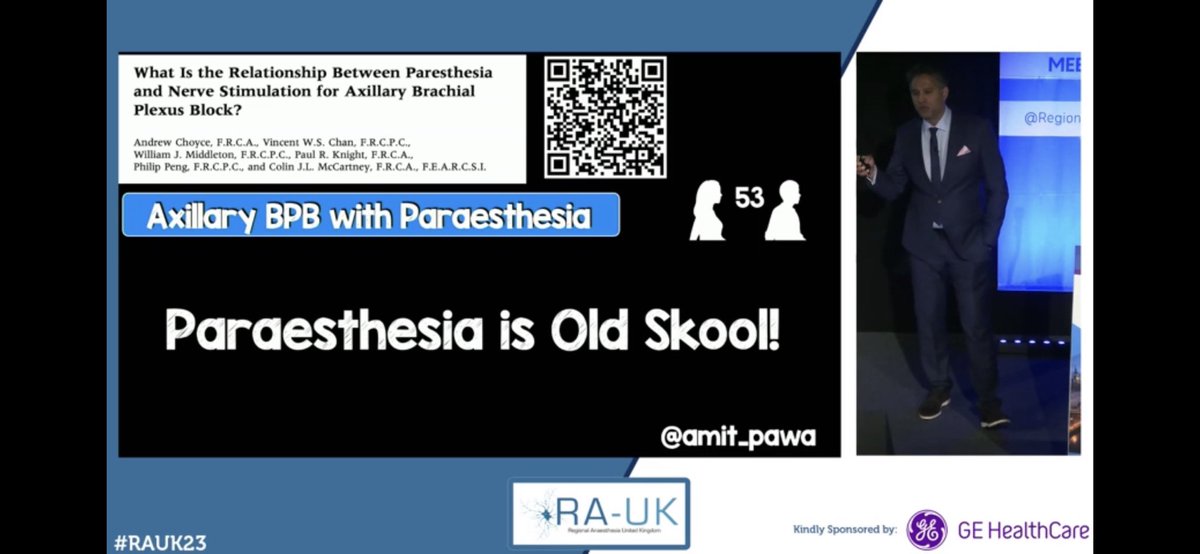
Humans now: Parasthesia is old school (even me an #OBAnes agrees) but parasthesia occurs in absence of twitch, may not detect neural contact. PNS did not prevent intraneural injection. Good solid literature argument from @amit_pawa - definitely negates sensitivity #RAUK23 






Extra points for the Star Wars reference! This is the Way! Mat the fourth be with you #RAUK23 

Addressing the bromance directly - nerve stimulation did not prevent intraneural injection. Still skewering nerves (now I’m hungry) #RAUK23 





@amit_pawa addresses the 6 second claim from @jeffgadsden - if it’s so easy why is it less efficient? #RAUK23 



Does dual guidance prevent harm? Apparently not. Question in my mind is that we know it’s not sensitive, but is that the point? Clearly stimulation is not sensitive enough - but if it’s specific… will @amit_pawa address that? #RAUK23 



Do we need to get that close to the nerve that stimulation would be useful? Can stay 1.6mm away from nerve with effect in 95%. If Yoda says it, I believe it - but literature added as well #RAUK23 







Ah @jeffgadsden quoted again (@ajrmacfarlane this is Kylo Ren from sequel trilogy, Darth Vader’s grandchild IYKYK) Summary of the argument so far - specificity missing? #RAUK23 





Ripping off the stimulator cord does like quite satisfying though #RAUK23 





DO NOT TRY THIS AT HOME! #RAUK23 





Single slide acknowledgement of exceptions - probably wise not to dwell on @jeffgadsden’s 4 pillar Pro argument? #RAUK23 

The moment of truth…
@jeffgadsden not only wins debate, but successfully overturns the pre-debate poll! Well done! But as @amit_pawa pointed out, the patient is the real winner! (And @amit_pawa may have been prejudiced by a few Trekkies in the audience) #RAUK23 

• • •
Missing some Tweet in this thread? You can try to
force a refresh