ATS’ Leadership are in a Kobiyashi Maru situation with #ConferenceGate
- one one hand, they signed a terrible contract and stand to lose a ton of money if they pull out of Orlando
- the other hand, they risk having no one show up & alienating most of their members
#ATSSafe4All
1/
- one one hand, they signed a terrible contract and stand to lose a ton of money if they pull out of Orlando
- the other hand, they risk having no one show up & alienating most of their members
#ATSSafe4All
1/
People are angry. Seeing how many green ribbons there are at ATS, it’s dawning on ATS’ leadership that they screwed up big time.
They wonder: Will these people boycott Orlando 3 times in the next decade? Will they keep paying dues? Is this an existential threat to the org?
2/
They wonder: Will these people boycott Orlando 3 times in the next decade? Will they keep paying dues? Is this an existential threat to the org?
2/
https://twitter.com/khibbert_md/status/1661365076178206720
The easiest move for the EC is to do nothing and (try to) pass the buck: If ATS implodes in 10 years after three disastrously unattended Orlando conferences will anyone remember whose fault it was?
By then EC members will have moved on to other things. Will we remember them?
3/


By then EC members will have moved on to other things. Will we remember them?
3/



But remember, the Koboyashi Maru is a test of character. How do candidates face a no-win situation?
Passing the buck & leaving others to deal w/ the inevitable consequences of their decisions isn’t leadership. It fails the test.
Lead with moral conviction not
spreadsheets.
3/
Passing the buck & leaving others to deal w/ the inevitable consequences of their decisions isn’t leadership. It fails the test.
Lead with moral conviction not
spreadsheets.
3/
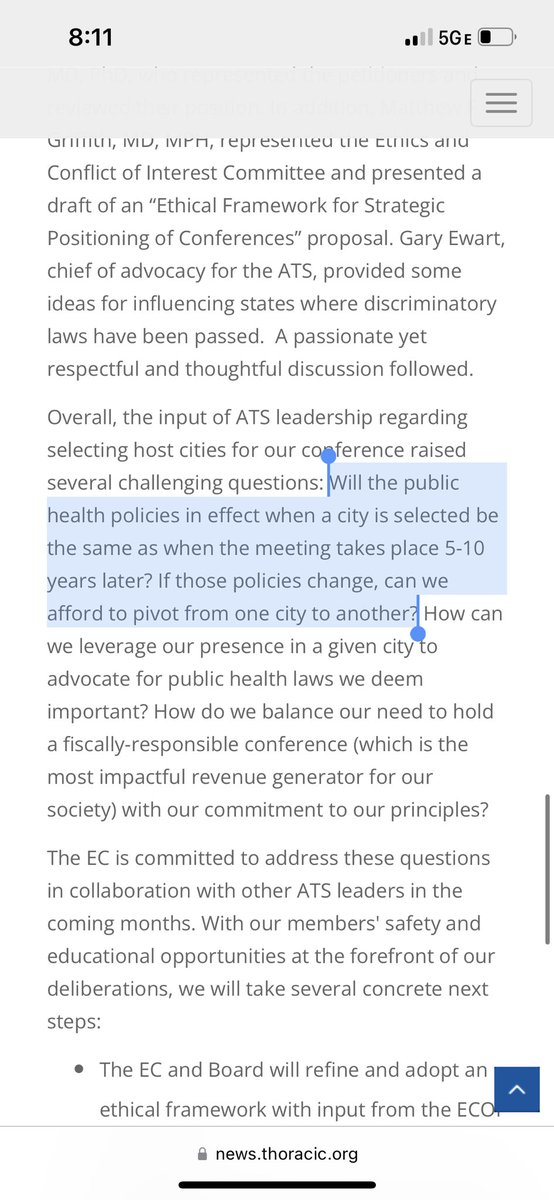
ATS’ Executive Committee should lead by example:
ATS should make it clear they won’t ever hold conferences in places with unjust laws. If NAACP issues travel advisories for FL, the EC shouldn’t be going there.
Lead by setting a moral example. People will remember that.
4/
ATS should make it clear they won’t ever hold conferences in places with unjust laws. If NAACP issues travel advisories for FL, the EC shouldn’t be going there.
Lead by setting a moral example. People will remember that.
4/
https://twitter.com/cnn/status/1660296192692039681
Finally remember that there is no such thing as a no-win scenario.
ATS could fight to get out of the onerous & expensive escape clauses.
ATS could raise money to cover the losses. Solicit donations from members. Hold two smaller ATS conferences/year.
Change the rules & win!
5/
ATS could fight to get out of the onerous & expensive escape clauses.
ATS could raise money to cover the losses. Solicit donations from members. Hold two smaller ATS conferences/year.
Change the rules & win!
5/
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter