Cilta-cel for early relapsed myeloma.
A deep dive-thread where we analyze this trial in incredible detail, all the nuances and subtleties.
Critical appraisal in patient/trainee friendly langauge.
Link to paper:
nejm.org/doi/full/10.10…
#mmsm
#ASCO23
A deep dive-thread where we analyze this trial in incredible detail, all the nuances and subtleties.
Critical appraisal in patient/trainee friendly langauge.
Link to paper:
nejm.org/doi/full/10.10…
#mmsm
#ASCO23
Trial was a comparison of cilta-cel to investigators choice of either dara/pom/dex (86.7% of patients received this) or velcade/pom/dex (12.3% of pts).
Authors write this control arm as "highly effective" standard of care therapy. Was it?
Authors write this control arm as "highly effective" standard of care therapy. Was it?

So unlike the ide-cel study (KARMMA-3), this trial enrolled patients that were not triple refractory (only 15%)- and only 21% of patients were refractory to daratumumab. Only 21% of patients refractory to carfilzomib.
Hence dara or isa + carfilzomib/dex should have been allowed
Hence dara or isa + carfilzomib/dex should have been allowed

What is their excuse for not allowing dara/carfilzomib/dex? See below.
I am not sure I buy this excuse.
This trial started enrolling in July 2020.
Dara/carfilzomib/dex (CANDOR) was presented first at ASH 2019.
Manuscript for CANDOR published in July 2020.

I am not sure I buy this excuse.
This trial started enrolling in July 2020.
Dara/carfilzomib/dex (CANDOR) was presented first at ASH 2019.
Manuscript for CANDOR published in July 2020.

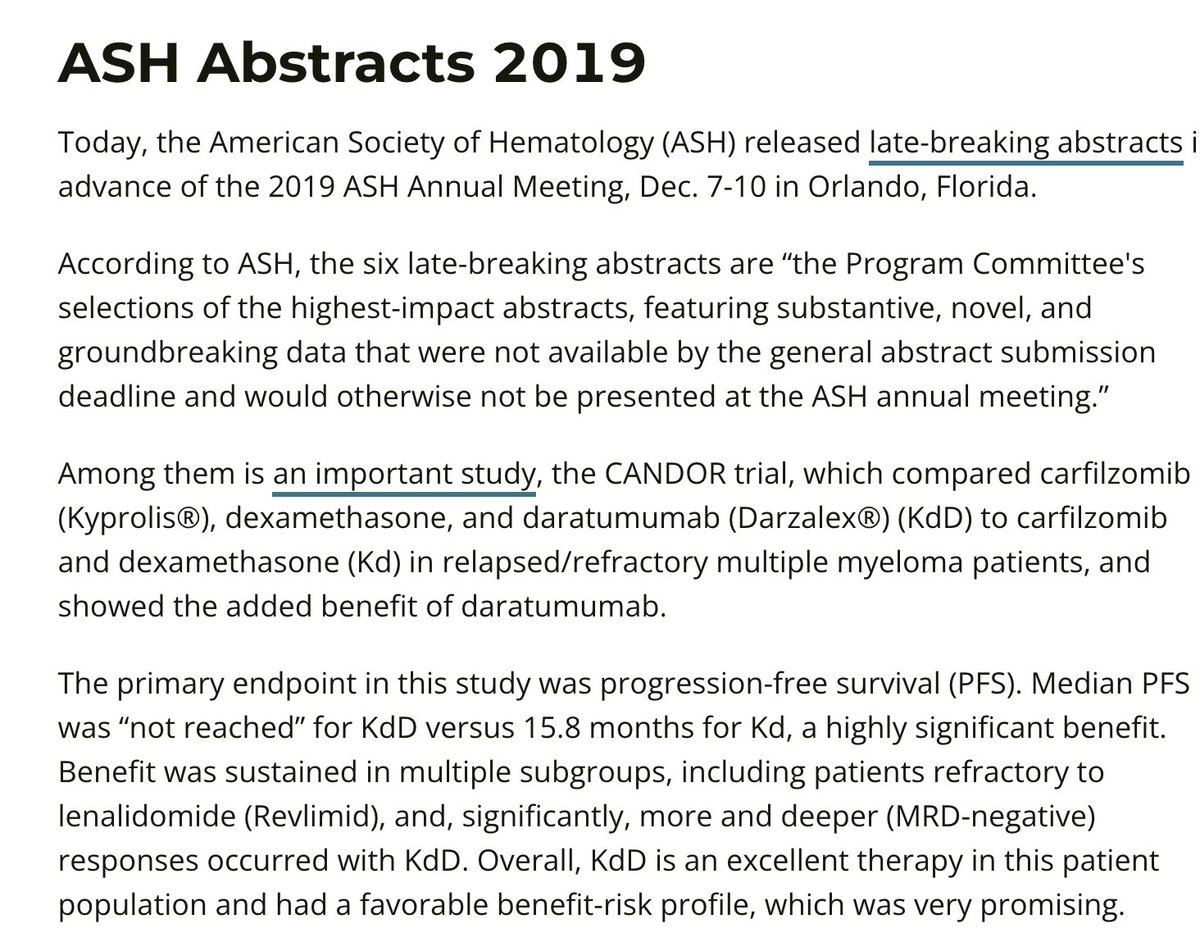
And if this excuse that Janssen uses is true- why is Dara/Carfilzomib/Dex not a control arm for their more recent studies? This is well after regulatory approval for DKd....
Talquetamab trial with dara/pom/dex control arm started to enroll in July 2022
clinicaltrials.gov/ct2/show/NCT05…
Talquetamab trial with dara/pom/dex control arm started to enroll in July 2022
clinicaltrials.gov/ct2/show/NCT05…
So we should call things for what they are.
They didnt want the best control arm, because as much as they believe in their drug (and I believe in their drug too)- they were not sure it could truly beat "best available therapy". And they also wanted "quicker regulatory approval"
They didnt want the best control arm, because as much as they believe in their drug (and I believe in their drug too)- they were not sure it could truly beat "best available therapy". And they also wanted "quicker regulatory approval"
Now that said and done, what was intent of this trial?
The intent of this trial was to confirm regulatory approval for cilta-cel. PFS was an acceptable endpoint for this setting, and this trial has met endpoint.
Its earlier regulatory approval is a success for patients and us!
The intent of this trial was to confirm regulatory approval for cilta-cel. PFS was an acceptable endpoint for this setting, and this trial has met endpoint.
Its earlier regulatory approval is a success for patients and us!
When we try to move a drug already established in a later line of therapy (as cilta-cel was in this case) to an earlier line of therapy- what is the correct endpoint and trial design?
PFS as an endpoint does not account for what happens "after progression".
PFS as an endpoint does not account for what happens "after progression".
You would want to show it is better to give drug earlier rather than later. Not "earlier" versus "never".
PFS doesnt answer question. For such a situation, PFS2 (which accounts for next line of therapy) is ideal.
Cross-over should be built in and offered to control as well.
PFS doesnt answer question. For such a situation, PFS2 (which accounts for next line of therapy) is ideal.
Cross-over should be built in and offered to control as well.
Now unfortunately PFS2 does not have precedence for regulatory approval. But as a field, we should think more about PFS2. One of my favorite trials at ASCO was a PFS2 endpoint trial- first line CDK4/6 inhibition versus second line.
It can be done.
It can be done.
https://twitter.com/oncology_bg/status/1665761318366859265?s=20
I can understand though why PFS was chosen here as endpoint. But i think this brings forward an important lesson in common sense oncology and trial design and hence must be brought up.
There was no cross-over in trial, and details of post-progression therapy not provided 😟
There was no cross-over in trial, and details of post-progression therapy not provided 😟
Thus this trial simply cannot tell us- is early CAR-T better than late CAR-T?
And whether early CAR-T is better than the most effective non-CAR-T therapies currently available?
But it is still a useful and potentially practice changing trial despite these crucial limitations.
And whether early CAR-T is better than the most effective non-CAR-T therapies currently available?
But it is still a useful and potentially practice changing trial despite these crucial limitations.
Lets also look at the inclusion criteria one more time.
For those with measurable M-spike, they mandated a M spike of greater than 1 g/dl.
If your patient progressed, you would have to wait for the M spike to rise all the way up to 1g/dl before they could be enrolled
For those with measurable M-spike, they mandated a M spike of greater than 1 g/dl.
If your patient progressed, you would have to wait for the M spike to rise all the way up to 1g/dl before they could be enrolled
This is a powerful selector for indolent biology.
KARMMA-3 allowed for M spike of 0.5 g/dl for entry.
Even other Janssen trials such as MAJESTEC-3 allowed for M spike of 0.5 g/dl.
To insist on a M spike of 1.0 g/dl for enrollment unfortunately excludes quick progressions
KARMMA-3 allowed for M spike of 0.5 g/dl for entry.
Even other Janssen trials such as MAJESTEC-3 allowed for M spike of 0.5 g/dl.
To insist on a M spike of 1.0 g/dl for enrollment unfortunately excludes quick progressions
It took a median of 44 days from receipt of apheresis to product release, and 79 days from first apheresis to cilta-cel infusion.
Bridging with DPd or PVd was mandated per protocol, so you couldnt get cilta-cel earlier than 4-6 weeks even if you got the product earlier.
Bridging with DPd or PVd was mandated per protocol, so you couldnt get cilta-cel earlier than 4-6 weeks even if you got the product earlier.
Like all randomized trials- this is on an intent to treat basis. So patients who did not get CAR-T but were randomized to CAR-T arm will still be included in denominator. This is very different than earlier phase studies.
To emphasize that point, 32 patients discontinued trial treatment before receiving cilta-cel.
That is 15.3% of patients!
So even though the median PFS accounts for those patients, the really highest risk biology (despite selection filters) never really even got to cilta-cel.
That is 15.3% of patients!
So even though the median PFS accounts for those patients, the really highest risk biology (despite selection filters) never really even got to cilta-cel.

In the control arm, three patients were "not treated- unclear why, and another nine withdrew consent. I assume this is because of unhappiness with being assigned to control arm.
Although this is a small fraction of study (12/211), alot of this can lead to informative censoring
Although this is a small fraction of study (12/211), alot of this can lead to informative censoring
Finally the efficacy results:
PFS endpoint met- not reached for cilta-cel versus 11.8 months for control group.
I am not in business of comparing hazard ratios across trials, so I will not indulge there 😀
PFS endpoint met- not reached for cilta-cel versus 11.8 months for control group.
I am not in business of comparing hazard ratios across trials, so I will not indulge there 😀

What about safety?
10 deaths due to treatment adverse events in cilta-cel, 5 in control (most due to COVID)
Close to 10% incidence of cranial nerve palsies (dont usually see this with ide-cel)
Similar incidence of infections
26% of cilta-cel pts had neutropenia over 30 days
10 deaths due to treatment adverse events in cilta-cel, 5 in control (most due to COVID)
Close to 10% incidence of cranial nerve palsies (dont usually see this with ide-cel)
Similar incidence of infections
26% of cilta-cel pts had neutropenia over 30 days
Overall survival follow-up short but completely overlapping at this point 12 month OS 84.1% with cilta-cel versus 83.6% with control.
Longer follow-up needed, and careful observation of post-protocol therapy and receipt of cilta-cel/other CAR-T in control arm will be needed.
Longer follow-up needed, and careful observation of post-protocol therapy and receipt of cilta-cel/other CAR-T in control arm will be needed.
What does this mean for my practice?
I think that once/if slots capacity improve and manufacturing times shorten, this will be a very attractive option at first relapse. The prospect of one and done treatment really appeals to patients.
I think that once/if slots capacity improve and manufacturing times shorten, this will be a very attractive option at first relapse. The prospect of one and done treatment really appeals to patients.
The most high-risk may never make it to cilta-cel, and were probably not reflected in this study.
For more frail patients, I would prefer longer-follow-up for survival before routinely utilizing this toxic intervention earlier. This is not a benign intervention by any means.
For more frail patients, I would prefer longer-follow-up for survival before routinely utilizing this toxic intervention earlier. This is not a benign intervention by any means.
Most (but not all) neurotoxicities were reversible. One must caution patient about this at time of consent.
2 out of 16 cranial nerve palsies and 2 out of 5 cases of peripheral neuropathy have not resolved with most recent follow-up.
2 out of 16 cranial nerve palsies and 2 out of 5 cases of peripheral neuropathy have not resolved with most recent follow-up.
Janssen and other pharma companies need to reflect carefully about whether it is appropriate to continue to use DPd etc (and not DKD) as control arm.
DPd, DVd and PVd are the new "doublet control" arms of myeloma trials.
Thanks for reading
END.
DPd, DVd and PVd are the new "doublet control" arms of myeloma trials.
Thanks for reading
END.
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter