1/9
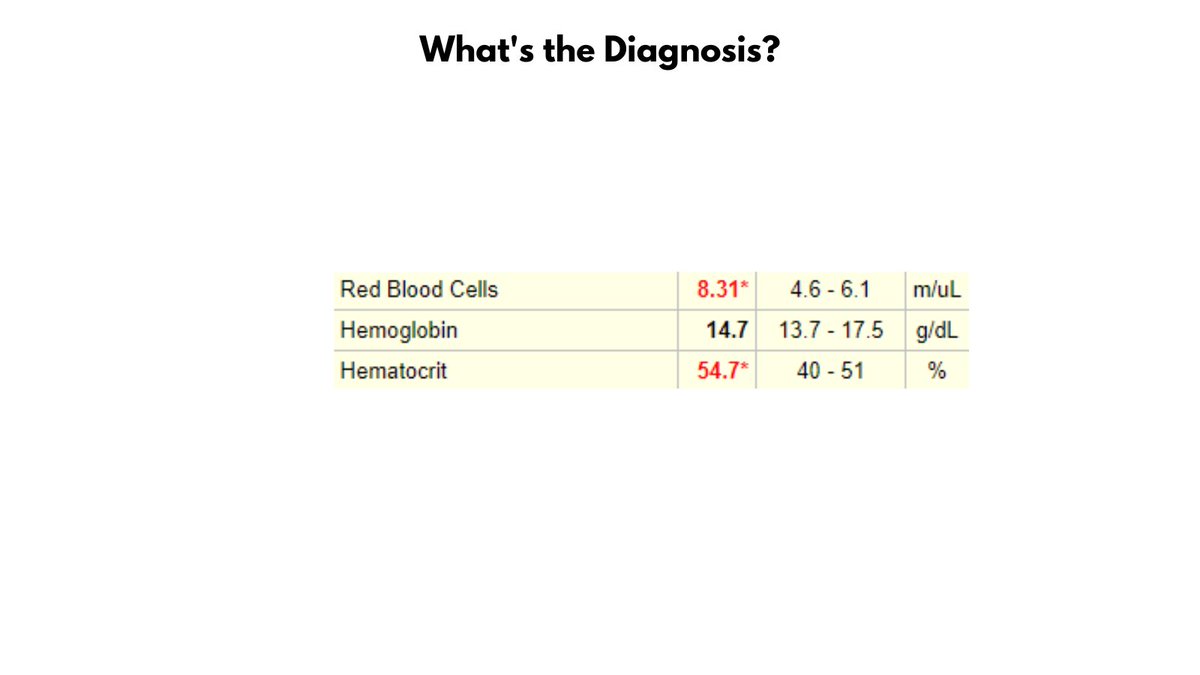
EXAMPLE OF Hb-Hct DISCORDANCE
Take a look at the values in the graphic. Without looking ahead in the thread, can you make a diagnosis?
EXAMPLE OF Hb-Hct DISCORDANCE
Take a look at the values in the graphic. Without looking ahead in the thread, can you make a diagnosis?
2/9
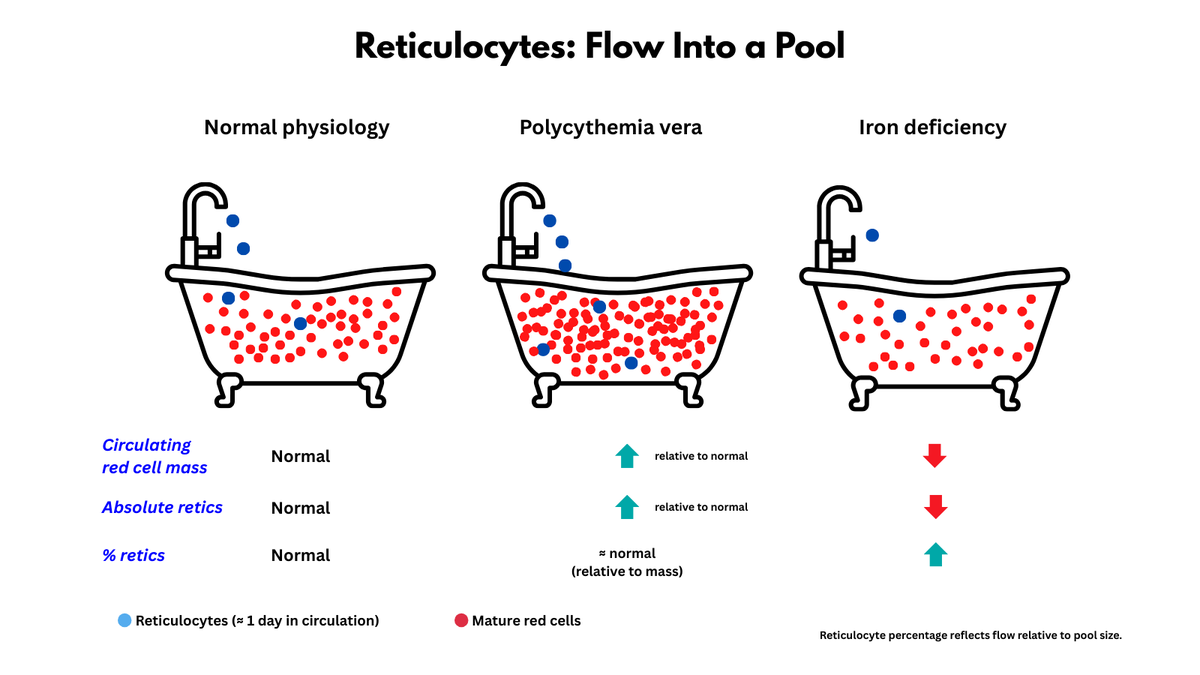
The patient has ERYTHROCYTOSIS (defined as an increased RBC count) and POLYCYTHEMIA (based on the Hct, but not the Hb).
The patient has ERYTHROCYTOSIS (defined as an increased RBC count) and POLYCYTHEMIA (based on the Hct, but not the Hb).

3/9
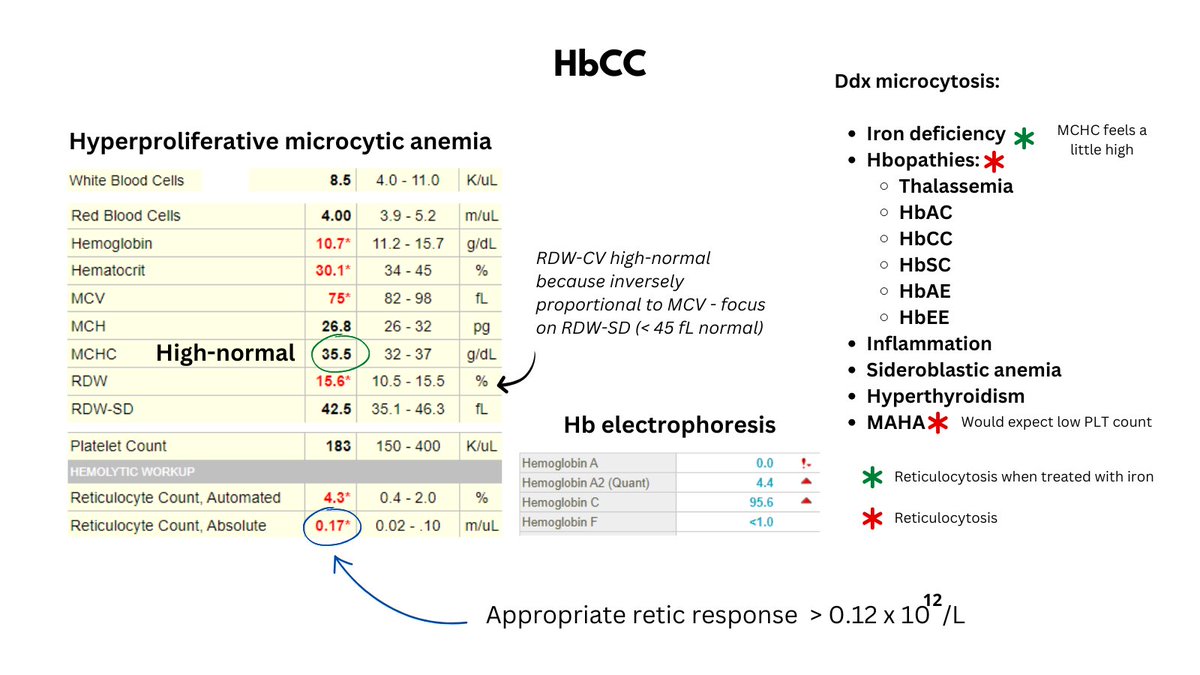
What's up with the elevated Hct but normal Hb? Well, there is violation of the 3:1 rule which states that the Hct is normally 3x the Hb (e.g., Hct 45, Hb 15). Stated another way, the MCHC (Hb/Hct) is low, thus there is HYPOCHROMIA.
What's up with the elevated Hct but normal Hb? Well, there is violation of the 3:1 rule which states that the Hct is normally 3x the Hb (e.g., Hct 45, Hb 15). Stated another way, the MCHC (Hb/Hct) is low, thus there is HYPOCHROMIA.

4/9
We can calculate not only the MCHC but also the MCV (Hct/RBC count). The MCV is only 66 fL, so the patient has non-anemic hypochromic microcytosis.
We can calculate not only the MCHC but also the MCV (Hct/RBC count). The MCV is only 66 fL, so the patient has non-anemic hypochromic microcytosis.

5/9
To summarize, the patient has erythrocytosis, polycythemia (according to Hct), and non-anemic hypochromic microcytosis.
To summarize, the patient has erythrocytosis, polycythemia (according to Hct), and non-anemic hypochromic microcytosis.

7/9
This is a patient with newly diagnosed Jak2 V617F-positive polycythemia vera. Many such patients present with concomitant iron deficiency (from increased Fe demand +/- occult GI bleeding).
This is a patient with newly diagnosed Jak2 V617F-positive polycythemia vera. Many such patients present with concomitant iron deficiency (from increased Fe demand +/- occult GI bleeding).
8/9
It's really interesting to consider that the patient with PV may present with erythrocytosis alone (masked PV), then develop erythrocytosis and polycythemia (+/- iron deficiency) and finally - during a specific window of treatment - polycythemia alone. So cool!!
It's really interesting to consider that the patient with PV may present with erythrocytosis alone (masked PV), then develop erythrocytosis and polycythemia (+/- iron deficiency) and finally - during a specific window of treatment - polycythemia alone. So cool!!

9/9
When considering the Hb and Hct in polycythemia vera, the Hct is the critical parameter because it is the primary determinant of blood viscosity and thrombotic complications. So, the presence of a normal Hb - as in this case - should not provide reassurance!
When considering the Hb and Hct in polycythemia vera, the Hct is the critical parameter because it is the primary determinant of blood viscosity and thrombotic complications. So, the presence of a normal Hb - as in this case - should not provide reassurance!
• • •
Missing some Tweet in this thread? You can try to
force a refresh