1/3
Clinic today was top heavy in iron deficiency. Such interesting histories!
Here is my standard checklist of questions. What else would you add:
1. Symptoms of anemia
2. Symptoms of ID:
2i. Pica
2ii. RLS
2iii. Hair loss
2iv. Brittle nails
2v. Cold intolerance
Clinic today was top heavy in iron deficiency. Such interesting histories!
Here is my standard checklist of questions. What else would you add:
1. Symptoms of anemia
2. Symptoms of ID:
2i. Pica
2ii. RLS
2iii. Hair loss
2iv. Brittle nails
2v. Cold intolerance
2/3
3. History related to causes:
3a. Blood loss:
3ai. Menstrual
3aii. Other bleeding symptoms
3aiii. Frequent blood donation
3b. Malabsorption:
3bi. Gluten sensitivity/abdominal symptoms
3bii. Bariatric surgery
3biii. PPIs
3biv. Helicobacter pylori infection
3biv. PA
3. History related to causes:
3a. Blood loss:
3ai. Menstrual
3aii. Other bleeding symptoms
3aiii. Frequent blood donation
3b. Malabsorption:
3bi. Gluten sensitivity/abdominal symptoms
3bii. Bariatric surgery
3biii. PPIs
3biv. Helicobacter pylori infection
3biv. PA
3/3
3c. Decreased intake
3ci. Vegan/vegetarian diet
3d. Increased demand
3di. EPO administration
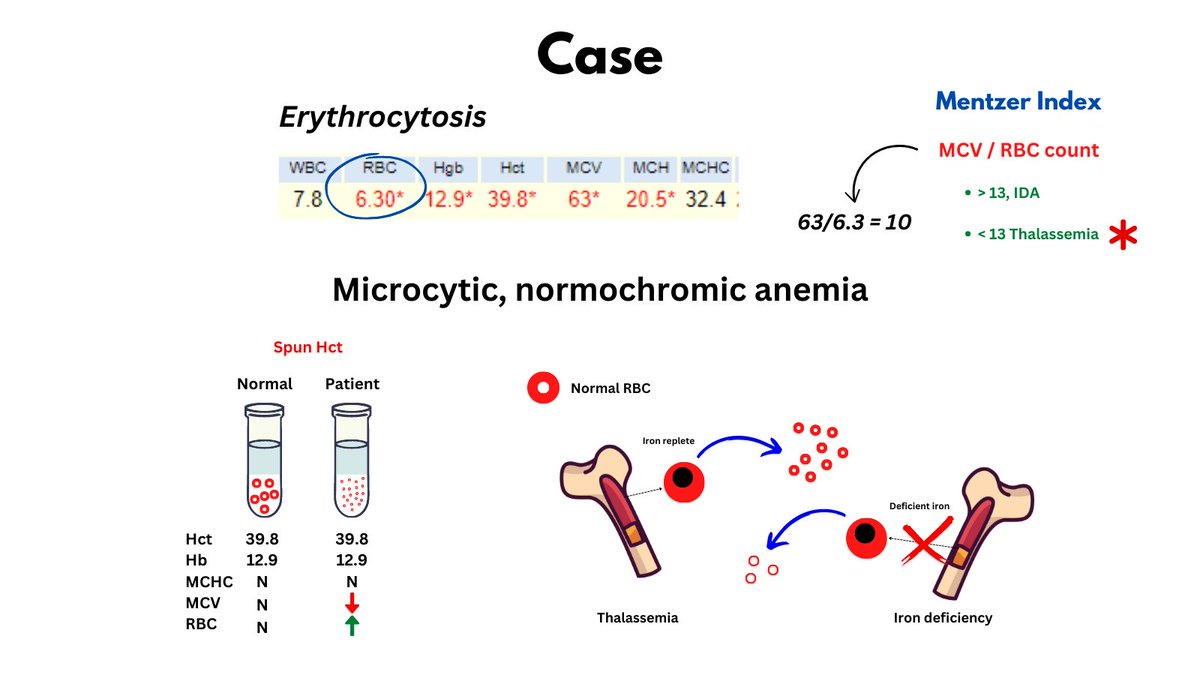
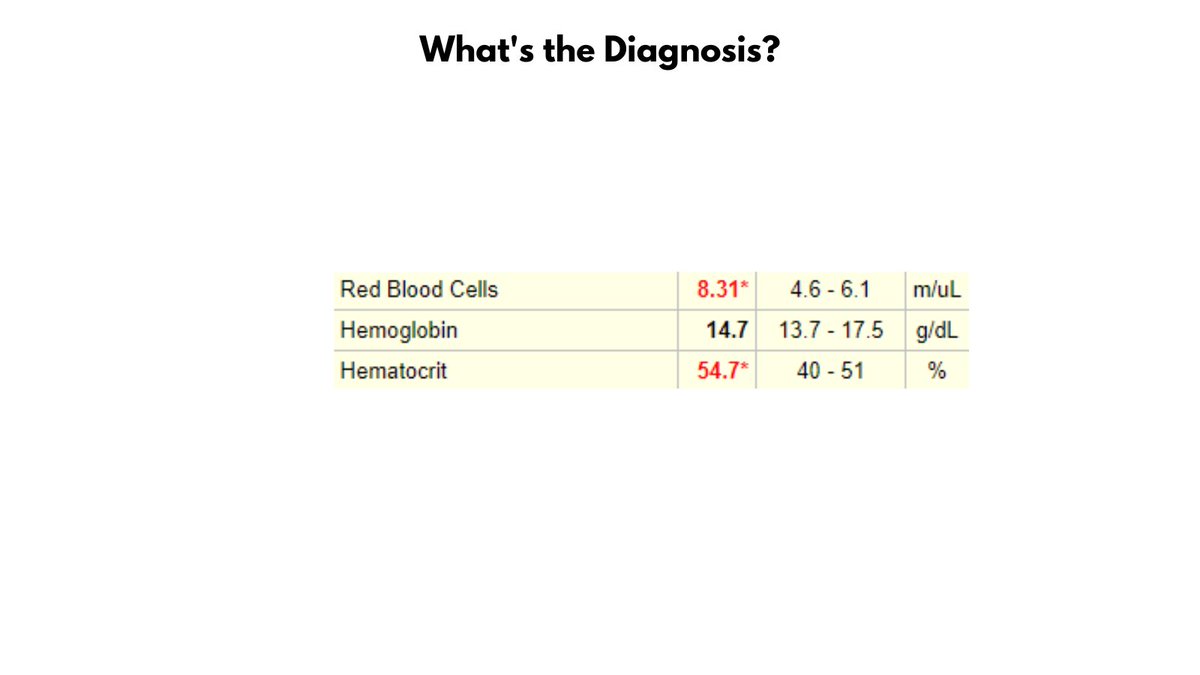
3dii. Polycythemia
... and family history (iron-refractory iron deficiency anemia)
3c. Decreased intake
3ci. Vegan/vegetarian diet
3d. Increased demand
3di. EPO administration
3dii. Polycythemia
... and family history (iron-refractory iron deficiency anemia)
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter