🛑I wrote about what “fatigue” really means for people with long COVID and ME/CFS, and why this profoundly debilitating symptom is so often misunderstood and trivialized.
(This piece also covers PEM.) 1/
theatlantic.com/health/archive…
(This piece also covers PEM.) 1/
theatlantic.com/health/archive…
First, an important note. I’ve been told that this piece will be free to read for 24 hours, but will then go behind the paywall. Best I could do. If you’re not a subscriber and this is useful to you or your loved ones, I’d suggest saving a copy ASAP. 2/ theatlantic.com/health/archive…
When long-haulers talk about their fatigue, they often hear “Oh I’m tired too”. But theirs is utterly different to the everyday version healthy people get. More severe. Very hard to push through (& costly if you try). Not cured by sleep. Multifaceted. 3/ https://t.co/yqZoRGtyxAtheatlantic.com/health/archive…



Post-exertional malaise—the cardinal symptom of ME/CFS—is distinct & worse. Less a symptom than a physiological state. After gentle physical/mental activity, your batteries aren’t drained but missing entirely. PEM is the annihilation of possibility. 4/ https://t.co/sJpE2OA5zhtheatlantic.com/health/archive…



PEM *can* be objectively measured, and yet is often dismissed because it so thoroughly inverts the dogma that exercise is good for you & you should push through ill health. Here, doing that can make you much worse. 5/ https://t.co/2VG6e06ISztheatlantic.com/health/archive…



Why this dismissal? This piece offers a brief cultural history, but there are three main factors—reductionism, sexism, and capitalism—all blending together into a cocktail of stigma. 6/ https://t.co/iCxQzRCy3ytheatlantic.com/health/archive…





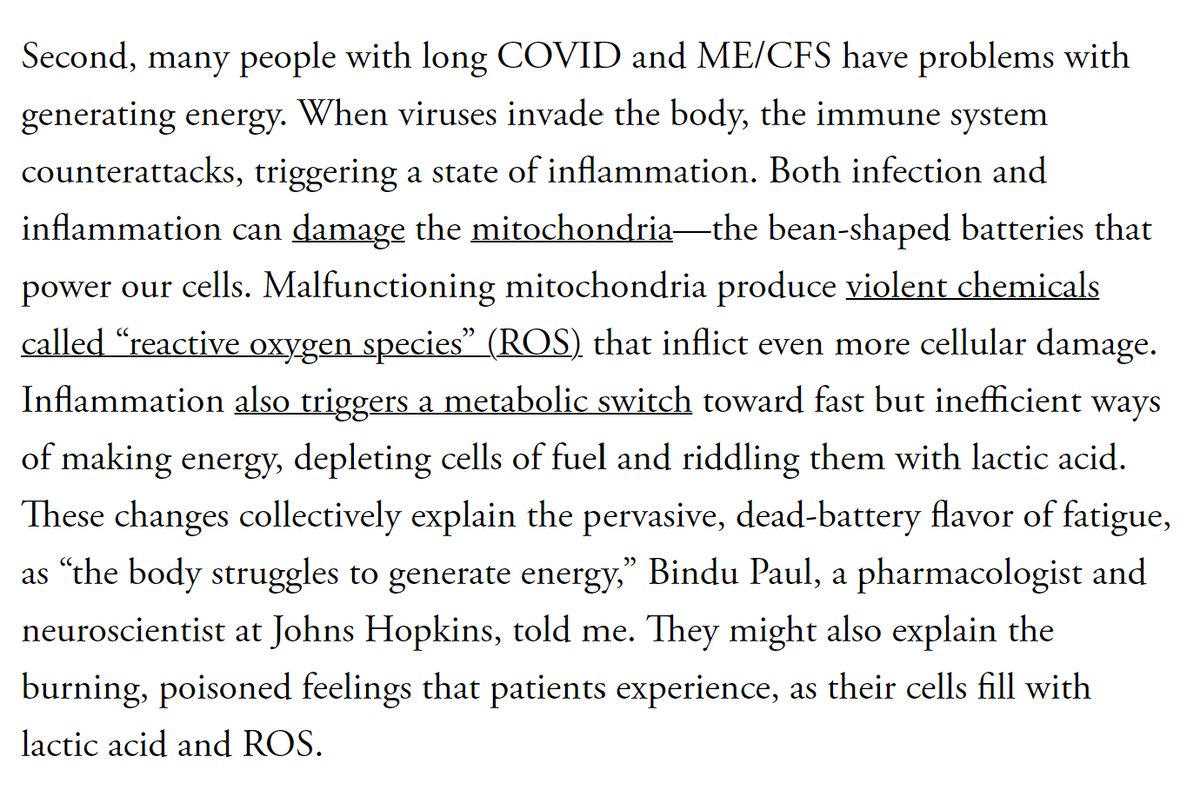
Contrary to popular belief, long COVID & ME/CFS are not mystery diseases. There’s plenty of evidence for at least two major pathways that might cause extreme fatigue and PEM--one neurological, one metabolic. 7/ https://t.co/qjdxMcfBVPtheatlantic.com/health/archive…



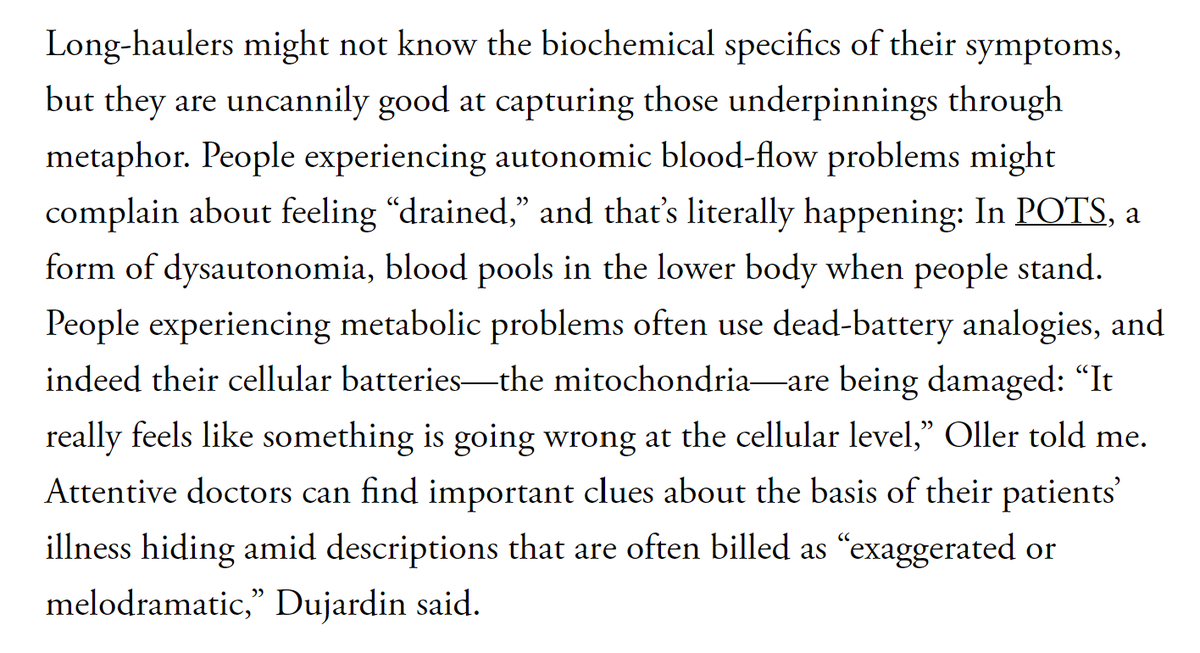
Note also that long-haulers might not know the biochemical specifics of their symptoms, but are uncannily good at capturing those underpinnings through metaphor. As ever, patients are the most important sources of knowledge. 8/ https://t.co/U0kqkV1urMtheatlantic.com/health/archive…

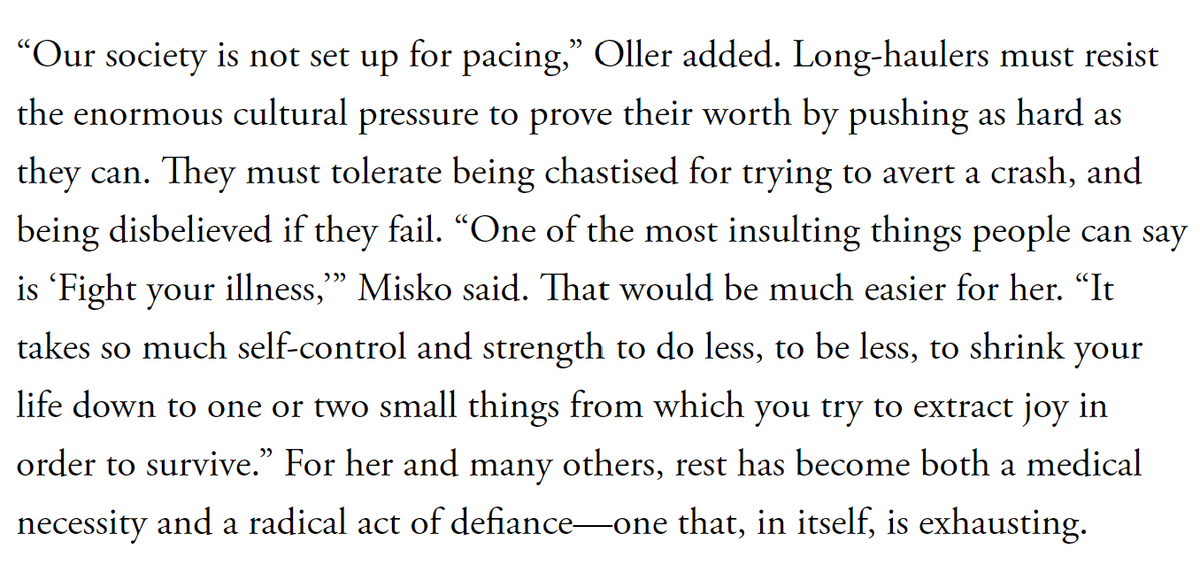
There’s no easy way out of this. Most treatments are about symptom management. Pacing—a strategy for keeping your activity levels below the levels that cause debilitating crashes—is crucial, but also very hard esp since our society isn’t set up for it. 9/ https://t.co/iyrXiQiPsztheatlantic.com/health/archive…



People with long COVID and ME/CFS face *so much* disbelief. But the reality and severity of their experiences is so obvious if you actually talk to them, supported by the scientific literature, and deserving of empathy and support. 10/ theatlantic.com/health/archive…
The fatigue piece is intended as a companion to last year’s one on brain fog. They’re both biographies of deeply misunderstood symptoms. I wanted to do them back to back but life got in the way. I’m glad both now exist, and I hope they help. 11/ theatlantic.com/health/archive…
Oh and I have recorded an audio version of the fatigue piece for people whose symptoms make it hard to read long pieces. There's some processing to do which is out of my hands but I hope it goes up later today. End/
PS: Just so everyone who sees this thread is aware of this standing offer:
https://twitter.com/edyong209/status/1684592883280842752
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter



