1/ Tweetorial on @abiomed Impella position (crucial for function and prevention of complications). Recently we summarized a practical algorithm for pVAD position that we developed @UZBrussel and published @ESC_Journals academic.oup.com/ehjacc/advance…
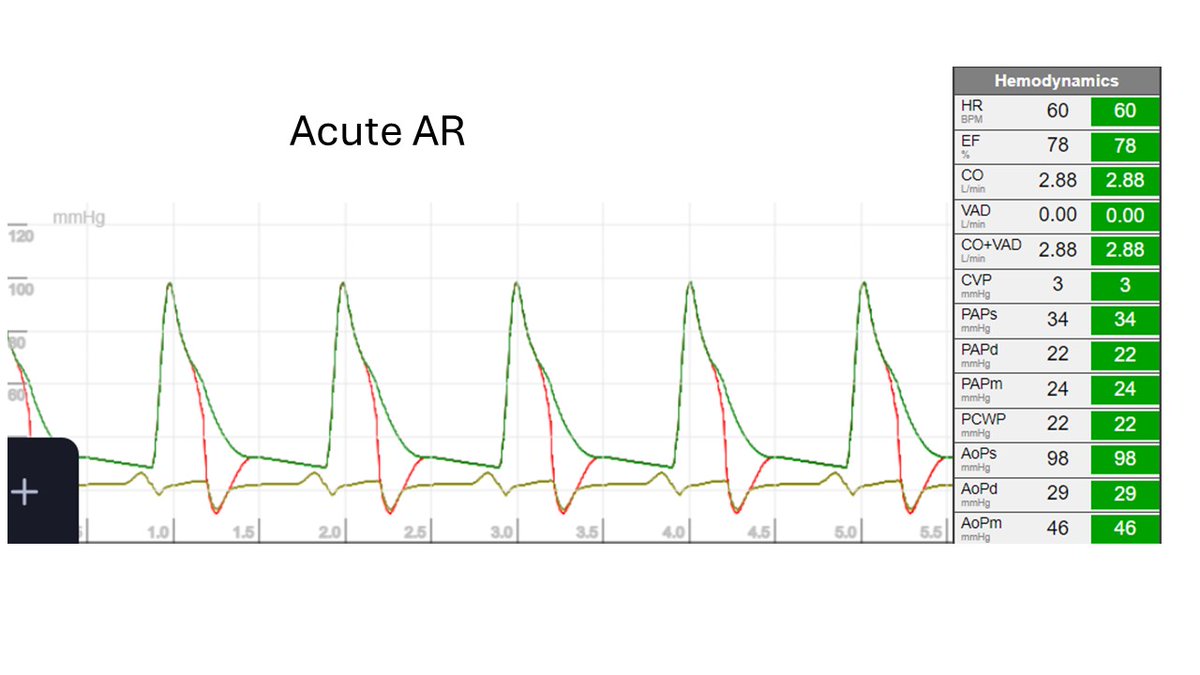
2/ The main problem with pVAD malposition is contact between outlet and AoV or the inlet with LV structures, leading to hemolysis or suction events (decreases support). Recently we published in detail on hemolysis (open access): 10.1080/17434440.2022.2108319
3/ Basically, there are two important axes to evaluate the position: a) insertion depth; b) the rotation. a) is well known, b) has recently gained more attention thanks to @lucabaldetti et al. (a subset of mal-rotation patients), () jacc.org/doi/abs/10.101…

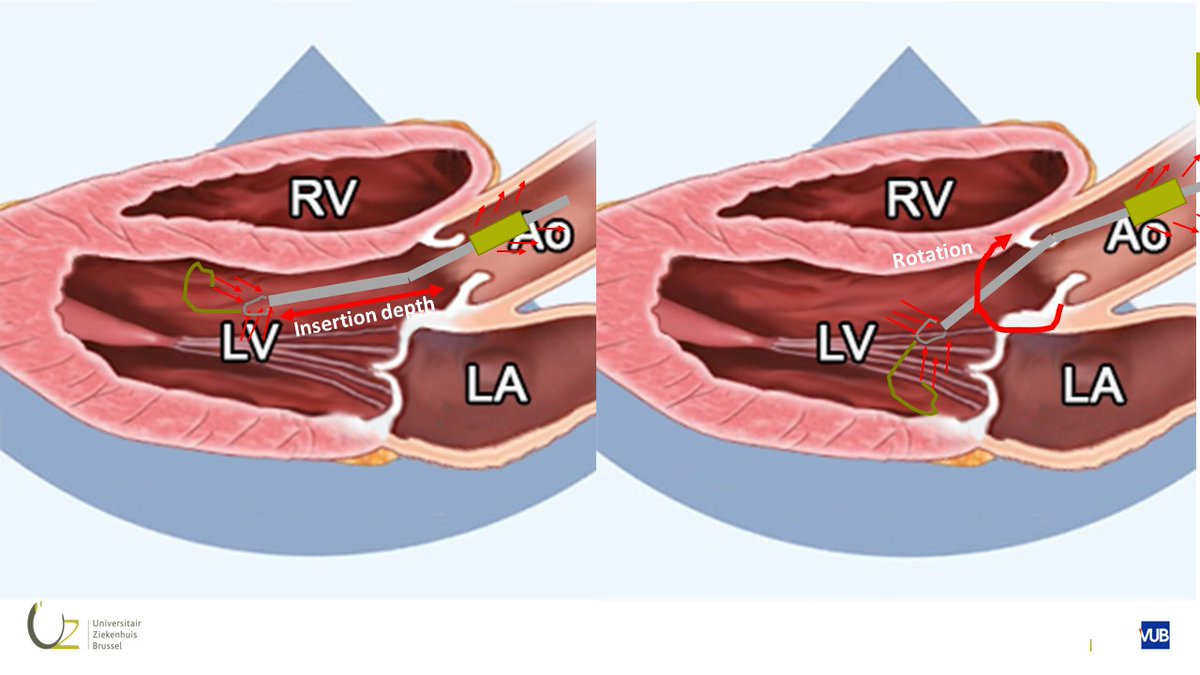
@lucabaldetti 4/ To evaluate the position of a pVAD at the bedside we have 2 tools: a) echocardiography and b) the console. These are complementary. Echocardiography mainly focuses on the inlet position. True inlet = interruption in lines; end of inlet cage = “teardrop” (paper contains videos) 

@lucabaldetti 5/ The console displays waveforms that are important. A) green = motor current (+/- flow). B) Red = measured aortic pressure at outlet C) White = calculated LV pressure. These change with malposition. 

@lucabaldetti 6/ When inlet and outlet are in one chamber->motor current becomes flat = no changes in pressure head (Pout-Pin) during cardiac cycle. You can imagine that an LV pressure at the outlet means over-insertion. When the pVAD is completely out of the LV, calculated LVP looks like AoP 
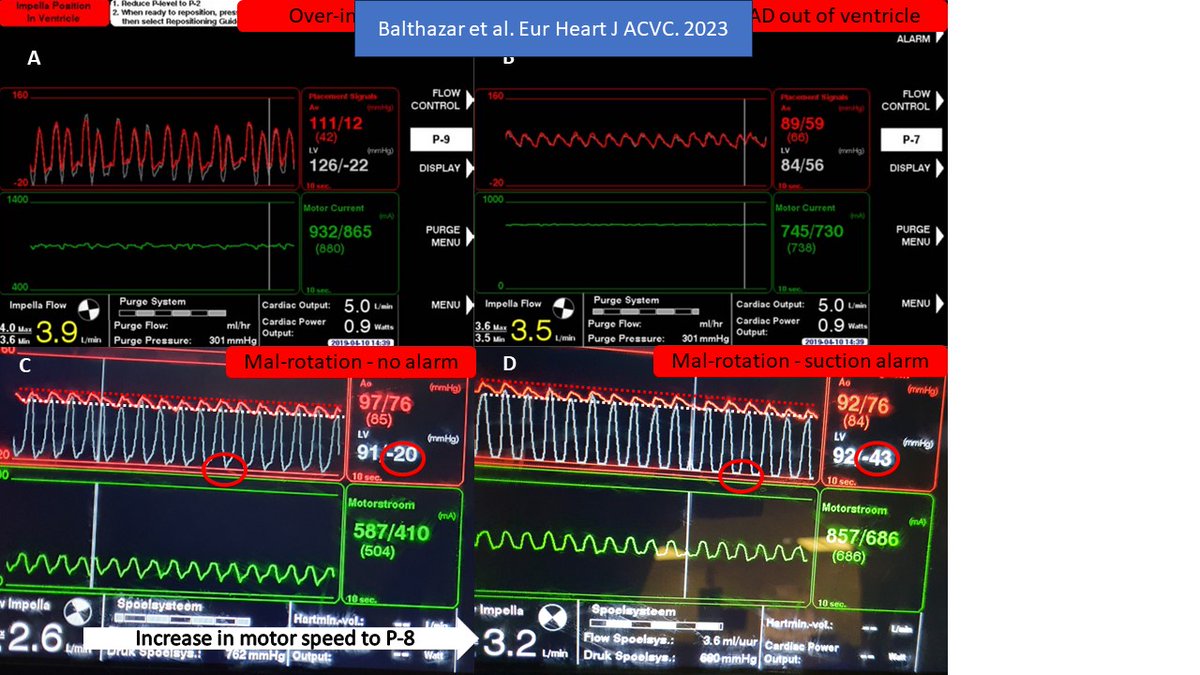
@lucabaldetti 7/ A major advance in pVAD management is the Smart Assist® technology that continuously displays a calculated LV waveform. The weakness of this waveform is that is calculated, which is actually its strength when evaluating pVAD position.
@lucabaldetti 8/ Simplified, the device calculates this pressure assuming that for a given motor current (which is a measure of flow), there is a certain pressure head (H) (Poutlet-Pinlet). Since Pout is aortic pressure, it can calculate the LV Pressure from this pressure head.
@lucabaldetti 9/ If something interferes with flow, the reduced flow is interpreted as reduced H, lowering “LVP” When decreased LV preload (ie, hypovolemia or RV failure) causes suction alarms, those manifest in diastole! @Babar_Basir et al. have shown relationship of diastolic suct and RVF 
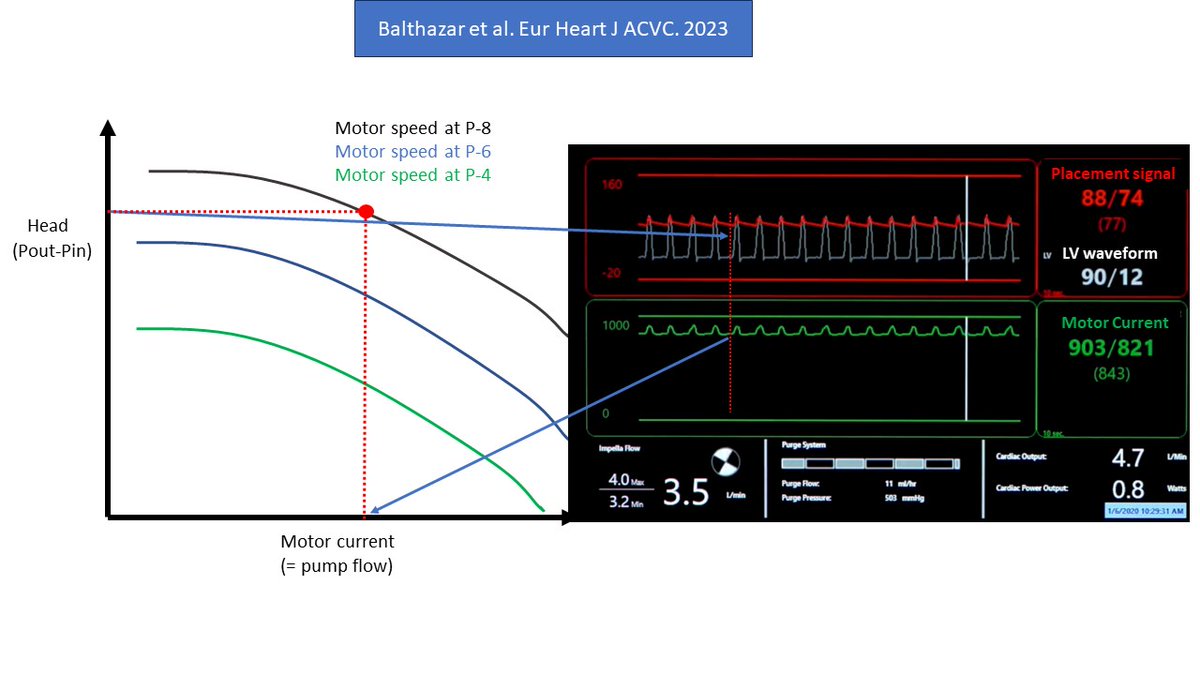
@lucabaldetti @Babar_Basir 10/ If the device is in an abnormal position the LV pressure will CONTINUOUSLY (= systole+diastole) be lower than aortic systolic pressure (impossible in a pulsatile situation where the aortic valve opens). If you learn to recognize this, you can even anticipate suction!! 
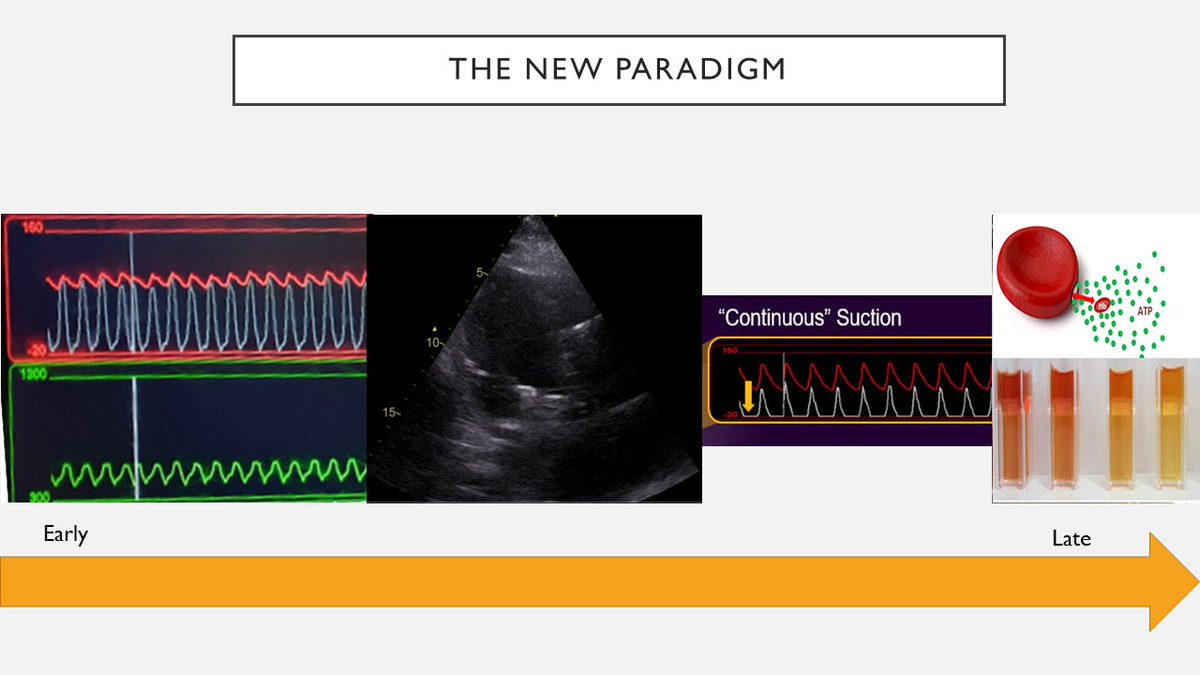
@lucabaldetti @Babar_Basir We summarized this information in an easy to use algorithm. In our practice, it proved helpful to prevent suction events. Of course we hope to prove this with data! 

@lucabaldetti @Babar_Basir 12/ Resolving malposition is easy if the problem is insertion depth. One can pull back or push, as long as there is no complete dislocation. Abnormal rotation is more difficult, but sometimes torque is possible, especially for axillary pVAD’s (the new 5.5 is very well torque-able 

@lucabaldetti @Babar_Basir 13/ If interested, please read the paper that contains much more detail and figures/video's. Thanks to the fantastic team @FH_Verbrugge @drnvanmieghem @InesVanloo @RaesMatthias
@iceman_ex @EHJACVCEiC @nickmmark @DrSethdb @VerwerftJan @Cosyns @jsemccm
@iceman_ex @EHJACVCEiC @nickmmark @DrSethdb @VerwerftJan @Cosyns @jsemccm
• • •
Missing some Tweet in this thread? You can try to
force a refresh