🔥🔥🔥 Hey #GIonc #Radonc friends- rectal cancer management is evolving rapidly. Let’s run through a case-based review of rectal cancer!!!
#ASTRO23


#ASTRO23


55F
cT3aN0M0 rectal adenocarcinoma, pMMR
11 cm from the anal verge
No compromise of the mesorectal fascia or evidence of extramural venous invasion
Patient is amenable to low anterior resection
What would you recommend for management?
cT3aN0M0 rectal adenocarcinoma, pMMR
11 cm from the anal verge
No compromise of the mesorectal fascia or evidence of extramural venous invasion
Patient is amenable to low anterior resection
What would you recommend for management?
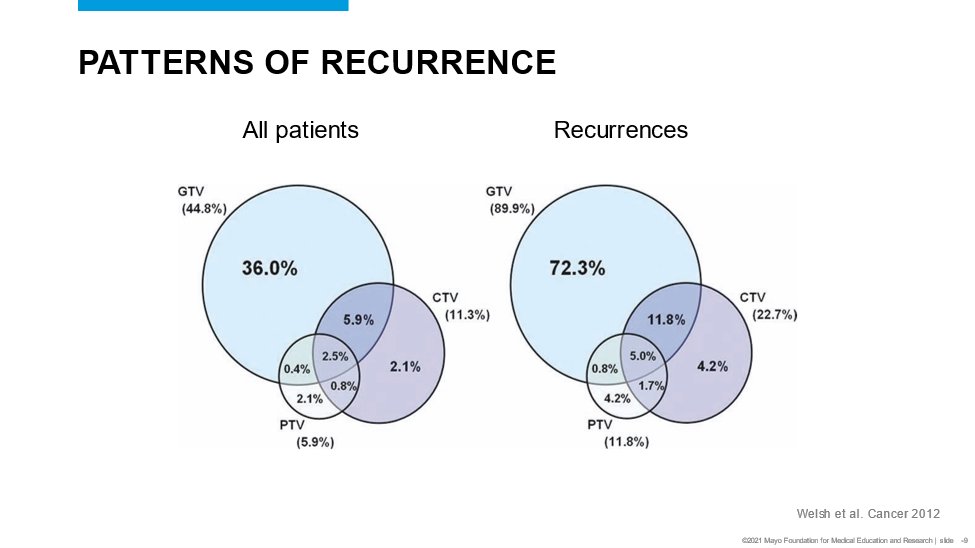
✅Pre-operative RT reduces the risk of pelvic recurrence for patients managed surgically for rectal cancer.
But some patients will suffer from acute and long term toxicity (bladder, bowel, sexual, endocrine dysfunction)
Do all patients derive benefit?
But some patients will suffer from acute and long term toxicity (bladder, bowel, sexual, endocrine dysfunction)
Do all patients derive benefit?

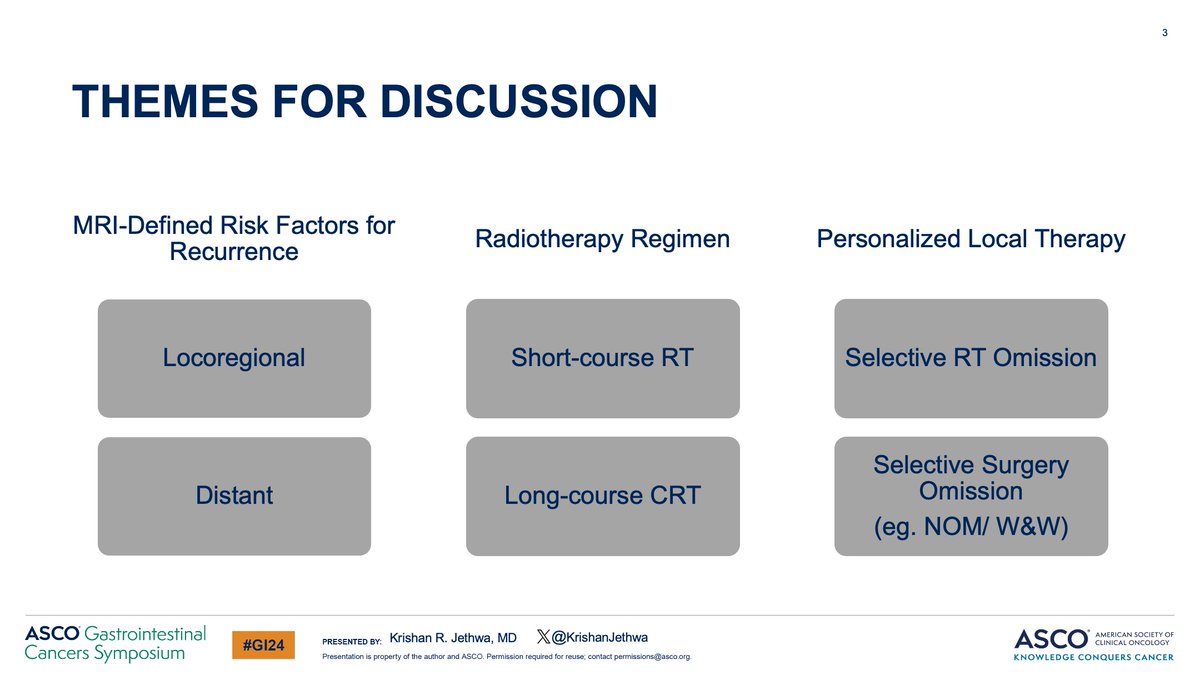
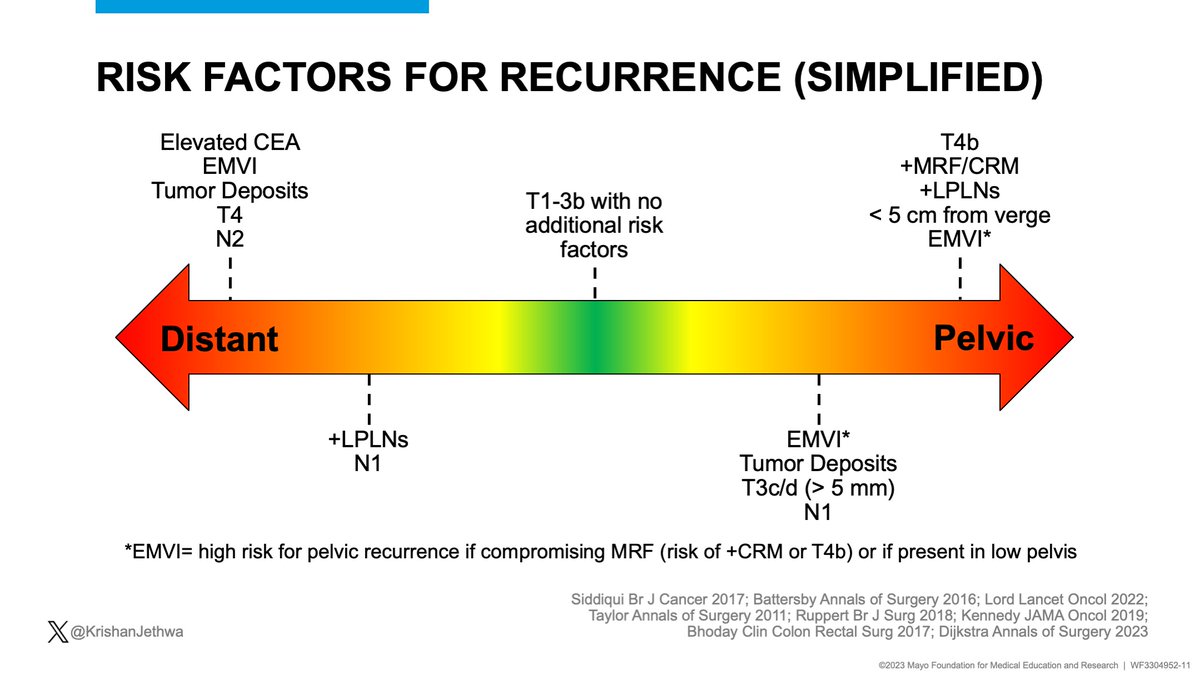
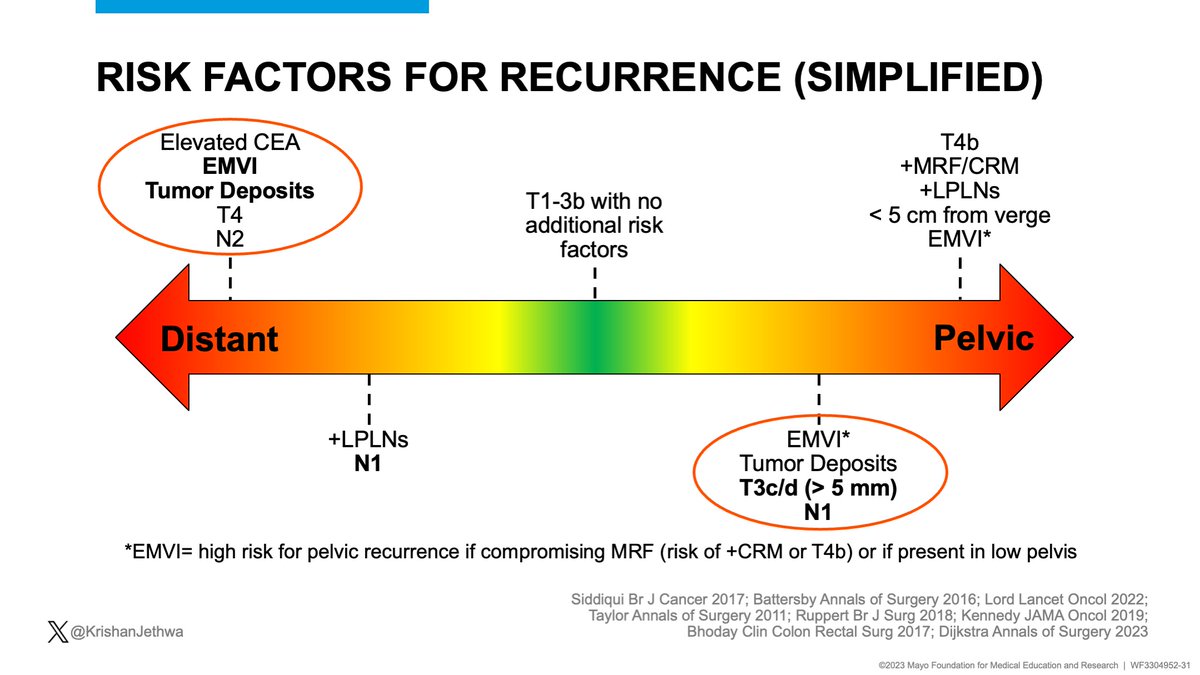
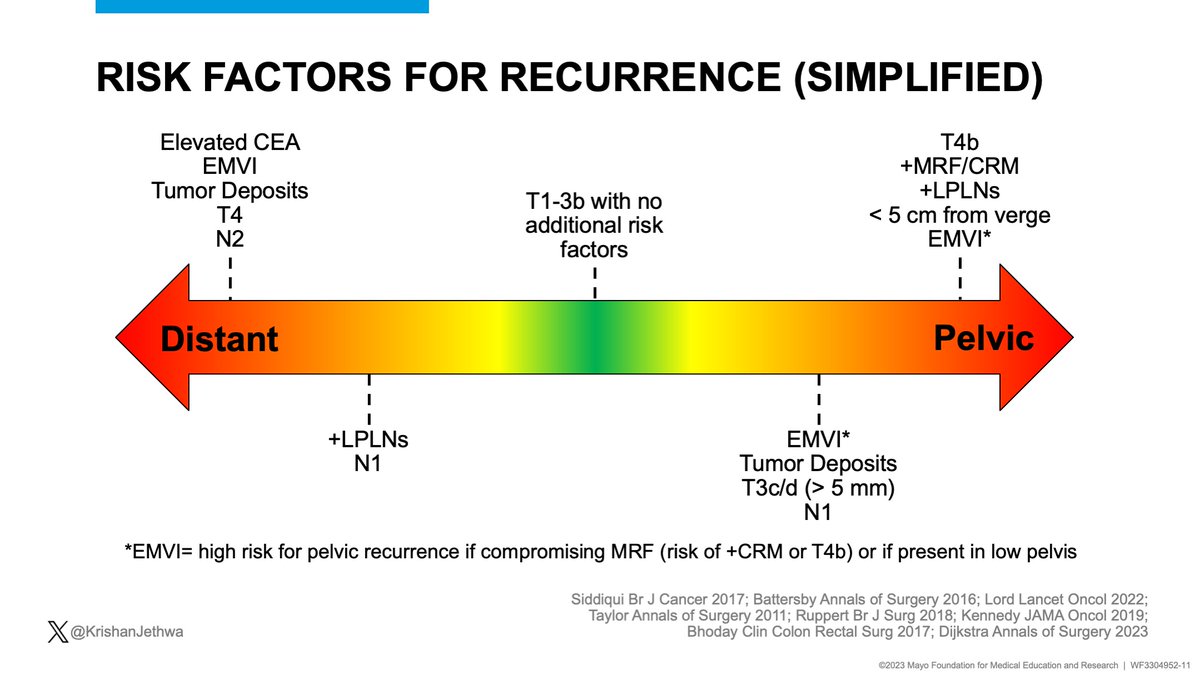
Rectal cancer is highly heterogeneous with a broad spectrum of risk for both pelvic and distant recurrence.
🔥🔥🔥 Understanding risk of recurrence is critical in clinical decision making!
This patient had favorable risk disease.
🔥🔥🔥 Understanding risk of recurrence is critical in clinical decision making!
This patient had favorable risk disease.
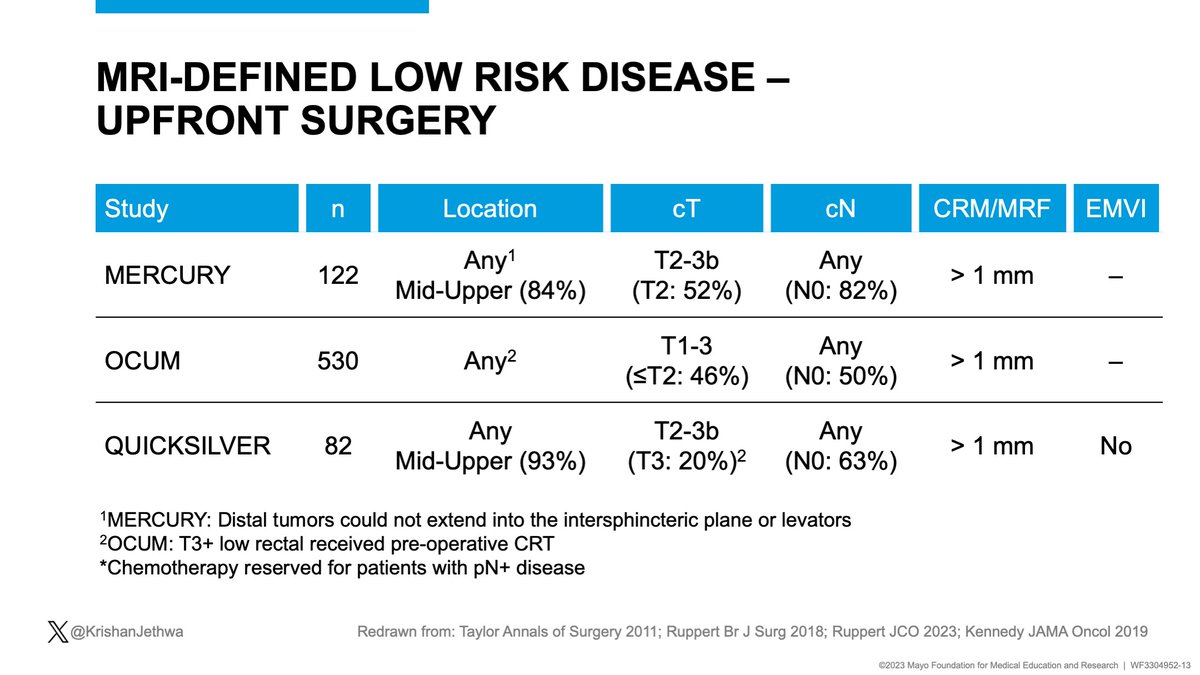
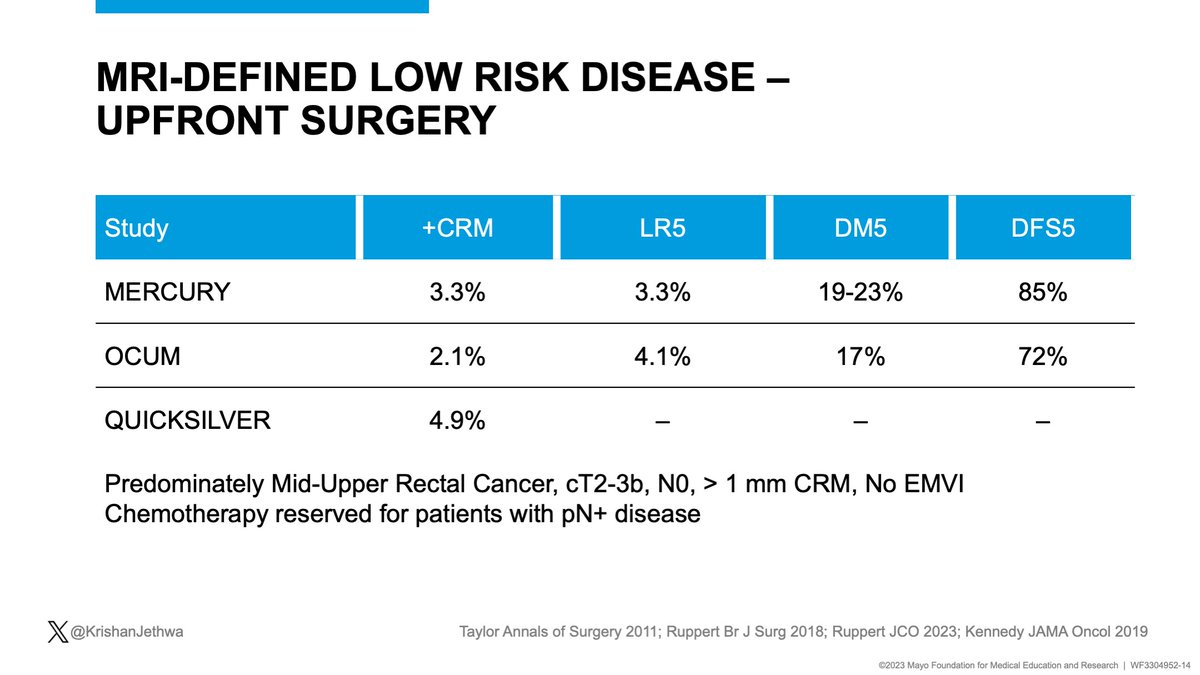
Mercury, OCUM, and Quicksilver included patients with predominately mid-upper rectal cancers, T2-3bN0, clear MRF, and per Quicksilver- no EMVI
Patients treated with up-front surgery
Chemotherapy only for pN+ patients
✅ < 5% + margins
✅< 5% 5-year pelvic recurrence


Patients treated with up-front surgery
Chemotherapy only for pN+ patients
✅ < 5% + margins
✅< 5% 5-year pelvic recurrence
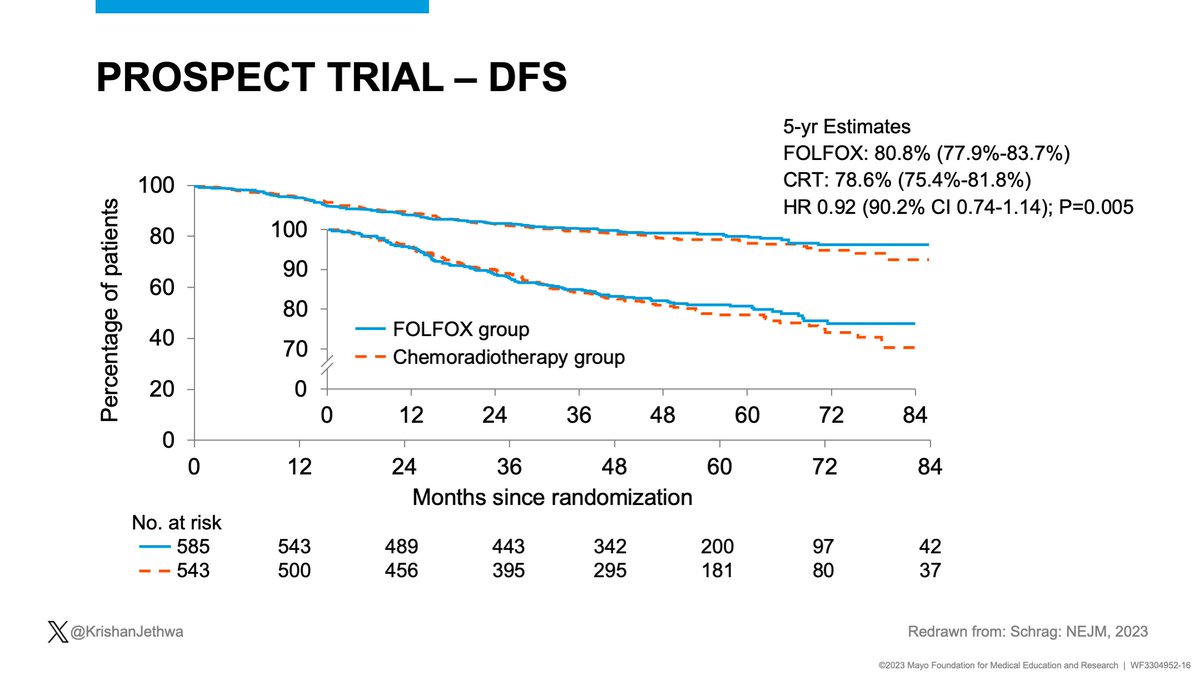
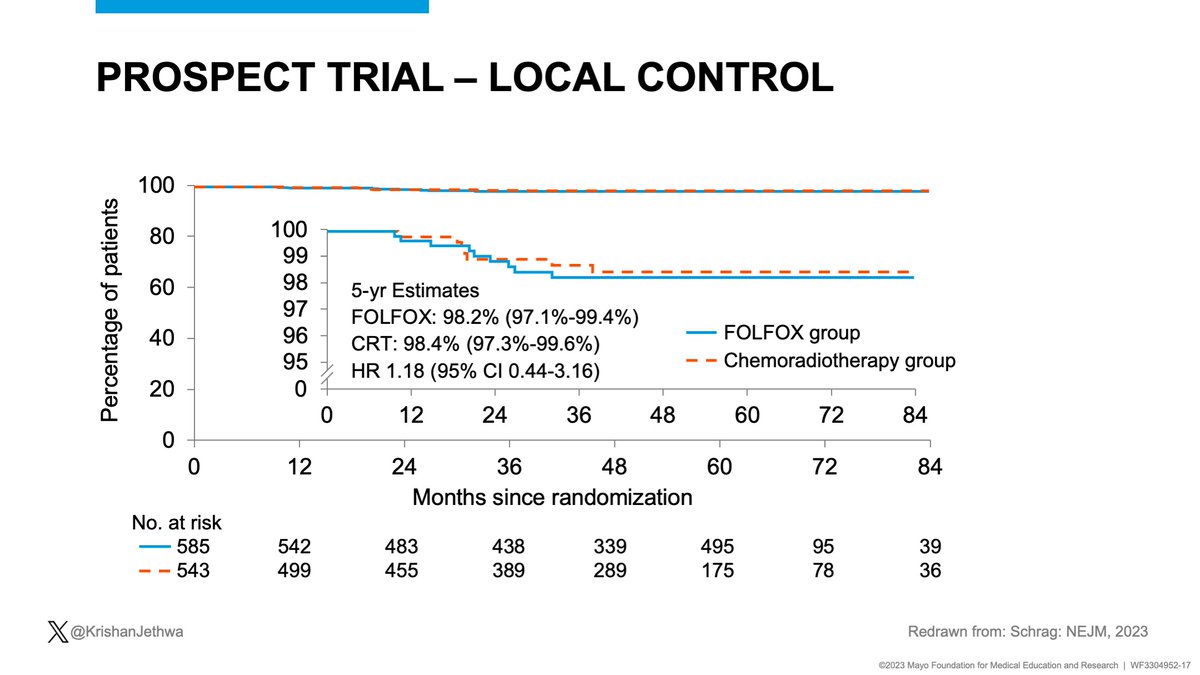
For pts with favorable risk cT3N0-1/cT2N1 rectal cancer amenable to LAR, PROSPECT compared:
LC-CRT
vs
Pre-op chemo +/- selective CRT
Study found no detriment in:
✅Local control
✅Disease free survival
✅Overall survival
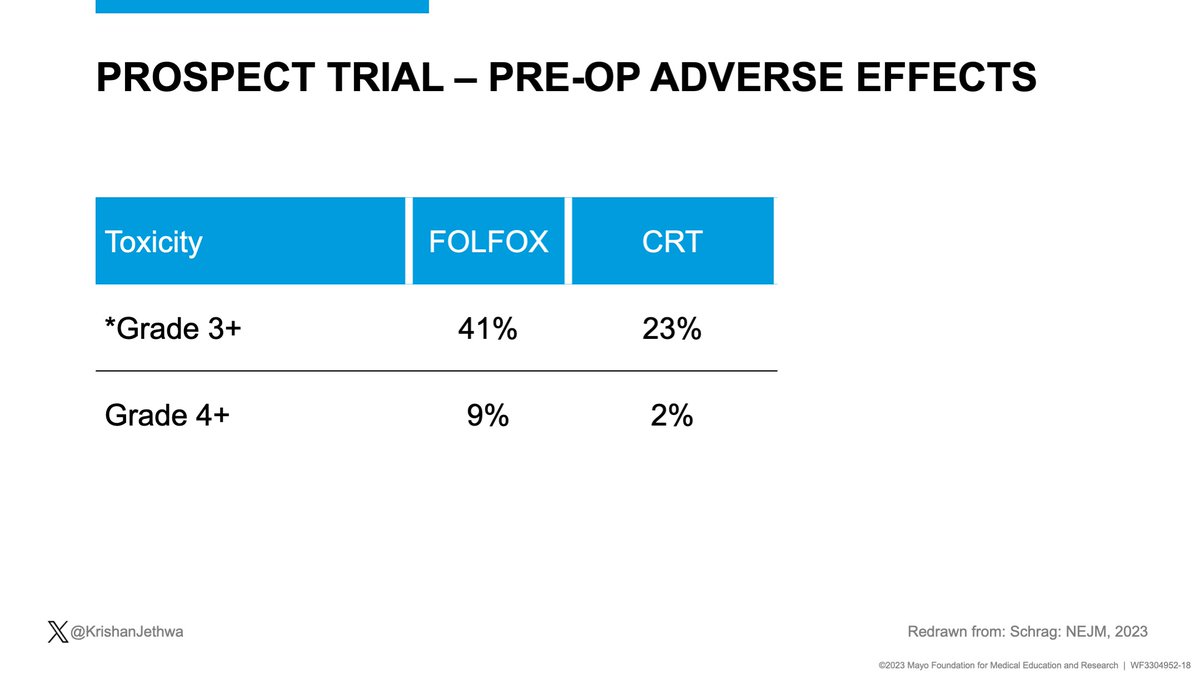
BUT
🔺 pre-op toxicity with FOLFOX




LC-CRT
vs
Pre-op chemo +/- selective CRT
Study found no detriment in:
✅Local control
✅Disease free survival
✅Overall survival
BUT
🔺 pre-op toxicity with FOLFOX
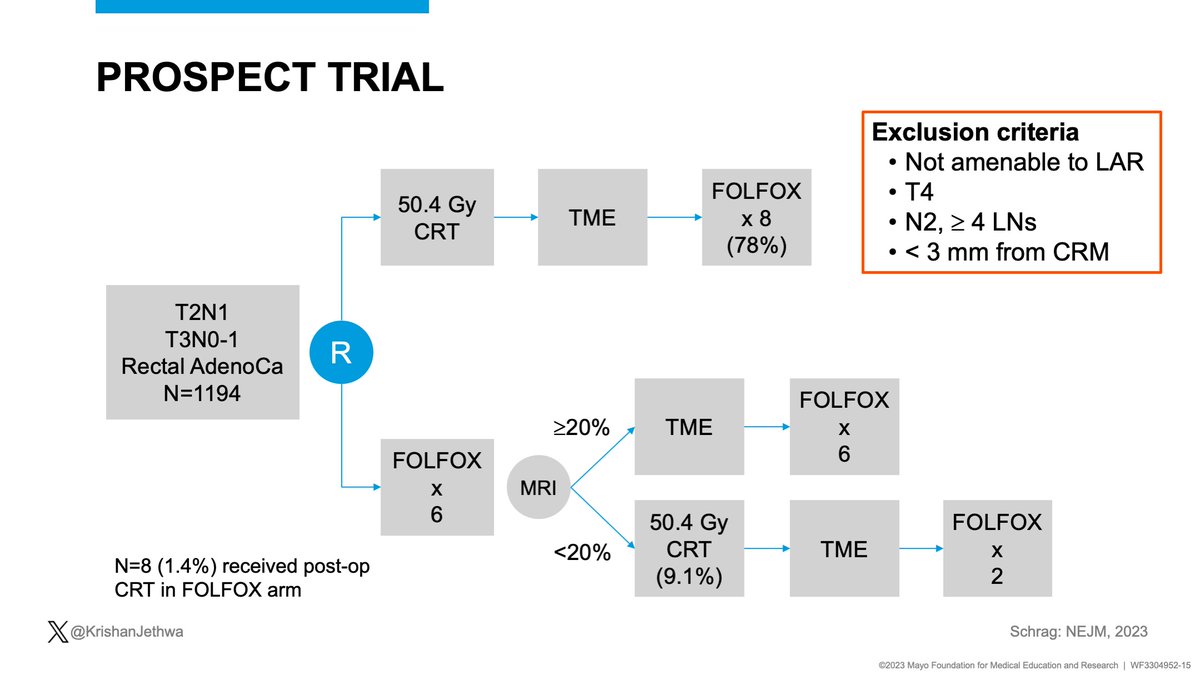
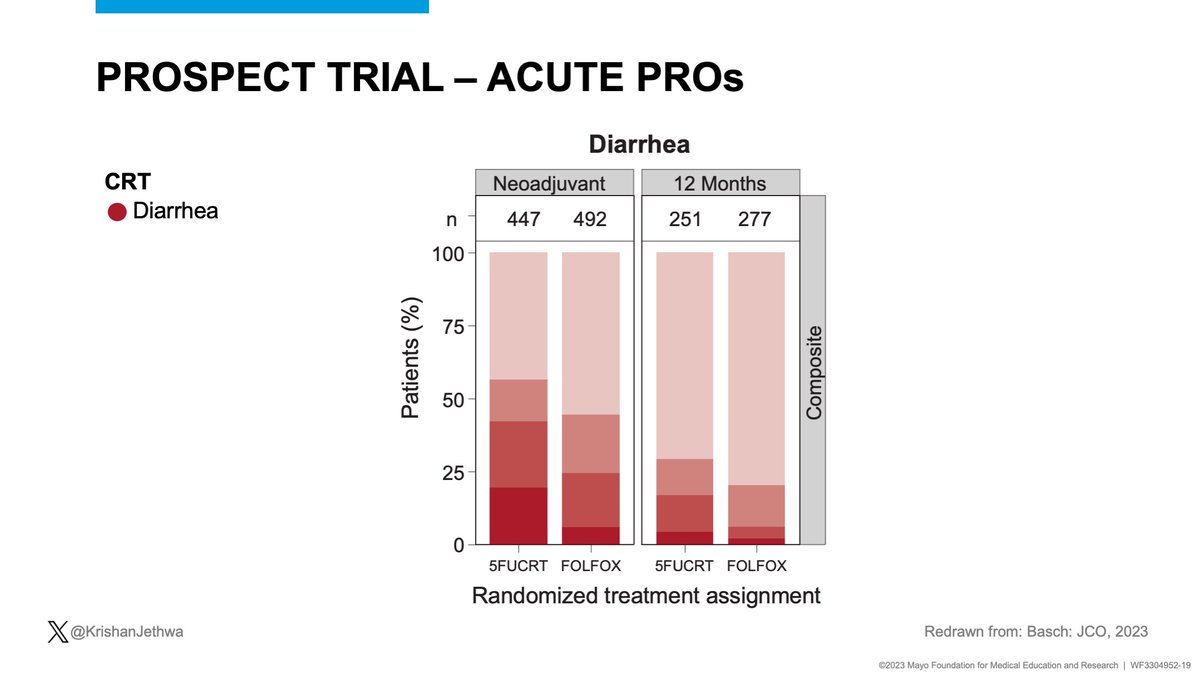
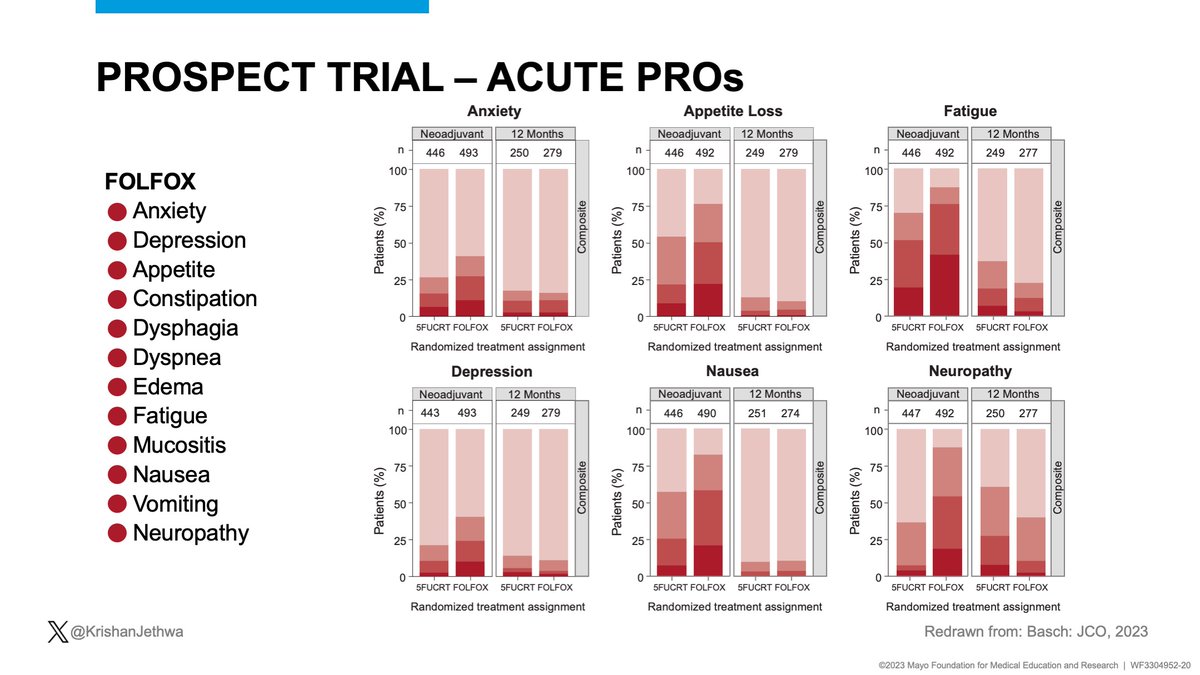
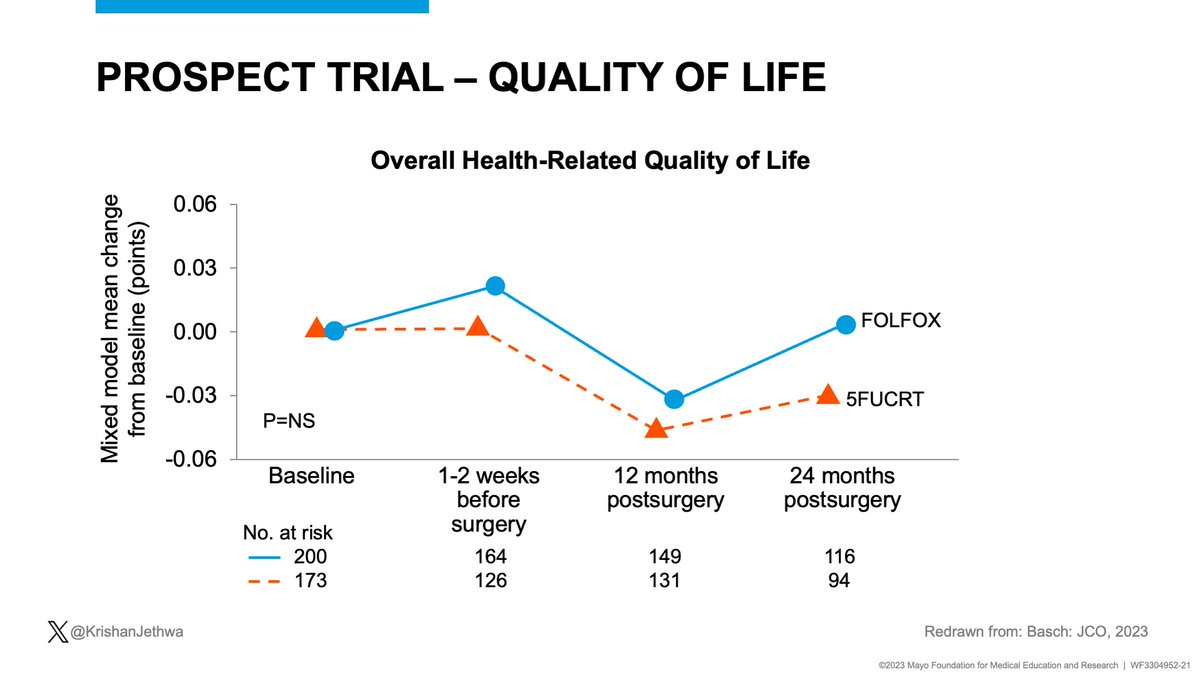
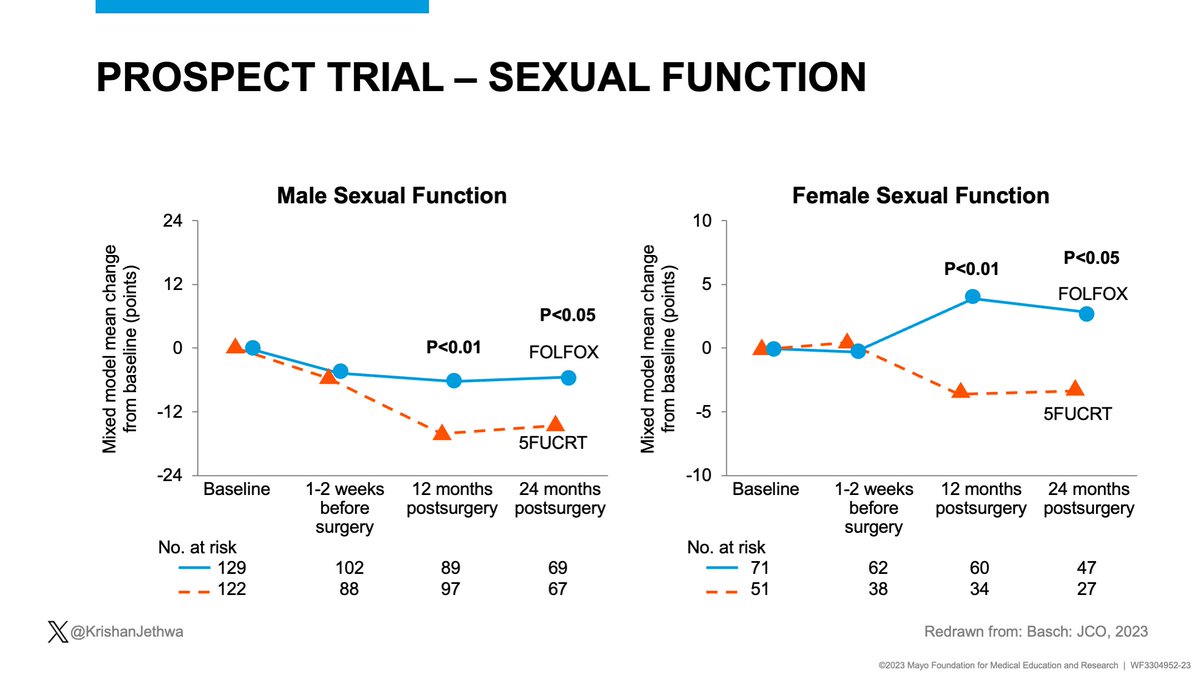
The investigators should commended for collecting PROs!
There were substantial differences in acute PROs but
✅ No difference in overall QoL
✅RT omission did better preserve sexual function




There were substantial differences in acute PROs but
✅ No difference in overall QoL
✅RT omission did better preserve sexual function
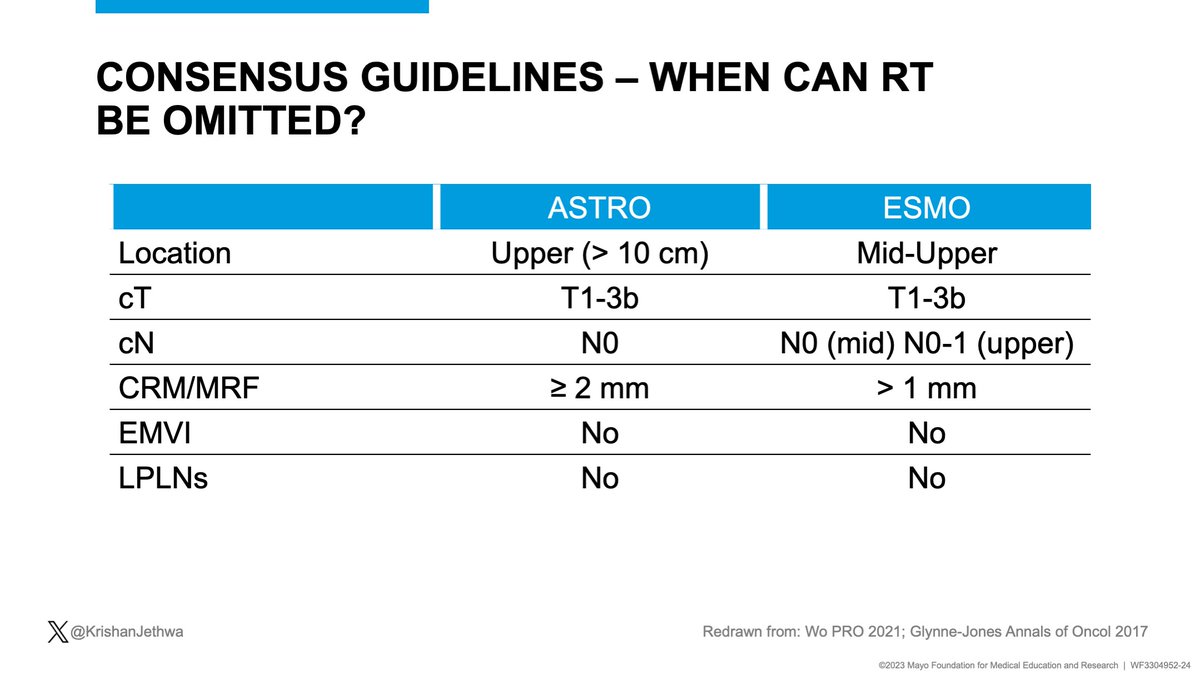
The nuance is 🔑
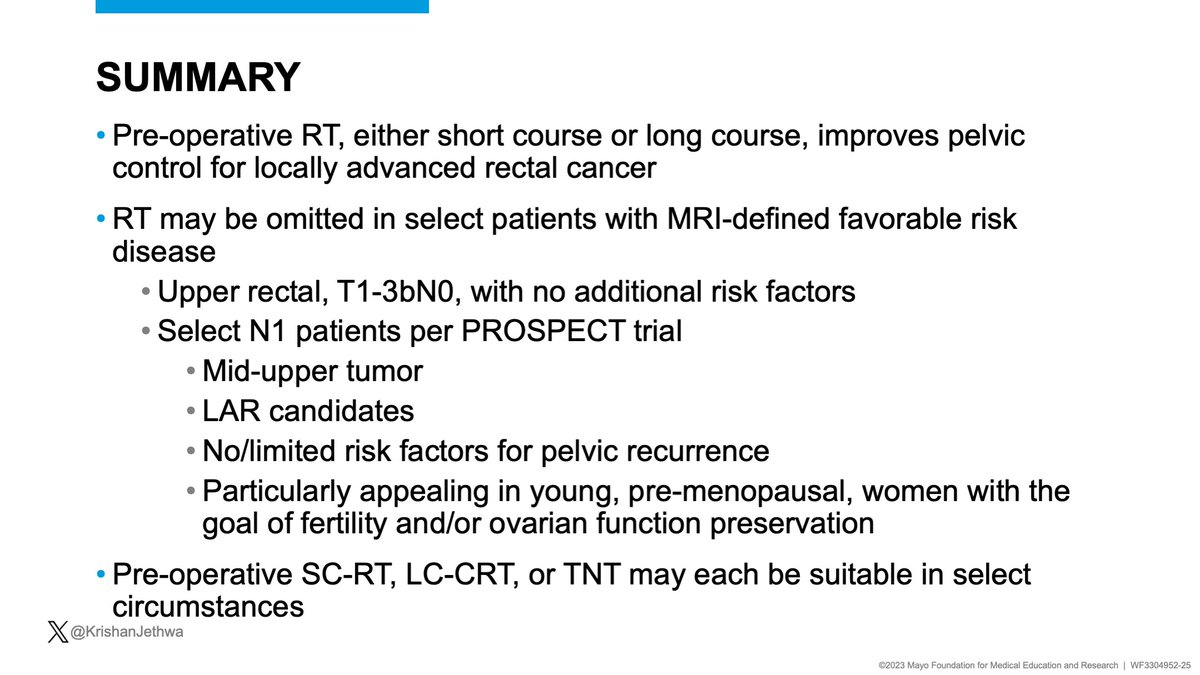
📌RT may be omitted in pts with MRI-defined favorable risk LARC planned for TME 🔪
✅Upper T1-3bN0 with no high risk features
⚠️Select N+ with a mid-upper tumor and no high risk features. Pre-operative chemotherapy may be used, per PROSPECT


📌RT may be omitted in pts with MRI-defined favorable risk LARC planned for TME 🔪
✅Upper T1-3bN0 with no high risk features
⚠️Select N+ with a mid-upper tumor and no high risk features. Pre-operative chemotherapy may be used, per PROSPECT
57M
cT3cN1M0 rectal adenocarcinoma, pMMR, 9 cm from the anal verge
Tumor deposit 2 mm from the mesorectal fascia but otherwise uncompromised.
+ EMVI
No extra-mesorectal lymphadenopathy
Patient is amenable to low anterior resection.
What would you recommend for pre-op management?
cT3cN1M0 rectal adenocarcinoma, pMMR, 9 cm from the anal verge
Tumor deposit 2 mm from the mesorectal fascia but otherwise uncompromised.
+ EMVI
No extra-mesorectal lymphadenopathy
Patient is amenable to low anterior resection.
What would you recommend for pre-op management?
This patient has risk factors for:
‼️ Distant metastasis
⚠️ Pelvic recurrence
Let's review why TNT is most appropriate!
‼️ Distant metastasis
⚠️ Pelvic recurrence
Let's review why TNT is most appropriate!
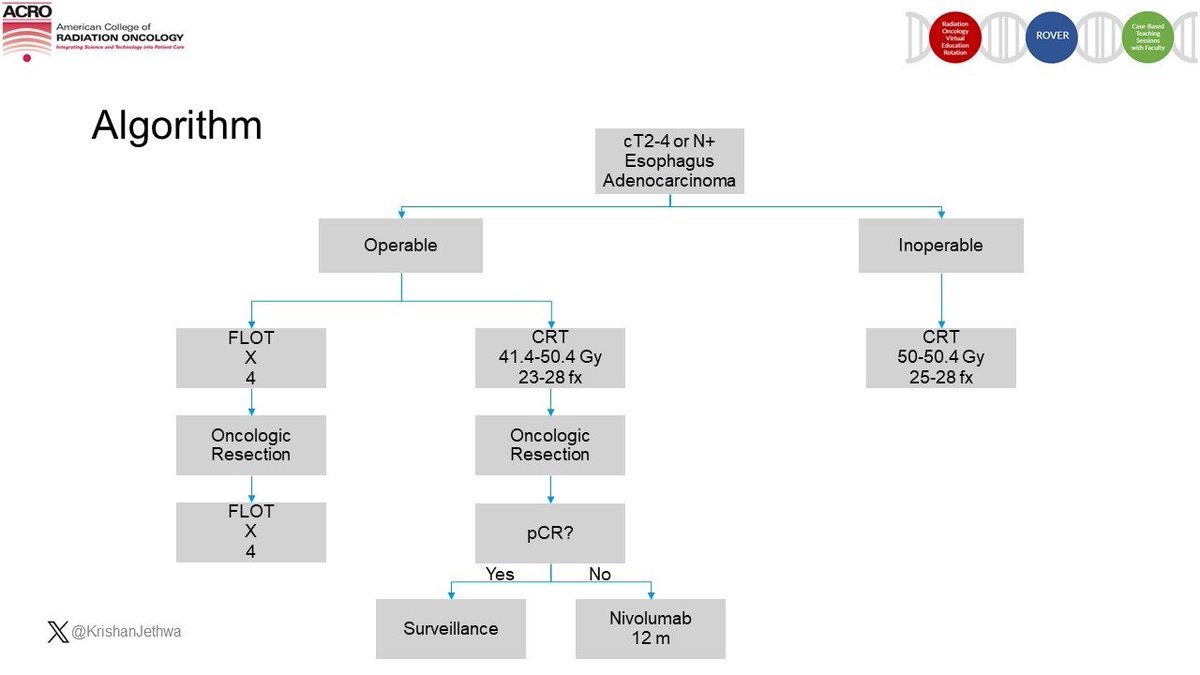
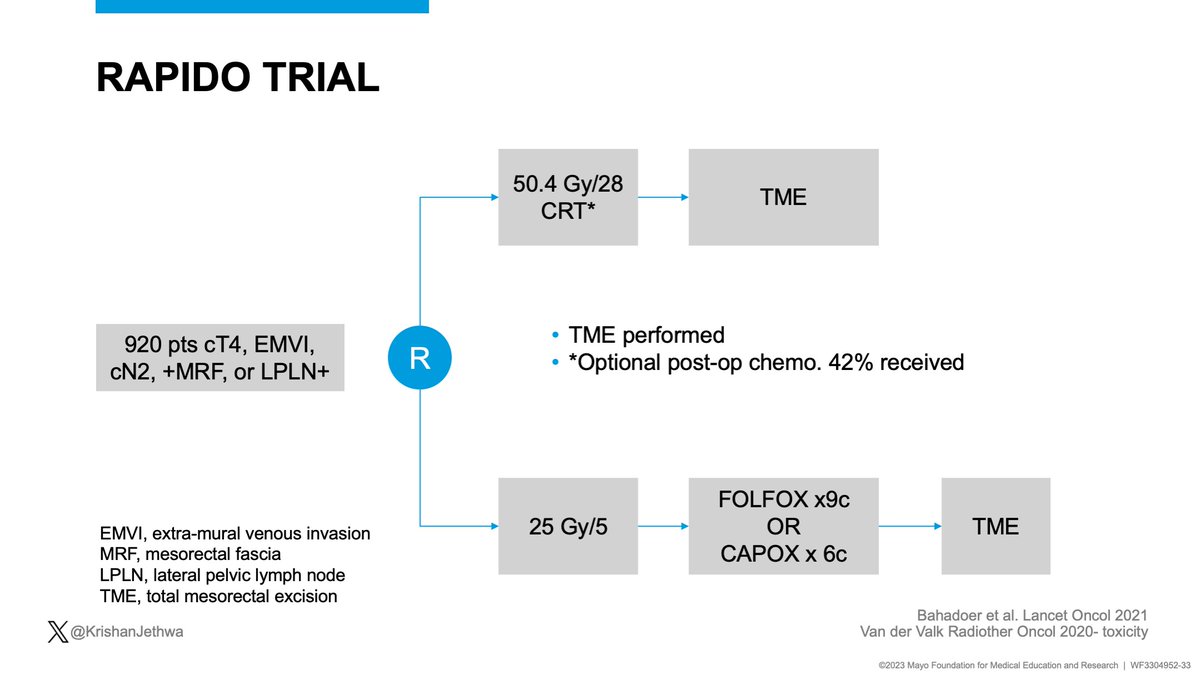
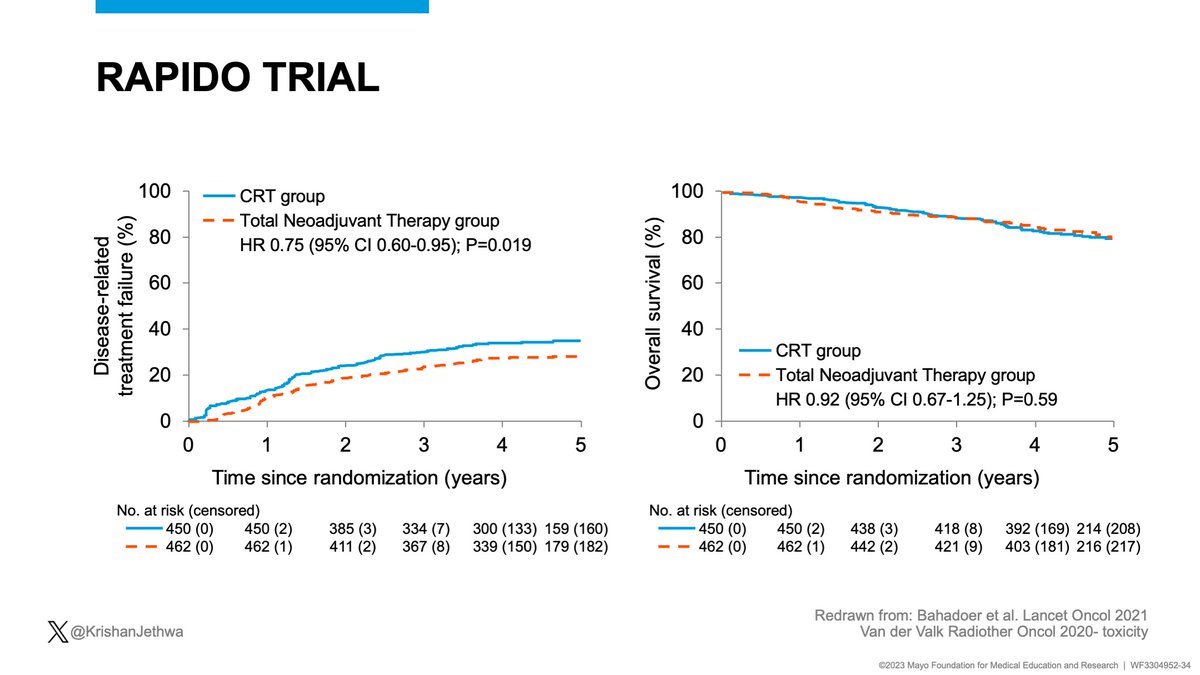
RAPIDO included pts with T4, cN2, +EMVI, +MRF, or +LPNs.
Randomized:
CRT (Adj chemo optional: 42% received)
vs.
Intensified TNT regimen of SC-RT-->FOLFOX.
Key results improved with TNT:
✅⬇️ Disease related treatment failure
✅ Decreased DM


Randomized:
CRT (Adj chemo optional: 42% received)
vs.
Intensified TNT regimen of SC-RT-->FOLFOX.
Key results improved with TNT:
✅⬇️ Disease related treatment failure
✅ Decreased DM
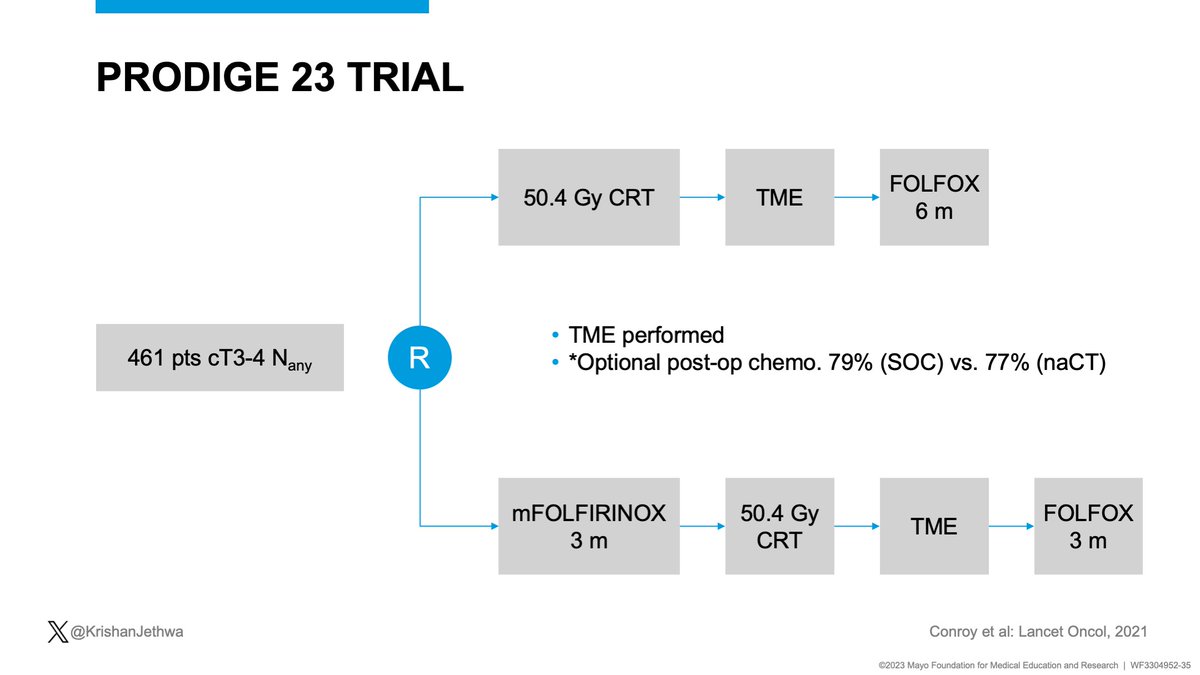
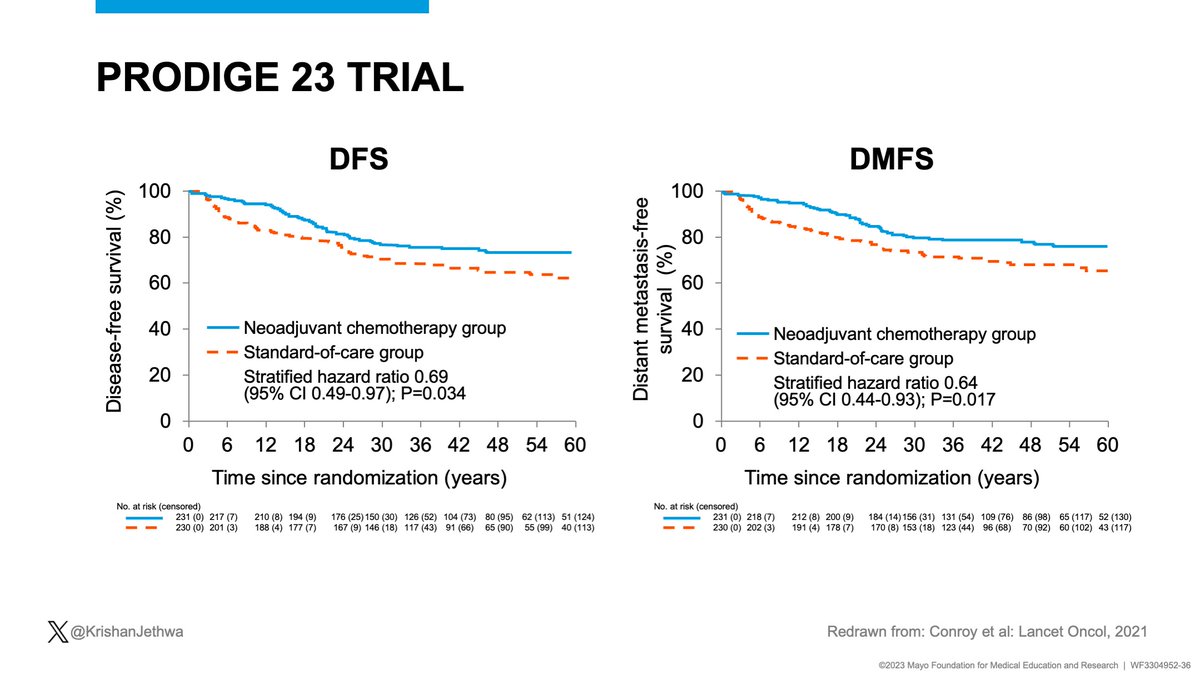
PRODIGE 23 included pts with cT3-4 disease
Randomized:
CRT-->FOLFOX
vs.
mFOLFIRINOX --> CRT-->S -->FOLFOX
Key results improved with TNT!
✅Improved DFS
✅ Decreased DM
✅✅✅ Improved OS!!!



Randomized:
CRT-->FOLFOX
vs.
mFOLFIRINOX --> CRT-->S -->FOLFOX
Key results improved with TNT!
✅Improved DFS
✅ Decreased DM
✅✅✅ Improved OS!!!
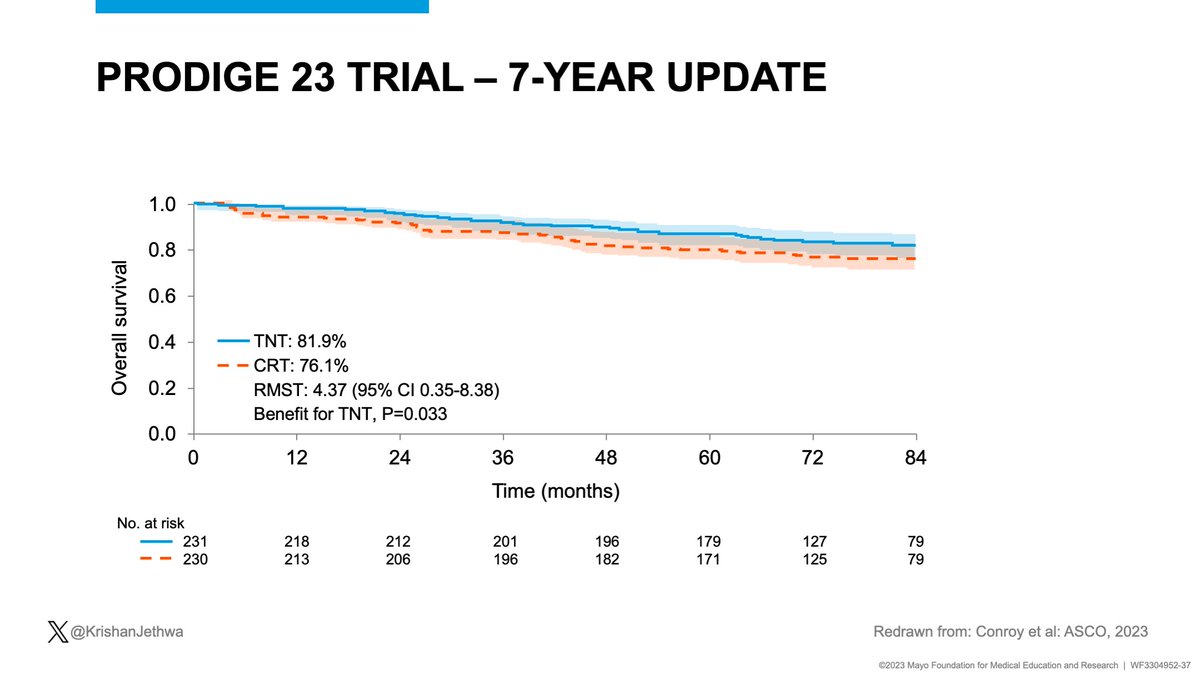
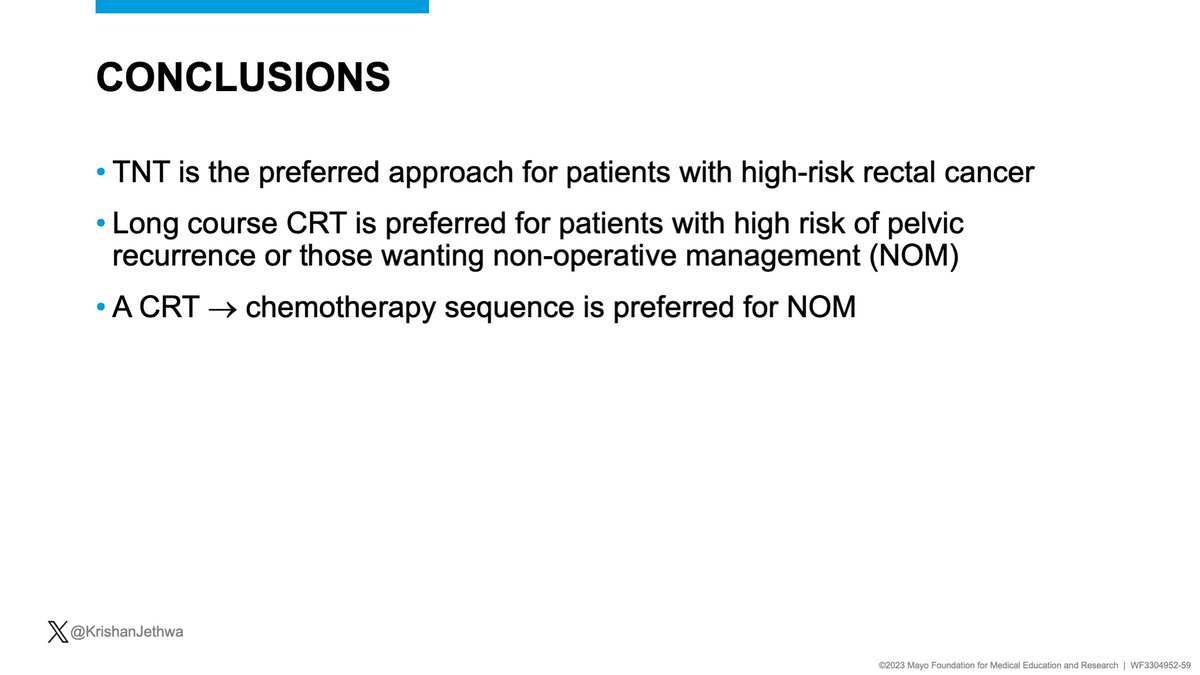
Summary!
TNT is the preferred approach for patients with
high-risk rectal cancer
✅Reduces distant metastasis
✅Improves disease-free survival
✅✅✅May improve overall survival
TNT is the preferred approach for patients with
high-risk rectal cancer
✅Reduces distant metastasis
✅Improves disease-free survival
✅✅✅May improve overall survival
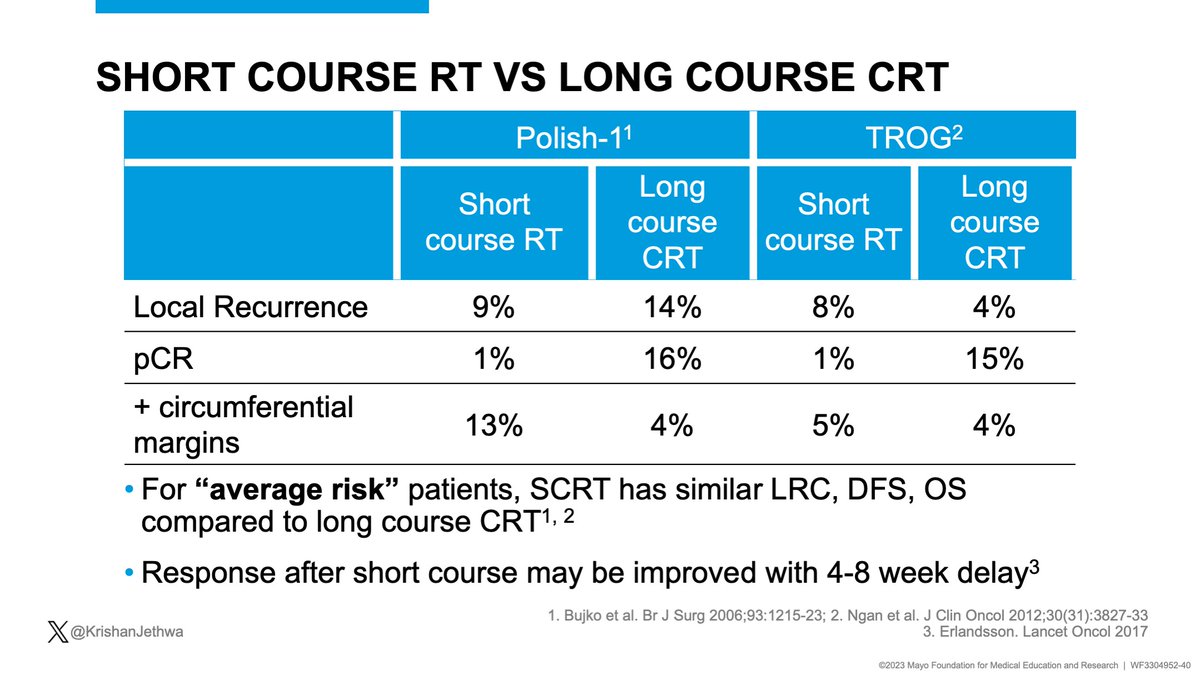
Let’s discuss SC-RT vs. LC-CRT
SCRT= similar LC, DFS, OS in prior studies of “average risk” patients.
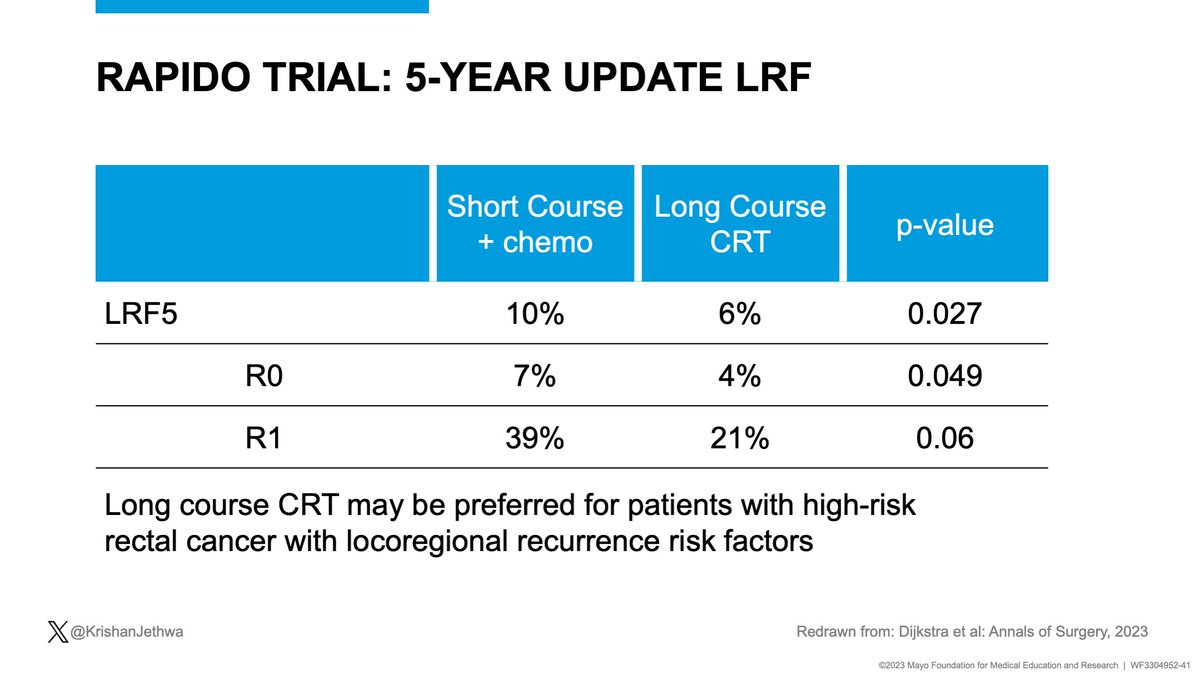
🔥RAPIDO- high risk: ⬆️ pelvic recurrence (10% vs. 6%) with SC-TNT vs. LC-CRT.
LC-CRT may be preferred for patients with high-risk rectal cancer
x.com/IJROBP/status/…



SCRT= similar LC, DFS, OS in prior studies of “average risk” patients.
🔥RAPIDO- high risk: ⬆️ pelvic recurrence (10% vs. 6%) with SC-TNT vs. LC-CRT.
LC-CRT may be preferred for patients with high-risk rectal cancer
x.com/IJROBP/status/…
69F
cT3cN2M0 rectal adenocarcinoma, pMMR
3-4 cm from the anal verge
+ MRF
- extra-mesorectal LNs
- EMVI
Patient will require APR, which she wants to avoid.
What would you recommend for initial management?
cT3cN2M0 rectal adenocarcinoma, pMMR
3-4 cm from the anal verge
+ MRF
- extra-mesorectal LNs
- EMVI
Patient will require APR, which she wants to avoid.
What would you recommend for initial management?
Key points:
This patient has:
‼️ DM risk
⚠️ Pelvic recurrence risk
🚨 Desire for organ preservation
Let's review sequence of therapy and relation to non-operative management
This patient has:
‼️ DM risk
⚠️ Pelvic recurrence risk
🚨 Desire for organ preservation
Let's review sequence of therapy and relation to non-operative management

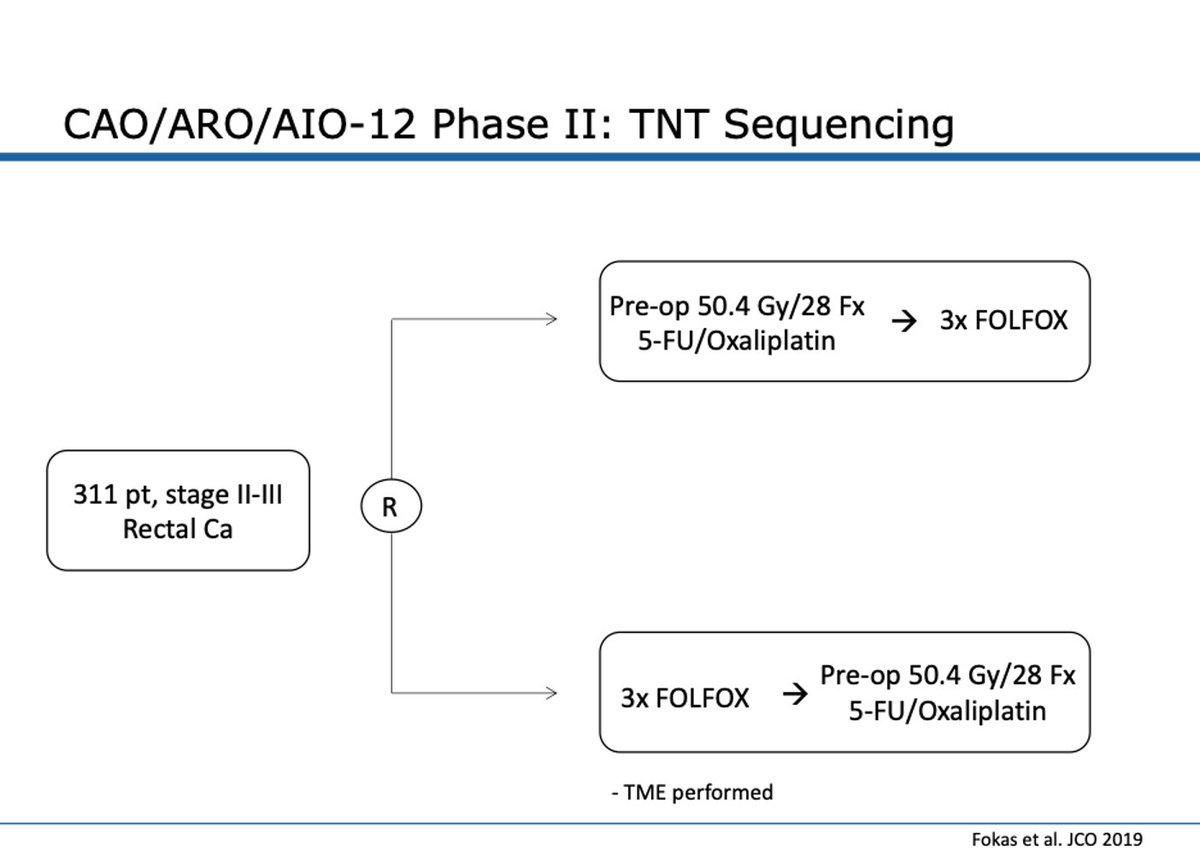
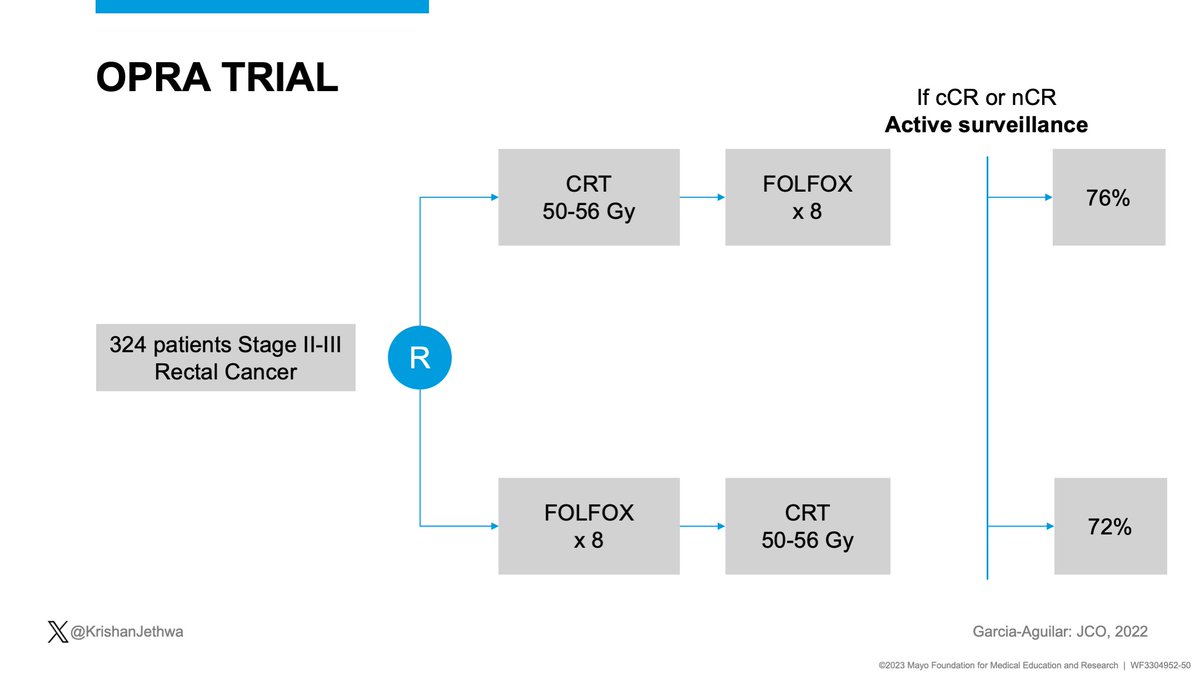
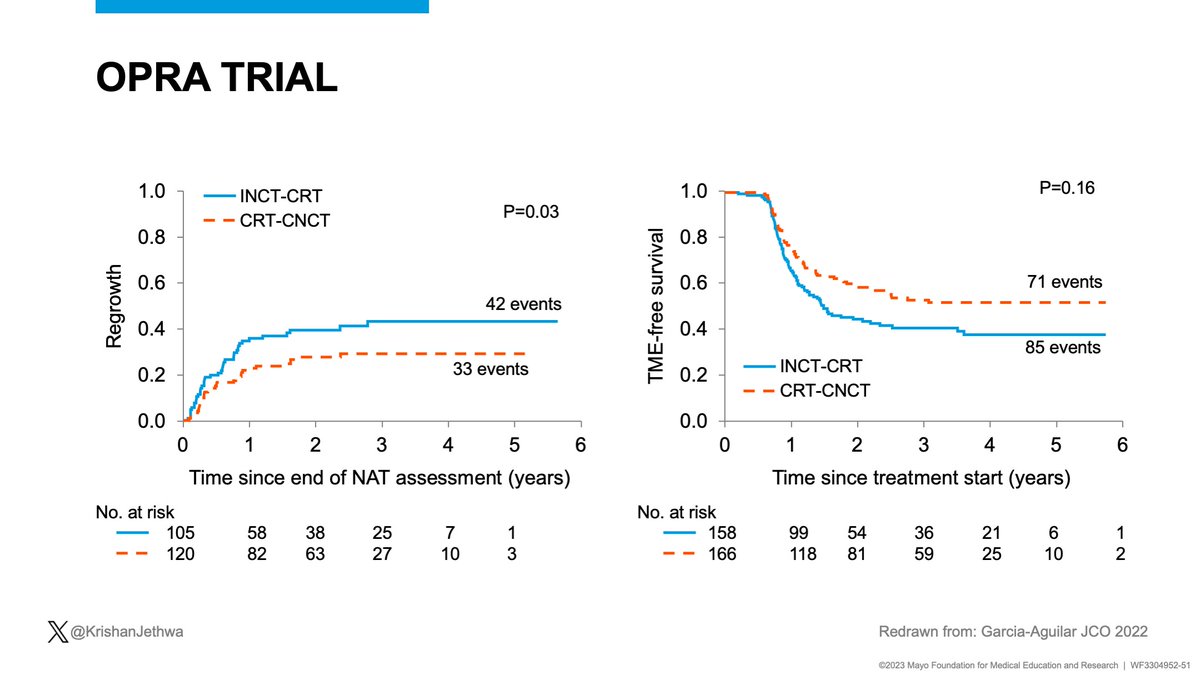
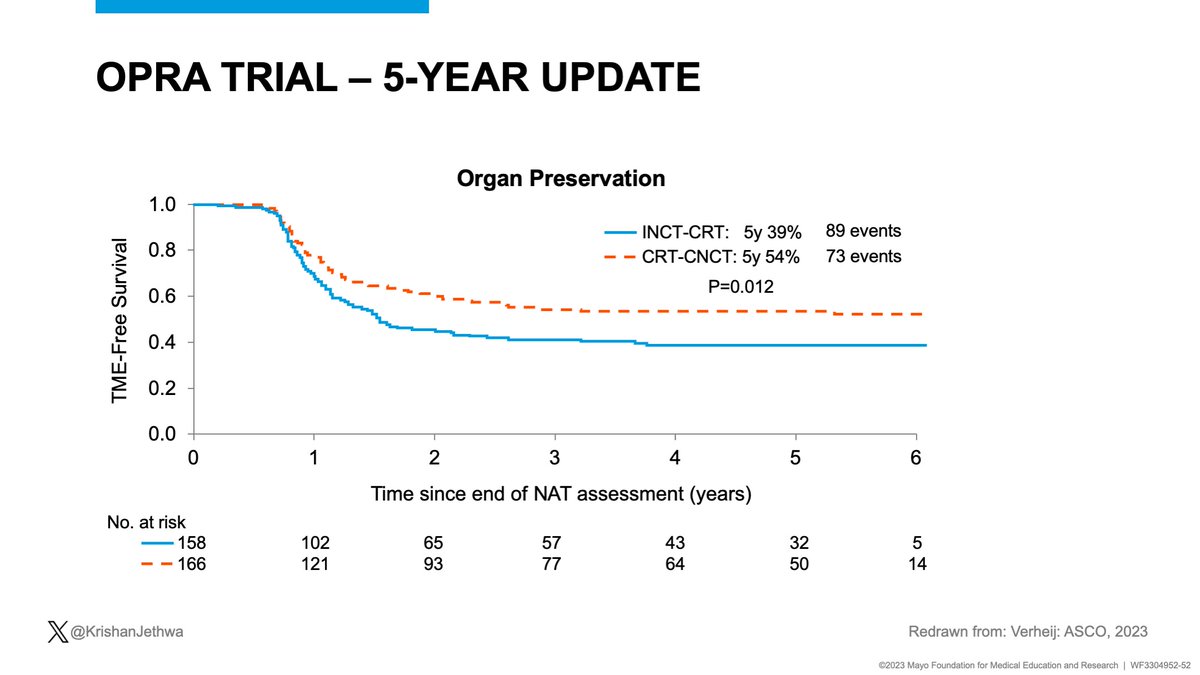
Why RT first?
2 RCTs evaluated TNT sequencing
German CAO/ARO/AIO-12 (pCR endpoint):
✅⬆️ pCR with CRT--> chemo.
OPRA:
CRT--> chemo sequence:
✅⬇️ local regrowth and
✅⬆️ organ preservation with CRT-->chemo
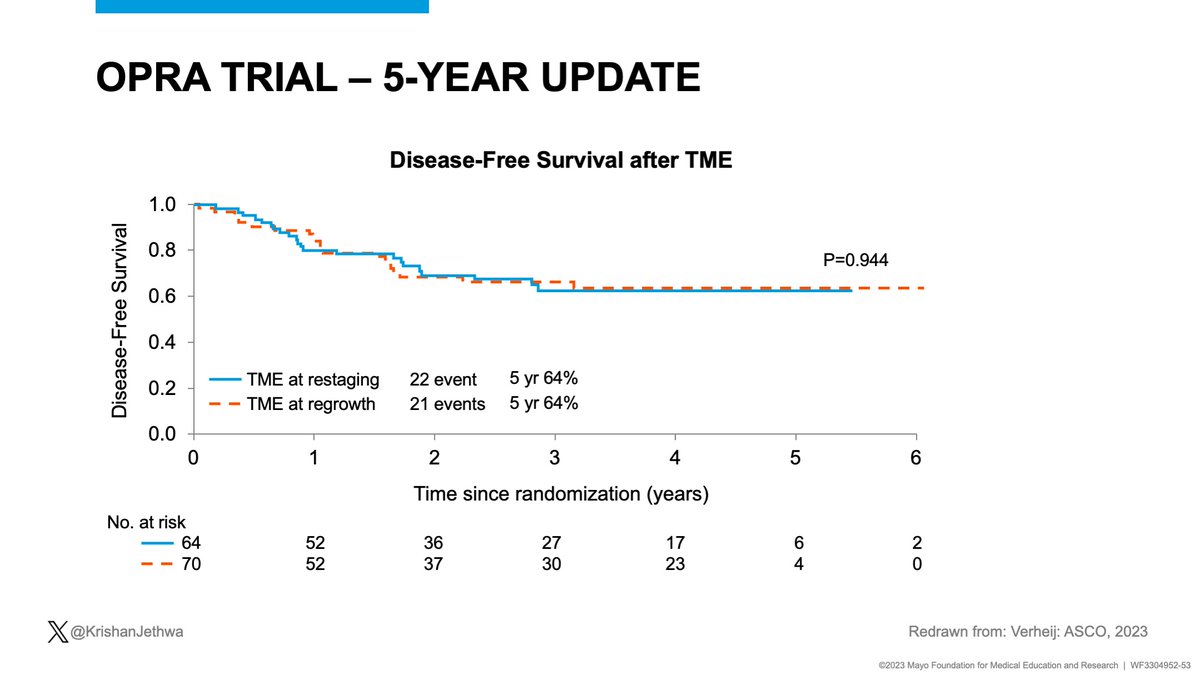
✅No difference in DFS or DFS after TME (initial iCR or regrowth)




2 RCTs evaluated TNT sequencing
German CAO/ARO/AIO-12 (pCR endpoint):
✅⬆️ pCR with CRT--> chemo.
OPRA:
CRT--> chemo sequence:
✅⬇️ local regrowth and
✅⬆️ organ preservation with CRT-->chemo
✅No difference in DFS or DFS after TME (initial iCR or regrowth)
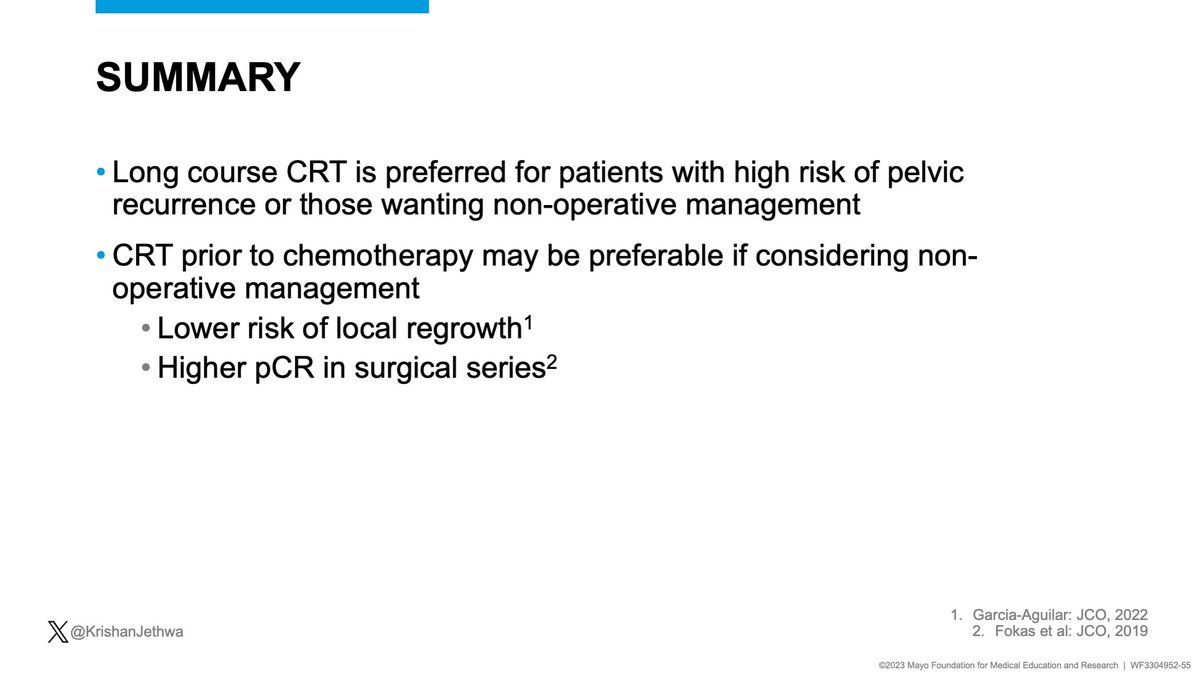
Summary:
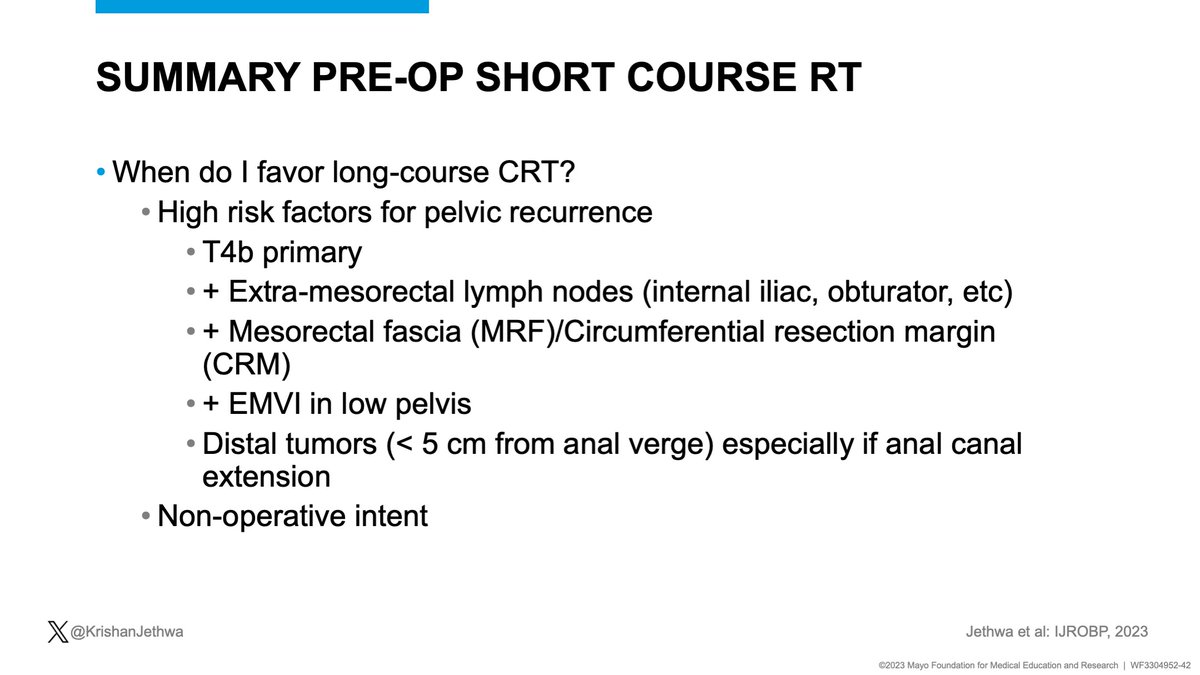
🔥LC-CRT is preferred for patients with high risk of pelvic recurrence or those wanting non-operative management
🔥CRT prior to chemotherapy may be preferable if considering non-operative management
✅Lower risk of local regrowth
✅Higher pCR in surgical series
🔥LC-CRT is preferred for patients with high risk of pelvic recurrence or those wanting non-operative management
🔥CRT prior to chemotherapy may be preferable if considering non-operative management
✅Lower risk of local regrowth
✅Higher pCR in surgical series
Key conclusions:
🔵 Rectal cancer is heterogeneous!
🔵 RT ⬇️ pelvic recurrence but may be omitted in select patients with MRI defined- low risk disease
🔵 TNT is preferred for high risk disease
🔵 CRT --> chemo sequence preferred for NOM
🔥🔥🔥 Multi-D collaboration is CRITICAL!




🔵 Rectal cancer is heterogeneous!
🔵 RT ⬇️ pelvic recurrence but may be omitted in select patients with MRI defined- low risk disease
🔵 TNT is preferred for high risk disease
🔵 CRT --> chemo sequence preferred for NOM
🔥🔥🔥 Multi-D collaboration is CRITICAL!

• • •
Missing some Tweet in this thread? You can try to
force a refresh