LinkedIn saw it first, but I’m proud to announce that, as of yesterday, I’ve finished a PhD (Publication) at @portsmouthuni @UoPSportScience. It was a winding and unorthodox route to develop content expertise and demonstrate the relevant scholarly skills, but worth every second.
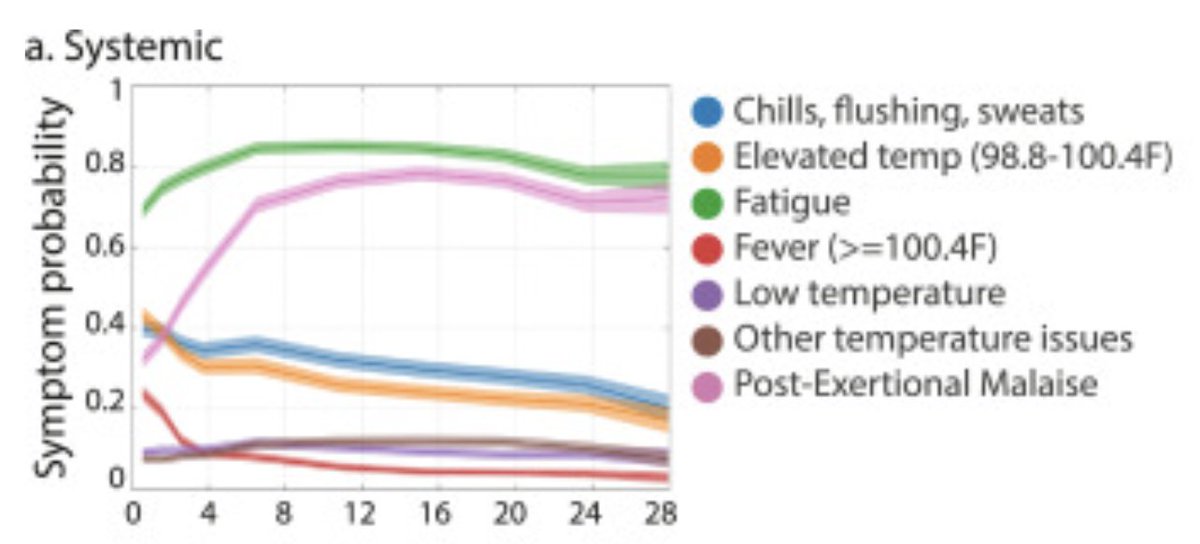
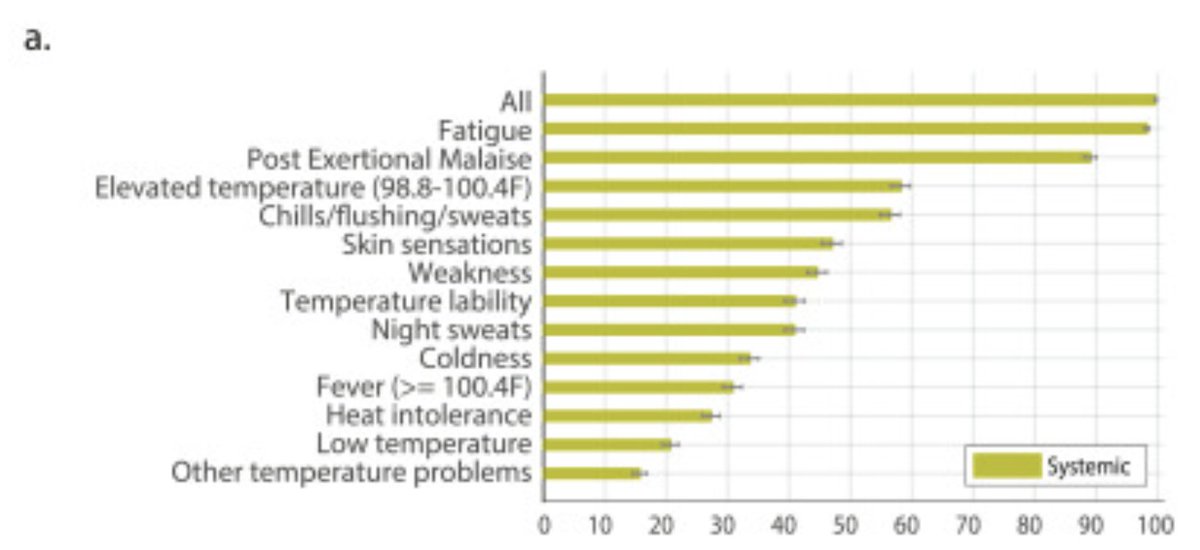
The title of my thesis is “From Function to Physiology and Back in Adults with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome.” It consolidated findings from 11 publications over the last decade of work in this area to tell the story of post-exertional symptoms and signs.
All of the publications in the thesis are out in the public domain, so you may have read them already.
Exercise testing in people with ME/CFS:
👉🏻
👉🏻
👉🏻
…pubmed.ncbi.nlm.nih.gov/23813081/
pubmed.ncbi.nlm.nih.gov/32568145/
pubmed.ncbi.nlm.nih.gov/30968005/
Exercise testing in people with ME/CFS:
👉🏻
👉🏻
👉🏻
…pubmed.ncbi.nlm.nih.gov/23813081/
pubmed.ncbi.nlm.nih.gov/32568145/
pubmed.ncbi.nlm.nih.gov/30968005/
Derivation and validation of outcomes measures:
👉🏻
👉🏻
👉🏻
Clinical and legal applications:
👉🏻
👉🏻
👉🏻 pubmed.ncbi.nlm.nih.gov/32568143/
pubmed.ncbi.nlm.nih.gov/36938769/
pubmed.ncbi.nlm.nih.gov/36938768/
massmecfs.org/images/pdf/Pri…
researchgate.net/publication/26…
researchgate.net/publication/33…
👉🏻
👉🏻
👉🏻
Clinical and legal applications:
👉🏻
👉🏻
👉🏻 pubmed.ncbi.nlm.nih.gov/32568143/
pubmed.ncbi.nlm.nih.gov/36938769/
pubmed.ncbi.nlm.nih.gov/36938768/
massmecfs.org/images/pdf/Pri…
researchgate.net/publication/26…
researchgate.net/publication/33…
Nascent scholarship on clinical interventions:
👉🏻
👉🏻
There’s a (lengthy) foreword discussing the history of psychologization of this phenomenon, tackling challenges of terminology, and covering the need to remediate injustices.pubmed.ncbi.nlm.nih.gov/32623426/
pubmed.ncbi.nlm.nih.gov/36938766/
👉🏻
👉🏻
There’s a (lengthy) foreword discussing the history of psychologization of this phenomenon, tackling challenges of terminology, and covering the need to remediate injustices.pubmed.ncbi.nlm.nih.gov/32623426/
pubmed.ncbi.nlm.nih.gov/36938766/
And, there’s a discussion of what comes next for this line of research. Many of those recommendations already have been put in motion by my @4workwell and @4workwellhealth, as @dsethlewis put it so well the other day, in the spirit of going slow and fixing things.
@4Workwell @4WorkwellHealth @dsethlewis Obviously none of this is worthwhile without people living with ME, and now Long Covid, and their carers and none of this is possible without my @4Workwell @4WorkwellHealth colleagues, other collaborators and friends, and mentors along the way. All of this takes a village.
@4Workwell @4WorkwellHealth Onward.
• • •
Missing some Tweet in this thread? You can try to
force a refresh