views
1/4
IGNORE THE MCH!
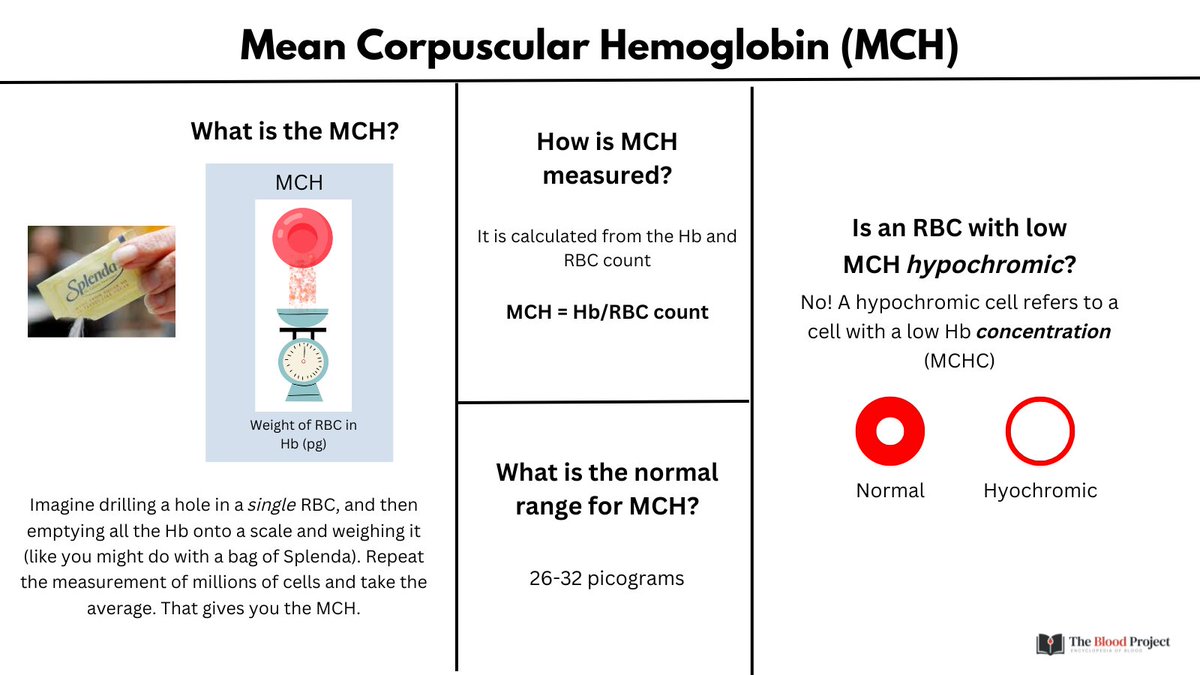
I don't know about you, but our institution provides the mean corpuscular hemoglobin (MCH) with the CBC.
Not only is it a virtually useless (and redundant) parameter, but it often gets confused with the much more meaningful MCHC.
IGNORE THE MCH!
I don't know about you, but our institution provides the mean corpuscular hemoglobin (MCH) with the CBC.
Not only is it a virtually useless (and redundant) parameter, but it often gets confused with the much more meaningful MCHC.
2/4
The MCH is the ave weight of the RBC in Hb (reported in pg). In contrast to the MCHC, it has no place in diagnostic algorithms for anemia.
MCH tracks with the MCV and MCHC (MCH = MCV x MCHC; MCV has the largest effect because % deviation is far greater than with the MCHC).
The MCH is the ave weight of the RBC in Hb (reported in pg). In contrast to the MCHC, it has no place in diagnostic algorithms for anemia.
MCH tracks with the MCV and MCHC (MCH = MCV x MCHC; MCV has the largest effect because % deviation is far greater than with the MCHC).

3/4
MCH has been said to be a surrogate marker for MCV. But if we have the MCV in hand, why do we need a surrogate marker?
There are really only two situations in which the MCH yields additional information to the MCV and MCHC:
MCH has been said to be a surrogate marker for MCV. But if we have the MCV in hand, why do we need a surrogate marker?
There are really only two situations in which the MCH yields additional information to the MCV and MCHC:

4/4
1. Additive effect low-normal MCV and low-normal MCHC may yield a LOW MCH. So what?
2. The MCH is admittedly a useful surrogate for MCV in situations where the MCV is artifactually altered, for example with prolonged storage of blood.
Bottom line: IGNORE THE MCH!!
1. Additive effect low-normal MCV and low-normal MCHC may yield a LOW MCH. So what?
2. The MCH is admittedly a useful surrogate for MCV in situations where the MCV is artifactually altered, for example with prolonged storage of blood.
Bottom line: IGNORE THE MCH!!
• • •
Missing some Tweet in this thread? You can try to
force a refresh