🔥SVT Quest🔥
For EP beginners, remembering the diagnostic criteria for SVTs like AT, ORT via an AP, and AVNRT can be quite tricky😱
There’s a ton of jargon—terms like V-A-V, V-A-A-V, V-V-A responses, orthodromic His capture, total pacing prematurity, A2-H*-V*, and more—plus countless specific values essential for accurate diagnoses💦
Over the years, electrophysiologists have developed various diagnostic maneuvers, yet even the best methods reveal flaws years after their debut. Consequently, others innovate new techniques, propelling continuous evolution and enhancement in the field🔥
EP University explores the global history of SVT diagnostic criteria, detailing their introduction, significance, and concepts in chronological order.
✅Step 1
differentiating AT from ORT and AVNRT
✅Step 2
differentiating ORT from AVNRT
✅Step 3
diagnosis of concealed nodovantricular/nodofascicular or his-ventricular pathway-related tachycardia.
#EPUniversity
For EP beginners, remembering the diagnostic criteria for SVTs like AT, ORT via an AP, and AVNRT can be quite tricky😱
There’s a ton of jargon—terms like V-A-V, V-A-A-V, V-V-A responses, orthodromic His capture, total pacing prematurity, A2-H*-V*, and more—plus countless specific values essential for accurate diagnoses💦
Over the years, electrophysiologists have developed various diagnostic maneuvers, yet even the best methods reveal flaws years after their debut. Consequently, others innovate new techniques, propelling continuous evolution and enhancement in the field🔥
EP University explores the global history of SVT diagnostic criteria, detailing their introduction, significance, and concepts in chronological order.
✅Step 1
differentiating AT from ORT and AVNRT
✅Step 2
differentiating ORT from AVNRT
✅Step 3
diagnosis of concealed nodovantricular/nodofascicular or his-ventricular pathway-related tachycardia.
#EPUniversity

✅Step 1
Differentiating AT from ORT and AVNRT
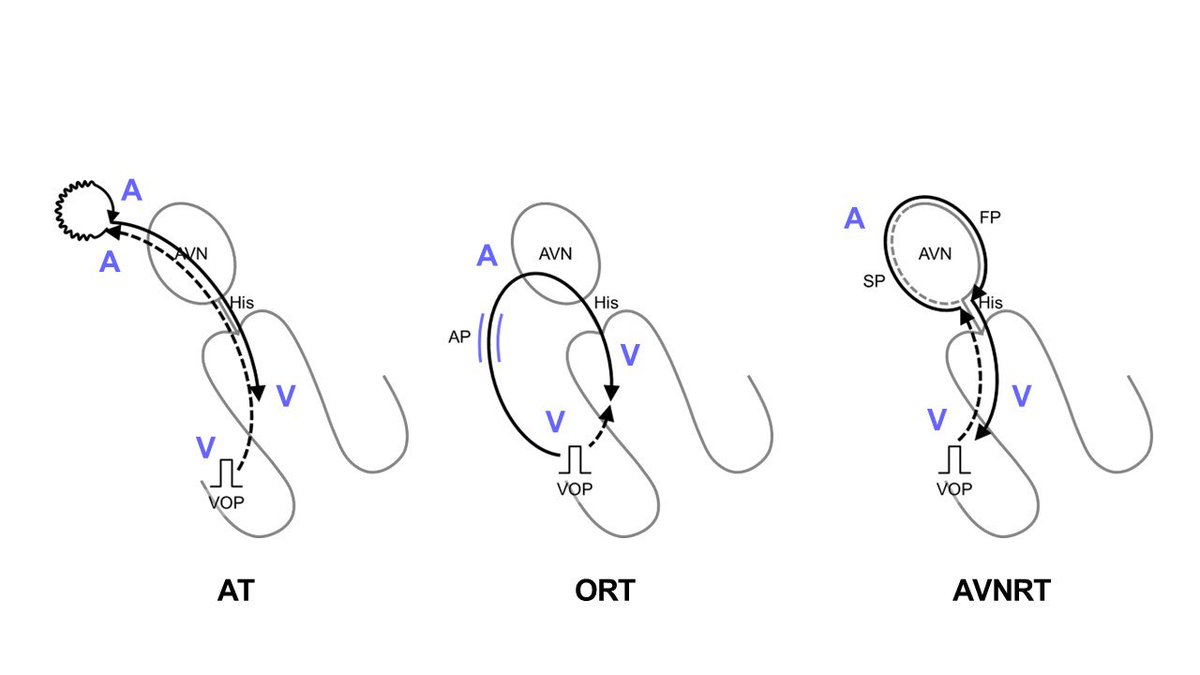
AT usually shows up as long RP tach, which needs careful differentiation from ORT via an AP with decremental properties or from fast-slow AVNRT, both of which also display long RP tach due to longer retrograde conduction times over decremental AP/slow pathway (SP) and relatively shorter anterograde conduction times over fast pathway.
Differentiating AT from ORT and AVNRT
AT usually shows up as long RP tach, which needs careful differentiation from ORT via an AP with decremental properties or from fast-slow AVNRT, both of which also display long RP tach due to longer retrograde conduction times over decremental AP/slow pathway (SP) and relatively shorter anterograde conduction times over fast pathway.
Brad Knight found that AT typically resumed with a V-A-A-V response after cessation of right ventricular overdrive pacing (VOP), whereas other SVTs like ORT and AVNRT usually resumed with a V-A-V response. There's a tricky thing to watch out for called a pseudo-V-A-A-V response. In ORTs via the decremental AP and atypical AVNRTs, pacing-induced decremental conduction through the retrograde AP or SP can cause the paced VA interval exceeding the pacing cycle length (PCL), creating a pseudo-V-A-A-V response. You can spot this fake-out when the second atrial beat (A2) after VOP speeds up at a PCL. To really nail the diagnosis of a V-A-A-V or V-A-V response, electrophysiologists need to figure out which atrial electrogram the last pacing captured by measuring the atrial interval.
#EPUniversity
sciencedirect.com/science/articl…
#EPUniversity
sciencedirect.com/science/articl…
🚨But a V-A-A-V response can happen from a double atrial response (DAR) using both FP and SP in fast-slow AVNRTs.🚨
This insight tells that while a V-A-V response rules out AT, a V-A-A-V response needs more digging.
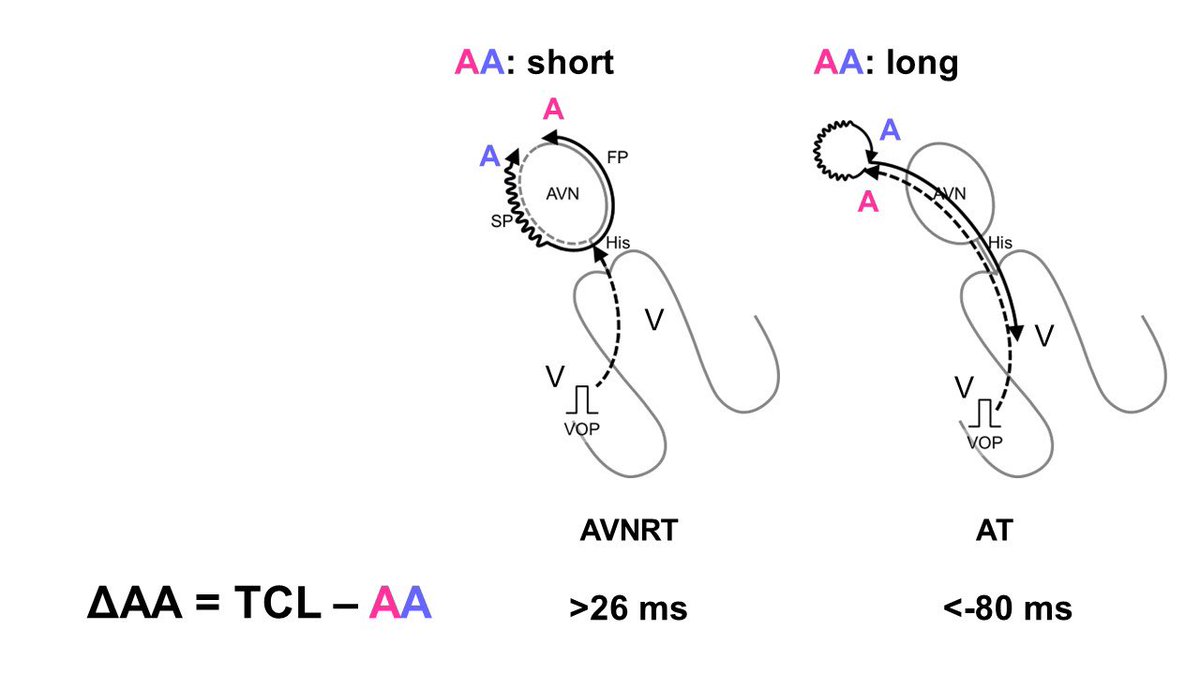
To tackle this, Kaneko @KanekoYosh et al. (including me) introduced the ΔAA interval to tell apart V-A-A-V responses in AT and AVNRT linked to a DAR💡
The ΔAA interval is figured by subtracting the AA interval during tachycardia (=TCL) from the AA interval between the 1st and 2nd atrial electrograms during the V-A-A-V response.
The AA interval during V-A-A-V is typically shorter in AVNRT as it shows the gap between retrograde FP and SP conduction. In contrast, it's longer in AT, reflecting the whole reentrant circuit's conduction time.
ΔAA >26 ms is diagnostic for fast-slow AVNRT, while a ΔAA < −80 ms is diagnostic for AT.
However, a ΔAA from −80 to 26 ms leaves the diagnosis up in the air.
#EPUniversity
#SVTquestonlinelibrary.wiley.com/doi/10.1111/pa…
This insight tells that while a V-A-V response rules out AT, a V-A-A-V response needs more digging.
To tackle this, Kaneko @KanekoYosh et al. (including me) introduced the ΔAA interval to tell apart V-A-A-V responses in AT and AVNRT linked to a DAR💡
The ΔAA interval is figured by subtracting the AA interval during tachycardia (=TCL) from the AA interval between the 1st and 2nd atrial electrograms during the V-A-A-V response.
The AA interval during V-A-A-V is typically shorter in AVNRT as it shows the gap between retrograde FP and SP conduction. In contrast, it's longer in AT, reflecting the whole reentrant circuit's conduction time.
ΔAA >26 ms is diagnostic for fast-slow AVNRT, while a ΔAA < −80 ms is diagnostic for AT.
However, a ΔAA from −80 to 26 ms leaves the diagnosis up in the air.
#EPUniversity
#SVTquestonlinelibrary.wiley.com/doi/10.1111/pa…
✅Differential Atrial Overdrive Pacing
🚨Differentiation of AT from ORT and AVNRT using VOP is limited without consistent 1:1 VA conduction.🚨
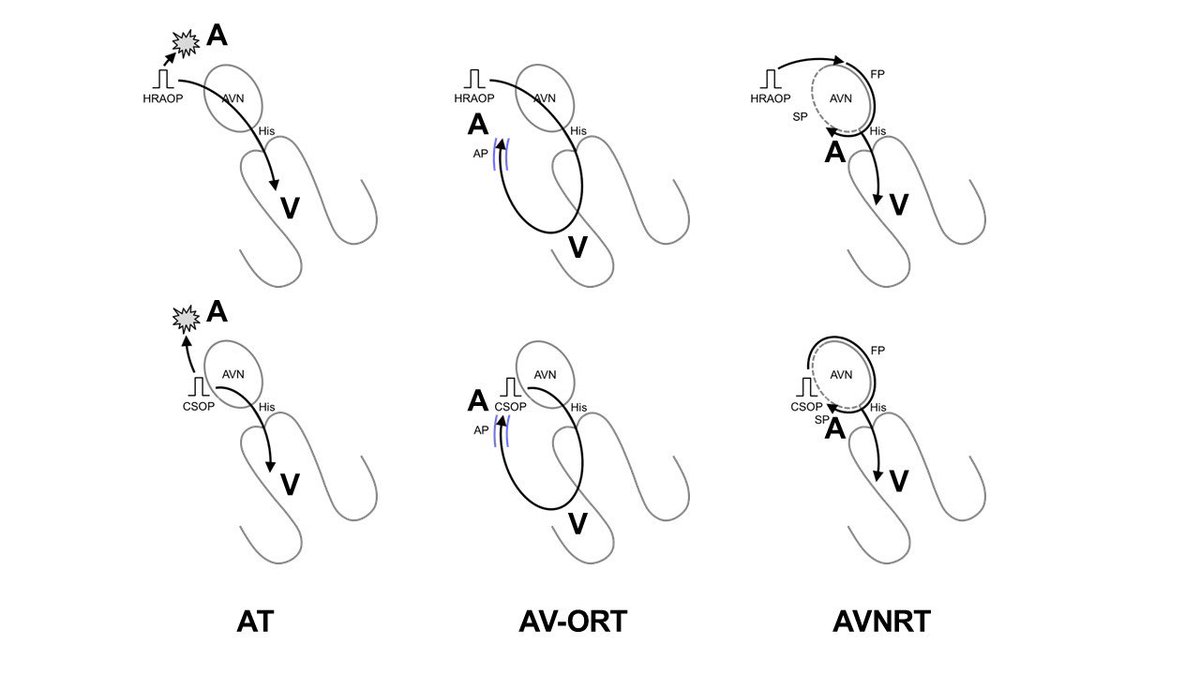
To address this issue, Dr Maruyama looked into VA linking using differential atrial overdrive pacing (DAOP).
During tachycardia, DAOP is applied at 3 locations—the HRA, pCS and dCS. The maximal difference in post-pacing VA intervals (from the last captured RV-EGM to the following atrial EGM) across these pacing sites is measured as the ΔVA interval.
ΔVA interval is fixed at ≤14 (later modified as 20) ms in ORT and AVNRT because the post-pacing VA interval reflects the conduction time of the retrograde limb of the tachycardia (AP or SP) regardless of the atrial pacing site.
ΔVA interval >14 (later modified as 20) ms (a lack of VA linking) is diagnostic for AT, as the post-pacing VA intervals are dependent on the time differences between the last pacing that captures the ventricle and the last pacing that captures the AT origin. These intervals vary according to the proximity of the pacing site to the AVN and AT origin.
#EPUniversity
#SVTquestsciencedirect.com/science/articl…
🚨Differentiation of AT from ORT and AVNRT using VOP is limited without consistent 1:1 VA conduction.🚨
To address this issue, Dr Maruyama looked into VA linking using differential atrial overdrive pacing (DAOP).
During tachycardia, DAOP is applied at 3 locations—the HRA, pCS and dCS. The maximal difference in post-pacing VA intervals (from the last captured RV-EGM to the following atrial EGM) across these pacing sites is measured as the ΔVA interval.
ΔVA interval is fixed at ≤14 (later modified as 20) ms in ORT and AVNRT because the post-pacing VA interval reflects the conduction time of the retrograde limb of the tachycardia (AP or SP) regardless of the atrial pacing site.
ΔVA interval >14 (later modified as 20) ms (a lack of VA linking) is diagnostic for AT, as the post-pacing VA intervals are dependent on the time differences between the last pacing that captures the ventricle and the last pacing that captures the AT origin. These intervals vary according to the proximity of the pacing site to the AVN and AT origin.
#EPUniversity
#SVTquestsciencedirect.com/science/articl…
✅The Last Entrainment Sequence
🚨However, later research showed that fast-slow AVNRTs might lack VA linking.
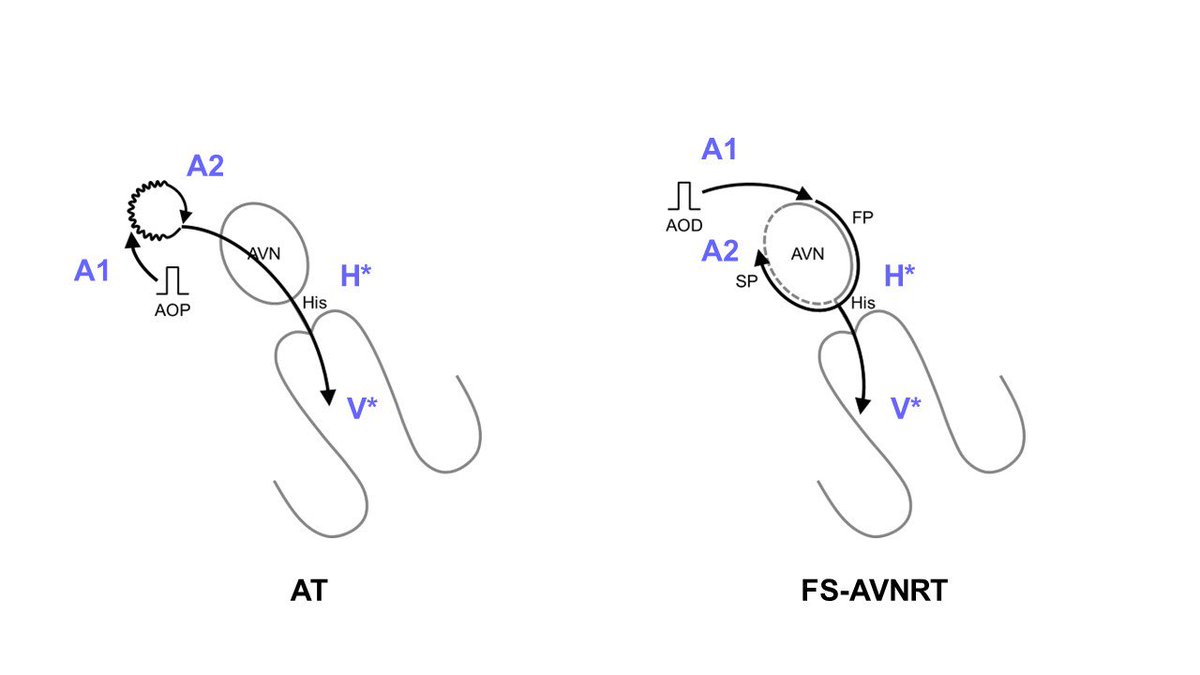
💡Based on this situation, Dr. Maruyama introduced the last entrainment sequence after AOP for more accurate
diagnosis of reentrant AT.
📝The initial step is to verify the orthodromic capture of the earliest atrial activation site (EAAS) by measuring A1-A2 after AOP cessation and repeating the AOP from another atrial site. Orthodromic capture is confirmed if A2 accelerates to PCL.
📝After confirming orthodromic capture, the sequence of A2, and the last His (H*) and RV (V*) EGMs accelerated to the PCL, is analyzed. The A2-H*-V* sequence is diagnostic of AT. Conversely, H*-V*-A2 and H*-A2-V* sequences suggest ORT or AVNRT.
🚨Note that pseudo-H*-V*-A2 response may occur in tricuspid annular ATs, particularly when the AOP site is closer to the AV node than to the AT circuit.
💡The advantage of this maneuver is not only in its accuracy for AT diagnosis but also in its helpfulness in determining the ablation strategy, especially for perinodal AT. The orthodromic capture of EAAS means the pacing site is proximal to the slow conduction zone of the reentrant AT circuit, that is essential information for a safer ablation strategy known as Yamabe's method.
#EPUniversity
#SVTquestjacc.org/doi/10.1016/j.…
🚨However, later research showed that fast-slow AVNRTs might lack VA linking.
💡Based on this situation, Dr. Maruyama introduced the last entrainment sequence after AOP for more accurate
diagnosis of reentrant AT.
📝The initial step is to verify the orthodromic capture of the earliest atrial activation site (EAAS) by measuring A1-A2 after AOP cessation and repeating the AOP from another atrial site. Orthodromic capture is confirmed if A2 accelerates to PCL.
📝After confirming orthodromic capture, the sequence of A2, and the last His (H*) and RV (V*) EGMs accelerated to the PCL, is analyzed. The A2-H*-V* sequence is diagnostic of AT. Conversely, H*-V*-A2 and H*-A2-V* sequences suggest ORT or AVNRT.
🚨Note that pseudo-H*-V*-A2 response may occur in tricuspid annular ATs, particularly when the AOP site is closer to the AV node than to the AT circuit.
💡The advantage of this maneuver is not only in its accuracy for AT diagnosis but also in its helpfulness in determining the ablation strategy, especially for perinodal AT. The orthodromic capture of EAAS means the pacing site is proximal to the slow conduction zone of the reentrant AT circuit, that is essential information for a safer ablation strategy known as Yamabe's method.
#EPUniversity
#SVTquestjacc.org/doi/10.1016/j.…
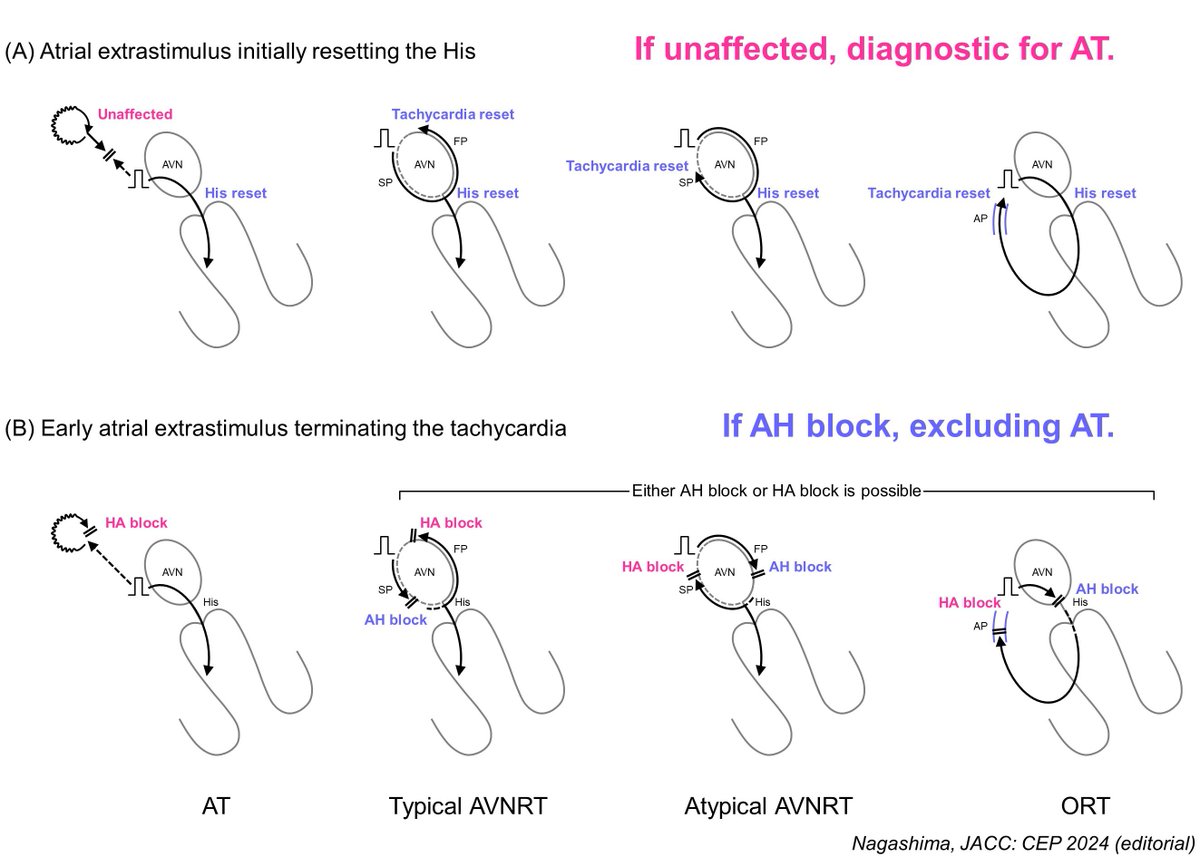
✅Scanned PAC Initially Resetting the His
🚨The utility of these overdrive pacing-based maneuvers is limited if the tachycardia stops or if sustained 1:1 AV conduction cannot be achieved during AOP, making the assessment unclear.
💡To tackle this issue, Inaba developed new diagnostic criteria using a single scanned PAC. The PAC is applied in the pCS, gradually decreasing the coupling interval until it first resets the His bundle, and continues until it stops the tachycardia. Tachycardia reset is confirmed by measuring the atrial interval over 2 cycles around the PAC.
💡If there's no tachycardia reset immediately following PAC that initially resets the His confirms AT with 96% sensitivity and 100% specificity.
💡Additionally, tachycardia termination with AH block by early PAC excludes AT with 92% sensitivity and 100% specificity.
📝This approach has a lower risk of stopping the tachycardia and is useful for SVTs with 2:1 AV conduction. However, its usefulness is limited when assessing tachycardias with wobbling TCL.
💕Actually, I have written the editorial in JACC CEP with this figure (in press)😃
#EPUniversity
#SVTquestsciencedirect.com/science/articl…
🚨The utility of these overdrive pacing-based maneuvers is limited if the tachycardia stops or if sustained 1:1 AV conduction cannot be achieved during AOP, making the assessment unclear.
💡To tackle this issue, Inaba developed new diagnostic criteria using a single scanned PAC. The PAC is applied in the pCS, gradually decreasing the coupling interval until it first resets the His bundle, and continues until it stops the tachycardia. Tachycardia reset is confirmed by measuring the atrial interval over 2 cycles around the PAC.
💡If there's no tachycardia reset immediately following PAC that initially resets the His confirms AT with 96% sensitivity and 100% specificity.
💡Additionally, tachycardia termination with AH block by early PAC excludes AT with 92% sensitivity and 100% specificity.
📝This approach has a lower risk of stopping the tachycardia and is useful for SVTs with 2:1 AV conduction. However, its usefulness is limited when assessing tachycardias with wobbling TCL.
💕Actually, I have written the editorial in JACC CEP with this figure (in press)😃
#EPUniversity
#SVTquestsciencedirect.com/science/articl…
In the summary of step 1, it's recommended to start with VOP. A V-A-V response rules out AT. However, because a V-A-A-V response might be caused by a double atrial response in AVNRT, it's necessary to further assess the ΔAA interval in the same tracing. Unless consistent 1:1 retrograde VA conduction is achieved, differential AOP should be used to check VA linking and the last entrainment sequence. Additionally, if the tachycardia stops during VOD or AOD, it's advisable to use an atrial extrastimulus.
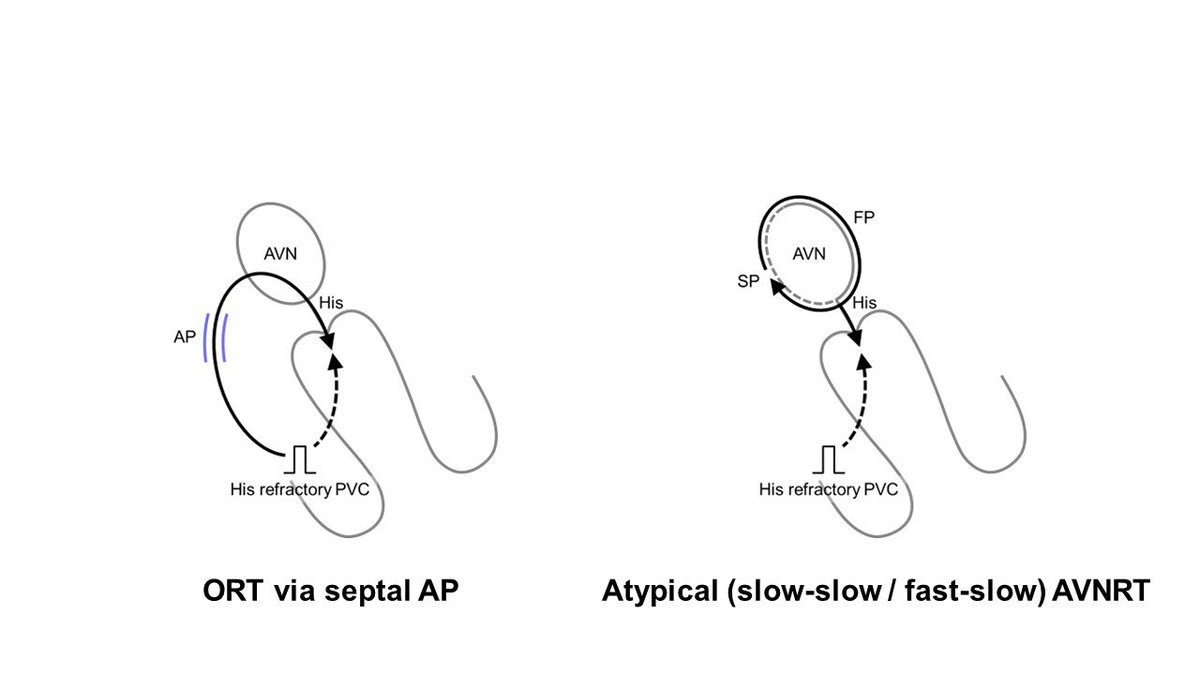
✅Step 2. Differentiating ORT from AVNRT
After ruling out AT, the next step is to differentiate between ORT and AVNRT.
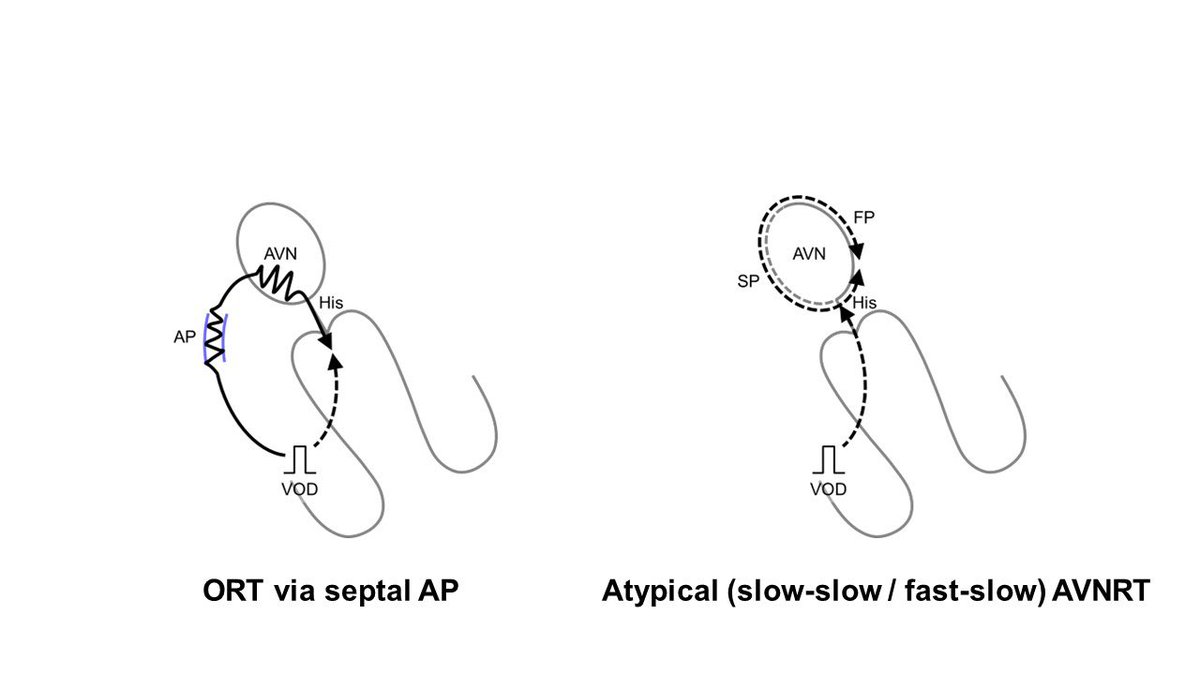
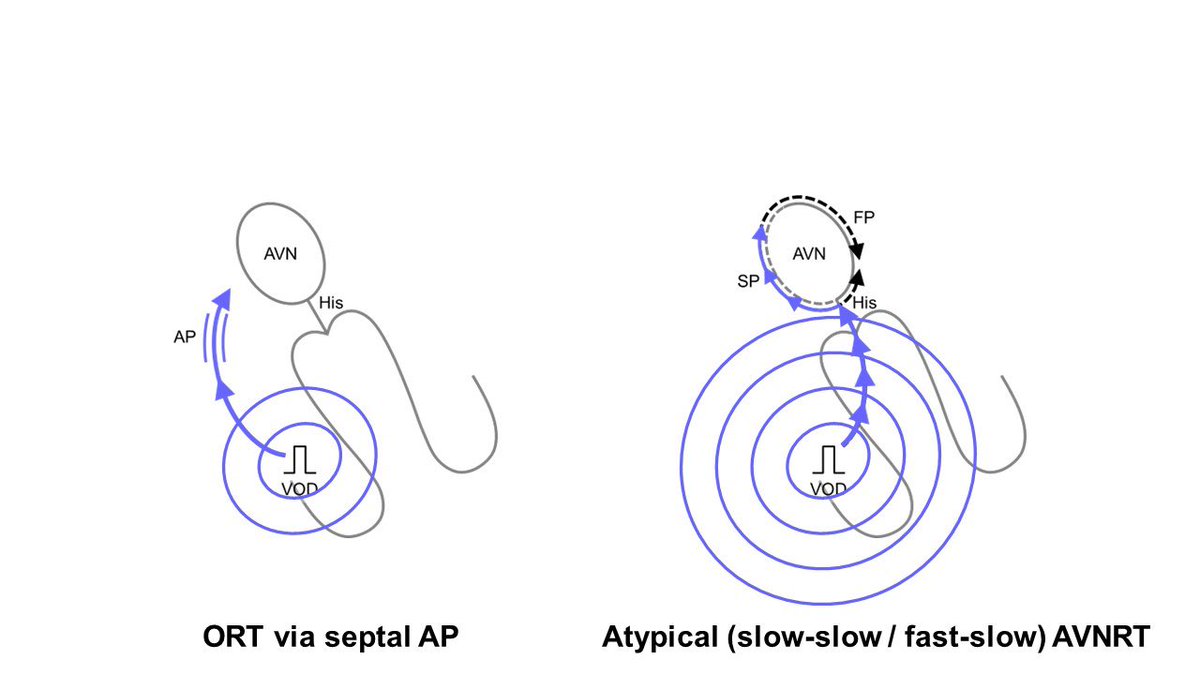
💡The most challenging differentiations include ORT with a septal AP and atypical AVNRT, because both show concentric atrial activation with an HA interval > 70 ms.
🚨Electrophysiologists need to be aware that because all current diagnostic maneuvers are designed to distinguish ORT from AVNRT, there’s a small risk of underdiagnosing ORT even if a maneuver yields a negative result. It's crucial to recognize that AVNRT can only be ultimately diagnosed after excluding ORT using all diagnostic criteria.
Organizing these maneuvers in chronological order makes it easier to understand their benefits, significance, and limitations.
#EPUniversity
#SVTquest
After ruling out AT, the next step is to differentiate between ORT and AVNRT.
💡The most challenging differentiations include ORT with a septal AP and atypical AVNRT, because both show concentric atrial activation with an HA interval > 70 ms.
🚨Electrophysiologists need to be aware that because all current diagnostic maneuvers are designed to distinguish ORT from AVNRT, there’s a small risk of underdiagnosing ORT even if a maneuver yields a negative result. It's crucial to recognize that AVNRT can only be ultimately diagnosed after excluding ORT using all diagnostic criteria.
Organizing these maneuvers in chronological order makes it easier to understand their benefits, significance, and limitations.
#EPUniversity
#SVTquest
✅His-refractory PVC
This maneuver was originally introduced by Wellens in 1967.
✅A single RV extrastimulus is delivered, and the coupling interval is systematically reduced by 5-10 ms until the pacing spike either overlaps or precedes the His potential by 20-25 ms.
✅If tachycardia is reset ≥10 ms following pacing, regardless of whether it is advanced or delayed, is diagnostic for ORT.
Similarly, ORT is diagnosed if tachycardia terminated without atrial capture, as this suggests a conduction block over the AP.
Conversely, AVNRT can’t be reset by His-refractory PVC.
🚨🚨However, the interpretation becomes more complicated once nodoventricular pathway (NVP)-related tachycardia is widely recognized. A reset by His-refractory PVC does not necessarily indicate ORT but merely suggests the presence of an AP, because AVNRT with a bystander NVP can also be reset by His-refractory PVC. Tachycardia can be reset or terminated without atrial capture, even just one cycle after a His-refractory PVC. This phenomenon is specifically diagnostic of AVNRT when a bystander cNVP is present, which will be posted later.
#EPUniversity
#SVTquestahajournals.org/doi/epdf/10.11…
This maneuver was originally introduced by Wellens in 1967.
✅A single RV extrastimulus is delivered, and the coupling interval is systematically reduced by 5-10 ms until the pacing spike either overlaps or precedes the His potential by 20-25 ms.
✅If tachycardia is reset ≥10 ms following pacing, regardless of whether it is advanced or delayed, is diagnostic for ORT.
Similarly, ORT is diagnosed if tachycardia terminated without atrial capture, as this suggests a conduction block over the AP.
Conversely, AVNRT can’t be reset by His-refractory PVC.
🚨🚨However, the interpretation becomes more complicated once nodoventricular pathway (NVP)-related tachycardia is widely recognized. A reset by His-refractory PVC does not necessarily indicate ORT but merely suggests the presence of an AP, because AVNRT with a bystander NVP can also be reset by His-refractory PVC. Tachycardia can be reset or terminated without atrial capture, even just one cycle after a His-refractory PVC. This phenomenon is specifically diagnostic of AVNRT when a bystander cNVP is present, which will be posted later.
#EPUniversity
#SVTquestahajournals.org/doi/epdf/10.11…
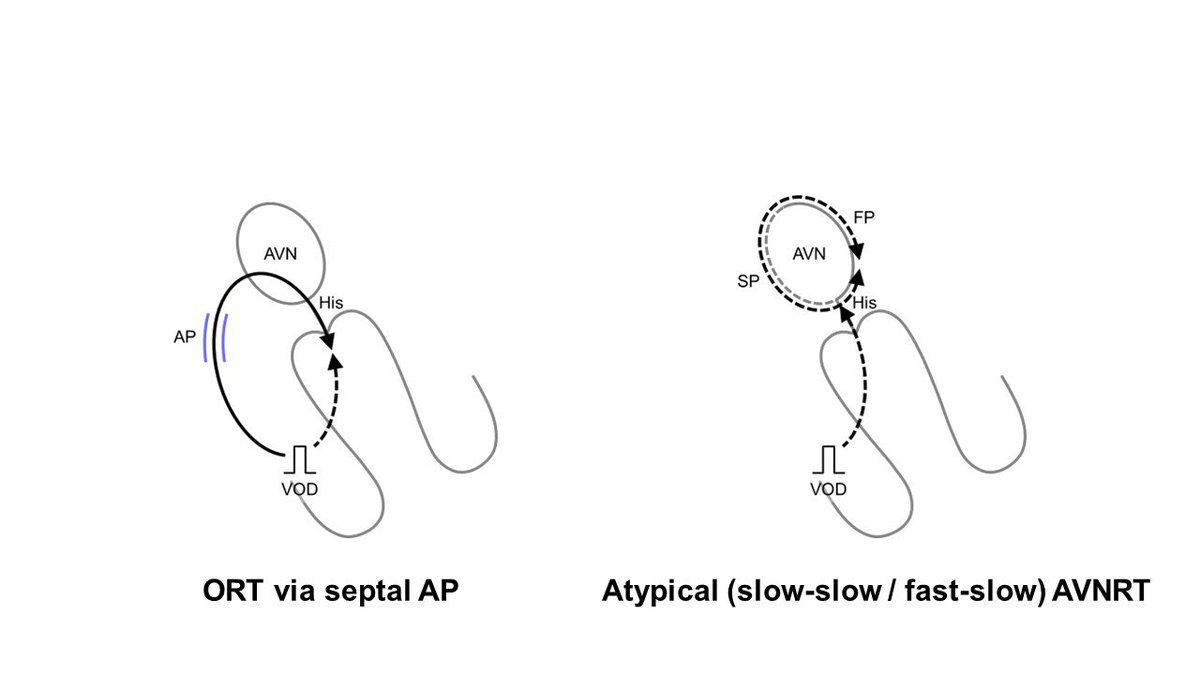
✅PPI – TCL, SA – VA
🚨The assessment of His-refractory PVC for SVT with wobbling TCL is tricky😰
✅Recognizing these challenges, Greg Michaud @DrGregMichaud pioneered VOD-based diagnostic maneuvers.
PPI – TCL represents twice the conduction time through the RV pacing site and the SVT circuit.
💡A cut-off value of PPI – TCL ≤ 115 ms clearly identifies ORT from AVNRT, given the larger size of the ORT circuit involving both A and V, and its proximity to the pacing site compared to the AVNRT circuit, which is confined to AVN.
💡Similarly, SA – VA ≤ 85 ms distinguishes ORT from AVNRT. SA interval was determined by measuring from the last pacing spike to the last captured HRA-EGM during VOD, while the VA interval was gauged from the onset of the QRS to the HRA.
🥰The most impressive aspect of this study is the patient selection. It focused exclusively on patients with concerning septal ORT and atypical AVNRT, excluding those with free wall AP and typical slow-fast AVNRT. This attitude is super cooool😍
#EPUniversity
#SVTquest
sciencedirect.com/science/articl…

🚨The assessment of His-refractory PVC for SVT with wobbling TCL is tricky😰
✅Recognizing these challenges, Greg Michaud @DrGregMichaud pioneered VOD-based diagnostic maneuvers.
PPI – TCL represents twice the conduction time through the RV pacing site and the SVT circuit.
💡A cut-off value of PPI – TCL ≤ 115 ms clearly identifies ORT from AVNRT, given the larger size of the ORT circuit involving both A and V, and its proximity to the pacing site compared to the AVNRT circuit, which is confined to AVN.
💡Similarly, SA – VA ≤ 85 ms distinguishes ORT from AVNRT. SA interval was determined by measuring from the last pacing spike to the last captured HRA-EGM during VOD, while the VA interval was gauged from the onset of the QRS to the HRA.
🥰The most impressive aspect of this study is the patient selection. It focused exclusively on patients with concerning septal ORT and atypical AVNRT, excluding those with free wall AP and typical slow-fast AVNRT. This attitude is super cooool😍
#EPUniversity
#SVTquest
sciencedirect.com/science/articl…

✅Corrected PPI – TCL
🚨The PPI–TCL looks an excellent tool for differentiating ORT from AVNRT, but it has significant limitations; the PCL must be set 10-30 ms shorter than the TCL to entrain the SVT circuit. Therefore, PPI may be prolonged due to decremental conduction over the AVN, posing a risk of underdiagnosing ORT due to a prolonged PPI.
💡To overcome this challenge, González-Torrecilla introduced corrected PPI–TCL, compensating for the delay in AVN conduction during VOD.
📝In practice, this delay can be calculated by taking the post-pacing AH interval—measured from the last captured beat at the HRA to the His in the first return beat after VOD—and subtracting the AH interval during the tachycardia.
📝While the uncorrected PPI–TCL and SA–VA present overlaps among septal ORT and AVNRT, a corrected PPI–TCL ≤110 ms effectively distinguishes ORT from AVNRT.
🔥However, this correction is needed only when the PPI–TCL is >115 ms to avoid the underdiagnosis of ORT. Correction is unnecessary when PPI–TCL is ≤115 ms, as in these cases, the PPI–TCL alone can accurately diagnose ORT.
#EPUniversity
#SVTquest
💕Reference
heartrhythmjournal.com/article/S1547-…
🚨The PPI–TCL looks an excellent tool for differentiating ORT from AVNRT, but it has significant limitations; the PCL must be set 10-30 ms shorter than the TCL to entrain the SVT circuit. Therefore, PPI may be prolonged due to decremental conduction over the AVN, posing a risk of underdiagnosing ORT due to a prolonged PPI.
💡To overcome this challenge, González-Torrecilla introduced corrected PPI–TCL, compensating for the delay in AVN conduction during VOD.
📝In practice, this delay can be calculated by taking the post-pacing AH interval—measured from the last captured beat at the HRA to the His in the first return beat after VOD—and subtracting the AH interval during the tachycardia.
📝While the uncorrected PPI–TCL and SA–VA present overlaps among septal ORT and AVNRT, a corrected PPI–TCL ≤110 ms effectively distinguishes ORT from AVNRT.
🔥However, this correction is needed only when the PPI–TCL is >115 ms to avoid the underdiagnosis of ORT. Correction is unnecessary when PPI–TCL is ≤115 ms, as in these cases, the PPI–TCL alone can accurately diagnose ORT.
#EPUniversity
#SVTquest
💕Reference
heartrhythmjournal.com/article/S1547-…
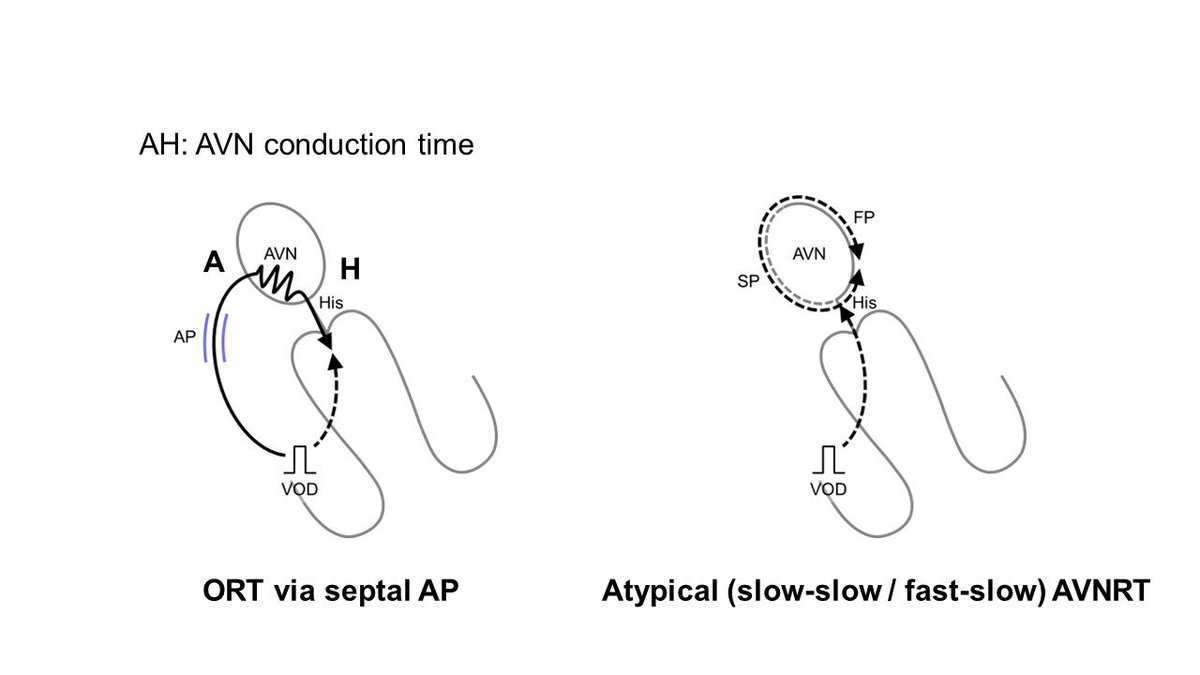
✅Orthodromic His Capture
🚨The corrected PPI–TCL looks excellent but still has significant limitations. Decremental conduction is not limited to the AVN; it can also occur in septal APs. This may lead to a prolonged PPI due to decremental conduction through the septal AP, even after the AH correction, thereby increasing the risk of missing ORT diagnoses.
🔥To overcome these measurement-based limitations, Greg and I focused on the direction of His bundle activation during VOD. During VOD, the His bundle and/or ventricular septum might activate anterogradely, indicating orthodromic capture of the His/ventricular septum.
💡This observation is explained by the orthodromic wavefront conducting retrogradely through the AP and then anterogradely through the AVN and His, where it collides with the antidromic wavefront from the subsequent pacing cycle. Stable fusion below the His, marked by consistent QRS fusion, occurs. Upon cessation of pacing, the His is activated next at the PCL, driven by the last-paced wavefront traveling retrogradely through the pathway and anterogradely through the AVN.
📝This maneuver allows for a straightforward and rapid assessment, as orthodromic His/septal ventricular capture can be determined by measuring from the His bundle or ventricular electrogram back an interval equal to the PCL. Identification of the preceding His bundle or ventricular EGM at this interval indicates orthodromic capture.
📝Conversely, in AVNRT, the His bundle is always activated retrogradely (antidromic His capture) to entrain the AVN circuit. Thus, no His signal is observed at this interval.
🔥This maneuver accurately diagnoses ORT in 60% of cases via a slowly conducting AP.
#EPUniversity
#SVTquest
heartrhythmjournal.com/article/S1547-…
🚨The corrected PPI–TCL looks excellent but still has significant limitations. Decremental conduction is not limited to the AVN; it can also occur in septal APs. This may lead to a prolonged PPI due to decremental conduction through the septal AP, even after the AH correction, thereby increasing the risk of missing ORT diagnoses.
🔥To overcome these measurement-based limitations, Greg and I focused on the direction of His bundle activation during VOD. During VOD, the His bundle and/or ventricular septum might activate anterogradely, indicating orthodromic capture of the His/ventricular septum.
💡This observation is explained by the orthodromic wavefront conducting retrogradely through the AP and then anterogradely through the AVN and His, where it collides with the antidromic wavefront from the subsequent pacing cycle. Stable fusion below the His, marked by consistent QRS fusion, occurs. Upon cessation of pacing, the His is activated next at the PCL, driven by the last-paced wavefront traveling retrogradely through the pathway and anterogradely through the AVN.
📝This maneuver allows for a straightforward and rapid assessment, as orthodromic His/septal ventricular capture can be determined by measuring from the His bundle or ventricular electrogram back an interval equal to the PCL. Identification of the preceding His bundle or ventricular EGM at this interval indicates orthodromic capture.
📝Conversely, in AVNRT, the His bundle is always activated retrogradely (antidromic His capture) to entrain the AVN circuit. Thus, no His signal is observed at this interval.
🔥This maneuver accurately diagnoses ORT in 60% of cases via a slowly conducting AP.
#EPUniversity
#SVTquest
heartrhythmjournal.com/article/S1547-…
✅Transition Zone Analysis
🚨Another challenge with VOP is tachycardia termination, which can make the assessment tricky.
💡AlMahameed and Greg Michaud came up with a method that focuses on starting the VOP. The principle is similar to resetting ORT with His-refractory PVCs.
📝In ORT, the VOD can capture the atrium in the early phase, where the paced complexes show progressive QRS fusion up to the first paced complex with stable QRS morphology, defined as the "transition zone."
In 94% of ORTs, the atrium is reset, like either an earlier or later atrial timing of ≥15 ms, or VA block in the transition zone. Meanwhile, in 97% of ORT cases, the SA interval locks to the PCL, with variations of <10 ms during the transition zone.
All ORTs show either atrial resetting or a stable SA interval.
📝On the flip side, in AVNRT, atrial resetting and a stable SA interval manifest after the transition zone.
🌸The greatest advantage of this maneuver is the feasibility of the assessment regardless of tachycardia termination during the VOP.
🚨However, the assessment based on a 12-lead ECG is somewhat time-consuming and lacks objectivity. Also, a pitfall is that this analysis doesn't work well when the atrial resetting occurs in the last beat of the transition zone (=the first beat with a stable QRS), since this could occur in either ORT or AVNRT.
Reference
#EPUniversity
#SVTquestahajournals.org/doi/10.1161/CI…
🚨Another challenge with VOP is tachycardia termination, which can make the assessment tricky.
💡AlMahameed and Greg Michaud came up with a method that focuses on starting the VOP. The principle is similar to resetting ORT with His-refractory PVCs.
📝In ORT, the VOD can capture the atrium in the early phase, where the paced complexes show progressive QRS fusion up to the first paced complex with stable QRS morphology, defined as the "transition zone."
In 94% of ORTs, the atrium is reset, like either an earlier or later atrial timing of ≥15 ms, or VA block in the transition zone. Meanwhile, in 97% of ORT cases, the SA interval locks to the PCL, with variations of <10 ms during the transition zone.
All ORTs show either atrial resetting or a stable SA interval.
📝On the flip side, in AVNRT, atrial resetting and a stable SA interval manifest after the transition zone.
🌸The greatest advantage of this maneuver is the feasibility of the assessment regardless of tachycardia termination during the VOP.
🚨However, the assessment based on a 12-lead ECG is somewhat time-consuming and lacks objectivity. Also, a pitfall is that this analysis doesn't work well when the atrial resetting occurs in the last beat of the transition zone (=the first beat with a stable QRS), since this could occur in either ORT or AVNRT.
Reference
#EPUniversity
#SVTquestahajournals.org/doi/10.1161/CI…
• • •
Missing some Tweet in this thread? You can try to
force a refresh




