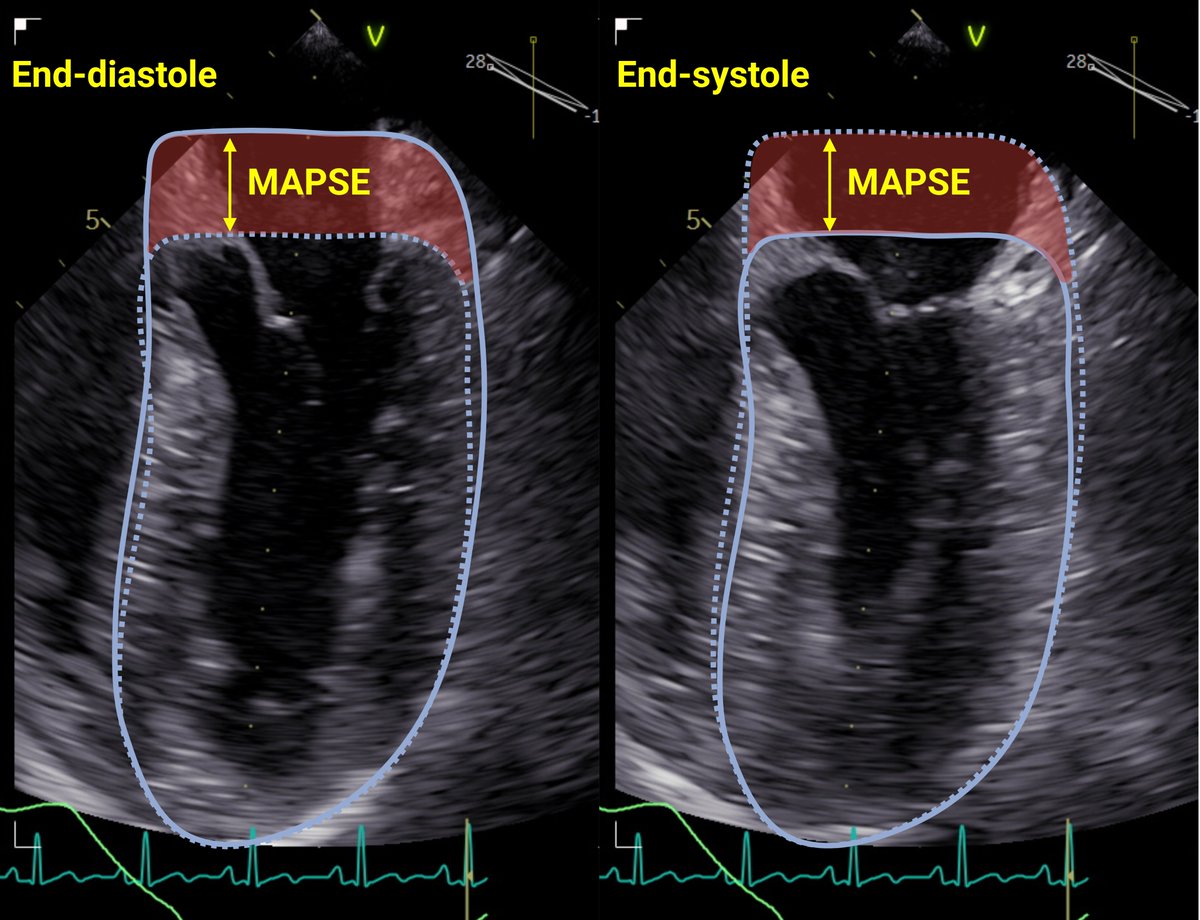
🧵1/ #AutoMAPSE had high feasibility for estimating MAPSE from ≥1⃣wall. Many worry that #MAPSE is limited by RWMA, such as acute MI - however, evidence suggests that regional MAPSE reflects global LV function.
#EchoFirst #POCUS #FOAMed #CardioTwitter rdcu.be/dHLxx
#EchoFirst #POCUS #FOAMed #CardioTwitter rdcu.be/dHLxx
2/ Several studies have shown that in AMI, MAPSE is ⬇️even in walls remote to MI. This was confirmed experimentally by Berg et al, in an experiment occluding the LAD in pigs and measuring #MAPSE by #WhyCMR.
First paper:
Berg et al: doi.org/10.1080/140174…
doi.org/10.1152/japplp…

First paper:
Berg et al: doi.org/10.1080/140174…
doi.org/10.1152/japplp…

3/ ⬇️MAPSE in remote walls is explained through the distribution of afterload. For a specific region to shorten, that region must overcome the opposing afterload imposed by its neighboring region, which is shortening in the opposite direction.
4/ Thus, if a region is not shortening (yellow segment), its neighboring region (red segment) has less opposing afterload and will shorten MORE. However.....
Figure from @strain_rate
Figure from @strain_rate

5/ ...the total afterload is only redistributed, and not changed: ⬇️myocardium must now overcome the total afterload. Therefore, remote regions (orange segments) experience ⬆️afterload and therefore shorten less.
Figure from @strain_rate
Figure from @strain_rate

6/ The total shortening is translated to the mitral annulus because all the walls are tethered to the mitral annulus. Thus, regional function from any wall affect #MAPSE of any other walls, and MAPSE = global LV function.
Fig from: folk.ntnu.no/stoylen/strain…

Fig from: folk.ntnu.no/stoylen/strain…

7/ This suggests that changes in regional MAPSE reflect changes in global LV function. Good for #AutoMAPSE! However, it also means that regional #MAPSE cannot detect regional dysfunction such as ischemia.
Fig shows the feasibility of #AutoMAPSE: rdcu.be/dHLxx

Fig shows the feasibility of #AutoMAPSE: rdcu.be/dHLxx

8/ This is also good news for #MAPSE using #POCUS. MAPSE from one wall is faster, simpler, and highly feasible in poor images. Also, several beats can easily be averaged, increasing the precision needed for monitoring by #EchoFirst.
end 🧵

end 🧵
https://twitter.com/dritsyk/status/1751654442414276705

unroll @threadreaderapp
• • •
Missing some Tweet in this thread? You can try to
force a refresh