1/3
THROMBOCYTOPENIA (TP) IN SEPSIS
1. Thrombocytopenia occurs in about 50% of patients in the ICU.
2. Sepsis accounts for approximately 50% of all thrombocytopenia in the severely ill.
3. Platelet count is included in the SOFA score.
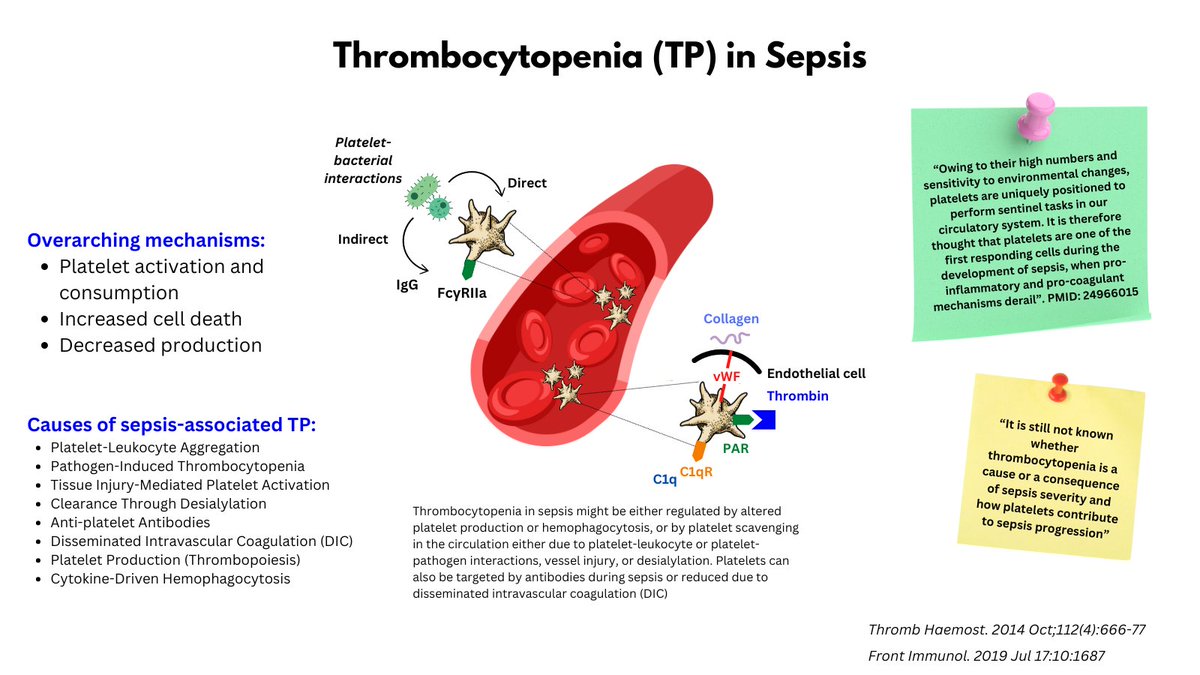
THROMBOCYTOPENIA (TP) IN SEPSIS
1. Thrombocytopenia occurs in about 50% of patients in the ICU.
2. Sepsis accounts for approximately 50% of all thrombocytopenia in the severely ill.
3. Platelet count is included in the SOFA score.
2/3
4. Platelet count is inversely associated with sepsis severity and mortality.
5. Mechanisms of thrombocytopenia in sepsis include:
-- a) Increased activation/consumption
-- b) Increased apoptosis
-- c) Decreased platelet production (uncommon)
4. Platelet count is inversely associated with sepsis severity and mortality.
5. Mechanisms of thrombocytopenia in sepsis include:
-- a) Increased activation/consumption
-- b) Increased apoptosis
-- c) Decreased platelet production (uncommon)
3/3
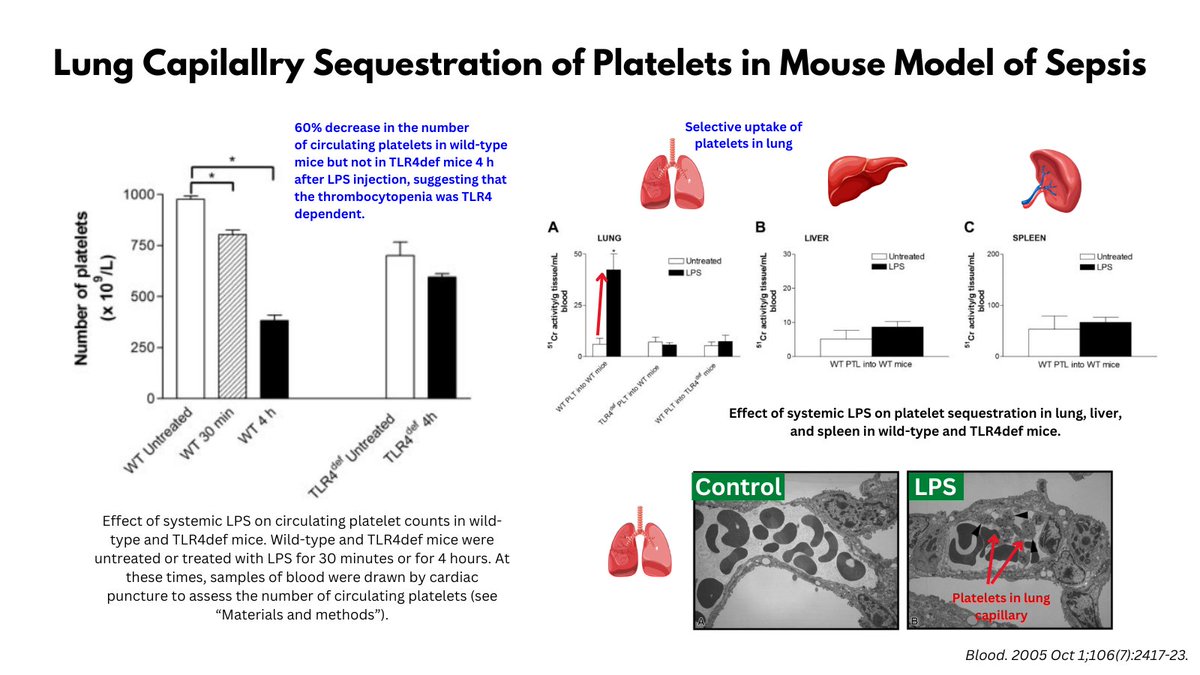
One of my favorite studies exploring mechanisms of sepsis-associated TP showed that injection of endotoxin in wild-type and TRL4 null. mice resulted in massive sequestration of platelets in the pulmonary microcirculation in WT, but not TRL4-deficient animals (graphic).
One of my favorite studies exploring mechanisms of sepsis-associated TP showed that injection of endotoxin in wild-type and TRL4 null. mice resulted in massive sequestration of platelets in the pulmonary microcirculation in WT, but not TRL4-deficient animals (graphic).
• • •
Missing some Tweet in this thread? You can try to
force a refresh