It’s out! Our new state-of-the-science review of MASKS/RESPIRATORS in reducing transmission of respiratory infections. 13 authors (for our disciplines, see posts 3-4). 38000 words. 413 references. One conclusion: these devices work. For detail, read on. 1/
journals.asm.org/doi/10.1128/cm…
journals.asm.org/doi/10.1128/cm…
The commissioned review, which was independently peer-reviewed, had 3 objectives: 1. Summarize the evidence on masks/masking. 2. Examine why this evidence is so widely misunderstood, misinterpreted, or dismissed. 3. Outline an agenda for future research. 2/
Author team was chosen for breadth of expertise, including: public health, epidemiology, infectious diseases, biosecurity, fluid dynamics, materials science, mathematical modeling, data science, clinical trials, sociology, anthropology, psychology, and occupational hygiene. 3/
Author team, which includes @DALupton @DFisman @AmandaKvalsvig @globalbiosec @ShovonBhattach2 @joevipond and others from @kirbyinstitute @mark_ungrin @sameo416, also had expertise in multiple kinds of evidence synthesis, including statistical meta-analysis. 4/
@DALupton @DFisman @AmandaKvalsvig @Globalbiosec @ShovonBhattach2 @joevipond @KirbyInstitute @Mark_Ungrin @sameo416 Study protocol for this narrative review with embedded meta-analysis was registered on INPLASY: 5/inplasy.com/inplasy-2024-1…
@DALupton @DFisman @AmandaKvalsvig @Globalbiosec @ShovonBhattach2 @joevipond @KirbyInstitute @Mark_Ungrin @sameo416 We searched extensively for high-quality evidence in all fields. We did NOT assume that all RCT evidence was “gold standard”, nor that all non-RCT evidence was “low-quality”. Indeed, we questioned whether the RCT deserves its hallowed status in this field. 6/ 

@DALupton @DFisman @AmandaKvalsvig @Globalbiosec @ShovonBhattach2 @joevipond @KirbyInstitute @Mark_Ungrin @sameo416 We covered evidence across a vast range of disciplines and study designs, including but not limited to: laboratory studies, RCTs, observational studies, modelling studies, social and psychological studies, surveys, policy analyses, environmental impact studies. 7/
@DALupton @DFisman @AmandaKvalsvig @Globalbiosec @ShovonBhattach2 @joevipond @KirbyInstitute @Mark_Ungrin @sameo416 We went through the basic science showing that SARS-CoV-2, like other respiratory infections, is transmitted via the air. We criticised EPISTEMIC TRESPASSING by infection prevention & control (IPC) physicians, who drew wrong conclusions from their own flawed experiments. 8/ 

@DALupton @DFisman @AmandaKvalsvig @Globalbiosec @ShovonBhattach2 @joevipond @KirbyInstitute @Mark_Ungrin @sameo416 We carefully traced the origins of the widely-propagated “droplet hypothesis”, in which it is assumed that large droplets somehow get deep into the lungs on some kind of ballistic trajectory (tip: they don’t). 9/ 

@DALupton @DFisman @AmandaKvalsvig @Globalbiosec @ShovonBhattach2 @joevipond @KirbyInstitute @Mark_Ungrin @sameo416 Why does this matter? Because IF the droplet hypothesis were correct (TL;DR: it’s not), all we’d need is one of those baggy, waterproof-backed ‘medical masks’ designed to stop the surgeon sneezing into the patient’s open abdomen or getting a mouthful when an abscess bursts. 10/
But because respiratory infections transmit via TINY PARTICLES SUSPENDED IN THE AIR, waterproof-backed medical masks are NOT the best way to stop them. Starting from first principles, what we need is something that EFFICIENTLY REMOVES PARTICLES FROM THE AIR. 11/
In other words, not all things you put over your face are equal! Here’s a few things to think about: 12/








Are you with me? There are good ways and bad ways of designing a mask! Ideally, you want one that's guaranteed HIGH-FILTRATION, LOW-RESISTANCE, WELL-FITTING and SUPER-CLEAN. Such a device is known as a RESPIRATOR. 2 examples shown: N95 (single-use) & elastomeric (reusable). 13/




Did we address the anti-maskers’ favourite argument that the holes in a mask filter are bigger than the SARS-CoV-2 virus? What do you think? Of course we did. MASK FILTERS ARE NOT SIMPLE SIEVES! 14/ 
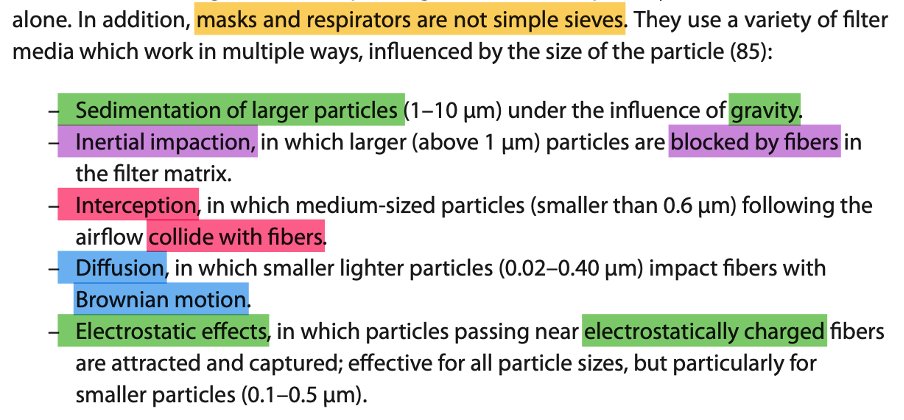
Here’s a nice diagram. Each little square is a different laboratory study. ‘Filtering facepiece’ means RESPIRATOR. ‘Community mask’ means one you made at home (from cloth). ‘Protection factor’ (note: LOGARITHMIC scale) is how much it blocks bad particles (higher is good). 15/ 

The above diagram is from Schmidt & Wang’s paper on the CRITICAL ROLE OF LEAKAGES in mask malfunction. If air leaks out around the sidesless protection. We thank these authors for letting us reproduce it. 16/ onlinelibrary.wiley.com/doi/full/10.11…
Another leakage study. Up the side is LEAKAGE (more is bad). Along the bottom is particle size. Different colours represent different masks: GREEN = medical mask (very leaky), PURPLE = respirator sealed all around with tape to get perfect fit (nothing gets through it). 17/ 

Credit for the previous image: Bagheri et al’s GOLD STANDARD laboratory study, which you can admire in full text here. Thanks to them for permission to reproduce. 18/ pnas.org/doi/abs/10.107…
OK, we’re getting to the RCT section. And this is where the quality of much of the evidence plummets—partly because there’s some flaky trials out there and partly because even the BEST trials of masks are INHERENTLY problematic.19/




Most RCTs of masks didn’t use an optimally-designed device. Many didn’t measure whether the mask was worn (where compliance *was* measured, was low). These flaws are like doing a RCT of a blood pressure drug at 1/100th the correct dose. They BIAS THE RESULT TOWARDS THE NULL. 20/
Other common flaws in mask RCTs include lack of power, suboptimal outcome measures, telling participants to only mask SOME of the time, and doing the study when there are no infections circulating. Each of these slip-ups will tend to bias results towards null. 21/
Small wonder, then, that most RCTs of masks in community or in healthcare settings produced no statistically significant difference between the ‘mask’ arm (actually, the “advice to slap a poorly-designed medical mask on if you feel inclined” arm) and the ‘no mask’ arm. 22/
The one adequately-powered RCT of community masking in the entire sample (which cluster-randomised villages in Bangladesh), by Abaluck et al, showed a statistically significant effect in favour of masks even though compliance was low. 23/ science.org/doi/full/10.11…
Let’s talk about RCTs of masks v respirators in healthcare. The research q here is of the utmost importance. Should we protect our staff with the kind of device that produced the purple line in post 17 above? Or should they get the device that produced the green (leaky) line? 24/
Here’s where the study designs go embarrassingly off. Because many IPC doctors falsely believe the droplet hypothesis (see post 9), their prior belief (which influences the intervention design) is that medical masks are as good as anything else so long as you wash your hands. 25/
IPC docs may also believe that infectious aerosols are produced by a patient only when they’re having a fancy procedure done to them by a doctor (hence ‘aerosol-generating medical procedure’ AGMP). (You’re right, it does rather smack of infantile omnipotence) 26/
In fact, patients infected with SARS-CoV-2 (or SARS-1 or MERS or influenza or measles or TB) emit infectious particles in the air by COUGHING and SPEAKING and even BREATHING. And those particles quickly spread THROUGHOUT THE INDOOR SPACE. 27/
Hence, any trial of masks v respirators in a healthcare setting MUST require the devices to be worn CONTNUOUSLY WHEN INDOORS. If higher-grade protection is worn only when close to a known ‘case’ or when doing an AGMP, it’s likely to be as good as a chocolate teapot. 28/
We meta-analysed mask-v-respirator trials in healthcare settings in 2 ways. First, lumping all trials together (result: respirators outperform masks *a bit*). Second, using only RCTs testing CONTINUOUS USE OF RESPIRATORS. Result: respirators outperform masks *significantly*. 29/
Acknowledging the limitations of observational evidence, we identified and summarised LOTS of observational studies and natural experiments. All studies pointed in the same direction: in favour of the kinds of effect you’d predict from basic science. 30/
pubmed.ncbi.nlm.nih.gov/34783656/#:~:t…
pubmed.ncbi.nlm.nih.gov/34783656/#:~:t…
Likewise with mathematical modelling studies (of which there are various kinds). In sum, the non-RCT evidence – rather surprisingly and very consistently – stacks up in favour of masks (and of respirators as even better). 31/ 

HARMS of masks. Three kinds: 1. Complete fictions (things the anti-maskers make up, like accumulation of poisonous CO2 in your body—it doesn’t happen). 2. Minor hazards (headaches, acne), which may be worth the trade-off. 3. Specific exemption conditions (see pic). 32/ 

When OTHERS are masked, there may be communication problems, especially for D/deaf people. One of our authors, @AmandaKvalsvig, is hearing-impaired. She wrote: it MAY NOT be in a deaf person’s interests if others remove their masks! (It may, but need to WEIGH UP RISKS). 33/
We need better communication strategies that can be employed if mass masking needs to be introduced again. We talk about some avenues for this in the paper (e.g. lapel mics so we don’t tire out our voices). More research needed on these! 34/
WHY DO PEOPLE MASK (and why do some REFUSE TO MASK)? Answer: for lots of psychological, cultural, ideological and social reasons, as @DAlupton says in her section. 35/




Misleading messages from leading public health agencies contributed to confusion about masks and about the relative benefits of respirators versus medical masks. 36/ 

Mask POLICIES involve strongly recommending and even mandating the wearing of masks in certain settings. We do a long section on this. Policymakers need to ASSESS THE RISKS, BALANCE THE TRADE-OFFS and SUPPORT THE POLICY (e.g. by giving them away). 37/
Single-use masks and respirators are not good for the planet. It’s time we moved to a more sustainable approach. Re-usable, recyclable and biodegradable devices exist. DID YOU KNOW that you can recycle chopped-up masks to make building materials like concrete? 38/
Time for conclusions. First, MASKS WORK!!! And we’ve explained why some people insist that they don’t! Read the yellow bit out loud please. 39/ 

Second conclusion. It’s time to REMOVE PEOPLE WHO CAN’T OR WON’T UNDERSTAND THE EVIDENCE ON MASKING FROM KEY DECISION-MAKING COMMITTEES. Who will be brave and make that move? Lives depend on it. 40/ 

Third conclusion. Mask policies should be based on ACTUAL risks, not SPECULATIVE ones. And masks, overall, should be better designed to REDUCE the minor side effects like hot face. 41/ 

Fourth conclusion. Talking of design, we need CREATIVE DESIGNS to suit EVERYONE, not just your standard crash-dummy white 70Kg clean-shaven male. 42/ 

Final conclusion: anti-mask disinformation is as dangerous as anti-vax disinformation. We need to systematically counter it. 44/ 

BOTTOM LINE: We don’t need any more masks-on v masks-off RCTs. That’s for dobbins. We need a NEW GENERATION of research which takes as its starting point the VAST EXISTING EVIDENCE BASE on the efficacy of masks and respirators. Then this: 45/ 

If you like this thread, please hit the retweet button! Thanks to @DALupton @DFisman @AmandaKvalsvig @globalbiosec @ShovonBhattach2 @joevipond and others from @kirbyinstitute @mark_ungrin @sameo416. 46/
@DALupton @DFisman @AmandaKvalsvig @Globalbiosec @ShovonBhattach2 @joevipond @KirbyInstitute @Mark_Ungrin @sameo416 And here’s the pice on my Departmental website 47/phc.ox.ac.uk/news/comprehen…
@DALupton @DFisman @AmandaKvalsvig @Globalbiosec @ShovonBhattach2 @joevipond @KirbyInstitute @Mark_Ungrin @sameo416 And here's our piece for The Conversation - also just out (you can syndicate): 48/
theconversation.com/masks-work-our…
theconversation.com/masks-work-our…
• • •
Missing some Tweet in this thread? You can try to
force a refresh